Reporte de caso
← vista completaPublicado el 24 de agosto de 2016 | http://doi.org/10.5867/medwave.2016.07.6524
Carcinoma anexial de células germinales con metástasis ósea en gestante: reporte de un caso y revisión
Adnexal germ cell carcinoma with bone metastases in pregnant women: case report and review
Abstract
Germ cell carcinoma during pregnancy is rare. However, its detection has increased due to the use of ultrasound fetal monitoring in the antenatal care program. In this article, we present the case of a Germ cell carcinoma during pregnancy is rare. However, its detection has increased due to the use of ultrasound fetal monitoring in the antenatal care program. In this article, we present the case of a pregnant 27-year-old diagnosed with an adnexal germ cell carcinoma at six weeks of gestation, whose initial approach was local resection (suboptimal cytoreduction). Four weeks after surgery, the patient presented with grade IV peripheral neuropathy in the lower limbs; magnetic resonance imaging scan indicated an infiltrative lesion at D5. The local medical board decided on chemotherapy starting on the 19th week of gestation. The rest of the pregnancy period was uneventful and the patient had a cesarean section at 34 weeks of gestation and a live newborn with no complications. Unfortunately, four days after caesarean section, the patient died of a septic shock with respiratory focus.
Introduction
The use of ultrasound for fetal assessment has enabled to increase the detection of asymptomatic adnexal masses. [1] These occur in 0.2 to 2% of pregnancies. Most are benign (teratomas and cistoadenomas) and revert spontaneously, becoming undetectable at week 14 [2]. Of the total adnexal masses, only 1 to 6% are malignant (one of 10,000 pregnant women), the second most common in pregnant women after cervical cancer [1],[3]. Between all adnexal tumors in pregnancy, 40% correspond to germ cell tumors. Of these tumors, about 15 to 20% are dysgerminomas [4].The potential for malignancy in these tumors is low. However, it represents a serious difficulty in handling during pregnancy due to the imminent risk of fetal harm. Currently, due to the limited information available, the management options for these patients are diverse. Intervention can just be surgical in cases where suspected to confirm malignancy, or it can be chemotherapy or adjuvant radiotherapy [3],[5]. The surgical management of a neoplasia is standard regardless if the patient is gestating or not, but use of adjuvant or palliative chemotherapy depends on the stage and the presence or absence of metastasis. Also, use of the latter will depend on the agent and the gestational age; between four and 12 weeks old there is a greater risk of teratogenicity [3].
Case description
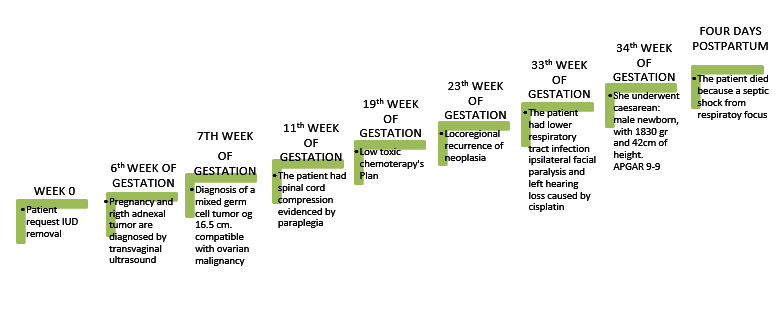
Female patient, 27 years old who came to outpatient gynecology department of a general hospital, requesting the removal of intrauterine device because of the desire of conception. After the procedure, the patient presented with diffuse abdominal pain in lower abdomen, so she was readmitted to the hospital where she underwent a transvaginal ultrasound. It was evident a gestation of six weeks, associated with right adnexal tumor of 127X88 millimeters in diameter. The values α fetoprotein and lactic dehydrogenase were over 1000 IU / ml (normal value ≤10 IU / ml) and 825 U / L (normal value = 50-150 U / L), respectively. In the week subsequent to transvaginal ultrasound, the patient presented exacerbation of abdominal pain. For this reason she was transferred to the emergency service of a level III hospital, where she was admitted with the diagnosis of acute surgical abdomen, undergoing laparoscopic explorative surgery. During surgery, a bleeding tumor was observed with peritoneal commitment in the right annex. The only procedure conducted was a right salpingo-oophorectomy (suboptimal cytoreduction because of pregnancy, sending the surgical specimen to pathology. This pathology study was conclusive, with a germinal mixed cell tumor (98% endodermal sinus tumor and 2% endodermal dysgerminoma) of high histological grade, and 16.5 centimeters long, compatible with ovarian malignancy.
After four weeks, the patient presented paraparesis that evolved rapidly to paraplegia. Hospitalization was decided with diagnosis of spinal cord compression. She underwent a spine magnetic resonance imaging scan, showing a paraspinal infiltrative lesion at D5 with involvement of the spinal canal. The evaluation of neurosurgery ruled out the surgical possibility due to spinal cord injury already established.
A medical board was held between the services of gynecology, neurosurgery, neonatology and oncology at which it was decided that the ideal therapeutic approach for the patient at that time, was chemotherapy with a low toxic potential scheme for the fetus.
At all times, the patient was informed about the therapeutic possibilities, potential consequences and risks for her and the fetus. Fetal viability was measured by serial ultrasound tests and staging of metastatic disease was tested through imaging controls, with the intent to evaluate the ideal delivery time.
Systemic chemotherapy began in week 19 of gestation. As a complication of treatment with cytostatics, the patient presented febrile neutropenia grade IV due to Escherichia coli ESBL from urinal focus, which conditioned multiple hospital readmissions. After four weeks of chemotherapy, locoregional recurrence of the tumor is observed.
The patient continued with chemotherapy regularly. At 33 weeks of gestation, she presented fever associated with low back pain, so she went to the emergency service where she was hospitalized. In this period, a lower respiratory tract infection was found, which was treated with antibiotics (Cefepime) having favorable clinical evolution. Concomitant with infection, she coursed with a left facial palsy (peripheral) associated with ipsilateral hearing loss, probably secondary to the use of cisplatin. A caesarean section was carried out at 34 weeks of gestation, resulting in a male live birth, weighing 1,830 grams, size 42 centimeters and a 9-9 Apgar test. Four days after caesarean section, the patient presented septic shock from respiratory focus, and died as a result.
 Full size
Full size Discussion
The coexistence of pelvic malignancies and pregnancy is very rare. For this reason the information on the subject is limited, making the management of these patients thoroughly discussed from a therapeutic point of view. Before the routine use of ultrasound techniques, most adnexal tumors were not recognized until delivery or until they became symptomatic [1]. Currently, they are diagnosed with ease during the first trimester. Their management depends on the risk of malignancy, which is very low in most cases [2].
Also, symptoms can be as subtle as a mild back pain, constipation or urinary symptoms, wrongly associated with pregnancy [6].
With regard to diagnosis, apart from physical examination, ultrasound remains the diagnostic method of choice for detecting adnexal masses. Ultrasound is the most accessible at all levels of care and the safest for the fetus. However, because ultrasound does not allow the assessment of tumor malignancy, if malignancy is suspected, nuclear magnetic resonance imaging is recommended to guide surgical treatment, thus allowing final histopathologic confirmation [1].
On the other hand, there are tumor markers such as CA 125, α-fetoprotein, and lactate dehydrogenase. All of them have high sensitivity, but low specificity for this type of neoplasia, given they are physiologically elevated during pregnancy [1].
Regarding the management of ovarian malignancies during pregnancy, expectant treatment ("wait and watch") in asymptomatic patients is the most currently accepted [2]. In another line, in symptomatic patients, the option is a conservative surgical treatment (suboptimal cytoreduction). Depending on the clinical stage, histological tumor characteristics, and general state of the mother, therapies such as radical surgery (optimal debulking), chemotherapy or adjuvant or palliative radiotherapy may be recommended [7].
Chemotherapeutic agents are in category D in pregnancy, being contraindicated in the first quarter since it has been demonstrated that fetal exposure at two to eight weeks is related to an increased incidence of stillbirth and malformations, the latter is not yet well clarified. For this reason, the suggestion is to wait until 14 weeks of gestation for initiating treatment with cytotoxic agents [6],[8]. Nevertheless, it is known that these drugs can cross the placental barrier during the following trimesters and alter cell division, generating growth retardation and prematurity, the main adverse effects of chemotherapeutic agents [8].
The case presented is a pregnant woman of 27 years with advanced disease at debut, subject to suboptimal debulking and rapid neurologic progression; even though a high percentage (60%) of malignant ovarian tumors diagnosed during pregnancy are in early stages. The average age of presentation of this type of tumor is under 40 years and with low grade of malignancy (well differentiated).
While it has been reported that most germ cell tumors (such as dysgerminomas or immature teratomas) have an excellent prognosis, in the case of our patient, the finding of a mixed line similar histological tumor but with high malignant potential, suggests that this association is unclear. In this regard, the need for studies or meta-analysis with more cases is proposed.
With regard to treatment, after receiving information about the risks and benefits, the patient agreed to undergo a multi-agent regime based on etoposide and cisplatin at 19 weeks of gestation. Thus, it applies to corroborate it with a retrospective study of twenty pregnant women with malignant ovarian tumors, diagnosed and treated in the Department of Oncology Gynecological Vali-e-Asr, Iran, in 1991 and 2002 [3]. In this study, data about treatment and monitoring verified that for these types of cancer, debulking surgeries must be applied timely. Postoperative adjuvant chemotherapy is also indicated, stressing, that it is contraindicated during the first quarter of pregnancy due to the high rate of abortion and abnormal fetal development. This treatment is recommended only in the second or third trimester, when the risk of congenital malformation of exposed fetuses is not greater than in the general population [3].
Similarly, in another review, five of seven patients matched with clinical signs of advanced disease (stages III-IV) and invasive histological lineage. These were considered as main poor prognostic factors that determined the low rate of overall survival; unlike five patients with tumors of low malignant potential who did not have evidence of disease at the end of follow up.
It should be emphasized that, although the course of pregnancy and caesarean delivery at 34 weeks continued without apparent neonatal complications, the evidence is still little with regard to the long-term cytotoxic chemotherapy consequences in this cancer during gestation. Furthermore, there is no convincing evidence of an increase in the number of malformations with the use of multiple cytostatic agents compared to treatment with one cytotoxic [3].
Conclusions
According to medical literature, the coincidence of a malignant adnexal mass and gestation has a variable incidence, with an average of 1 per 10,000 pregnancies [2]. While the risk of malignancy is relatively low, currently available diagnostic methods (ultrasound, magnetic resonance imaging), enable earlier diagnosis resulting in improved life expectancy for the mother and fetus. Treatment should be individualized and made in a multidisciplinary manner (medical oncologist, gynecologist-oncologist, radiation therapist, psychiatrist, neonatologist, among others). Although many chemotherapeutic agents are contraindicated during pregnancy, there are specific benefit-risk situations in which this treatment should be considered as it was the case of the patient presented here.
While there is no evidence of neonatal malformations associated with chemotherapy, close and regular checks to rule out future complications in early follow-up are suggested.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
Informed consent could not be applied in this patient. While at first, the patient verbally agreed to the preparation of this report from her case, sudden death, prevented signed consent. Our team does not have access to relatives, so they could not sign the informed consent. For this reason, in this manuscript, all data identifying the patient (such as name, ID number, and other identifiers) have been omitted.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated to Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that there was no funding coming from external sources.

