Reporte de caso
← vista completaPublicado el 17 de julio de 2017 | http://doi.org/10.5867/medwave.2017.06.7000
Embarazo ectópico abdominal secundario a perforación uterina por interrupción voluntaria del embarazo: presentación de caso
Ectopic abdominal pregnancy due to uterine perforation after an attempt to terminate pregnancy: a case presentation
Abstract
Secondary abdominal ectopic pregnancy is rare in clinical practice, but may lead to an increased maternal mortality. We present the case of a patient with an abdominal pregnancy secondary to a uterine perforation caused by a voluntary attempt to interrupt pregnancy that presented with nine weeks of abdominal pain and minimal vaginal bleeding which was mistakenly diagnosed as acute pelvic inflammatory disease, urinary tract infection, and post-abortion products of conception. Finally, the abdominal ultrasound test found an abdominal ectopic pregnancy. An exploratory laparotomy was performed and the fetus and placenta were removed without difficulties with a favorable postoperative course. It was concluded that uterine perforation during curettage of the cavity went unnoticed, leading to secondary abdominal implantation of pregnancy with a inconclusive clinical presentation, where ultrasound plays a fundamental diagnostic role. Laparotomy is indicated in most of these cases.
Introduction
Ectopic pregnancy is one of the conditions that contribute to an increase in maternal mortality, reaching between 10 and 15% of maternal mortality cases. Currently there is a significant increase in its incidence, occurring in about 0,8 to 2,0% of all pregnancies [1].
There are multiple predisposing factors to ectopic pregnancy which include the following, a history of pelvic inflammatory disease, endometriosis, three or more induced abortions, as well as history of infertility, previous ectopic pregnancy, early onset of sexual intercourse, multiple sexual partners and the use of intrauterine devices [2].
Ectopic gestation can be implanted in multiple locations. Most of them are tubal (98%), less frequently ovarian (1%) or abdominal (1%), and rarely endocervical (0,1%) or developed on an intramyometrial diverticulum (0,03%). Of all these varieties, primary or secondary abdominal variety is uncommon (with an incidence of one for every ten thousand live births), and presents a much higher risk of maternal death than the other locations (7,7 times more than tubal and 90 times greater than an eutopic one), because it often involves multiple intra-abdominal organs and large blood vessels with massive haemorrhage in case of rupture. Overall, maternal mortality is 0,5 to 18% and the fetal is 40 to 95% [2], [3], [4].
The secondary abdominal location is usually due to a tubal abortion, although it may be due to other causes such as rupture of a uterine horn, a previous caesarean scar, and rarely due to iatrogenic perforation of the uterus during a voluntary attempt to interrupt pregnancy [4].
Considering all of the above, and the low frequency of abdominal gestation secondary to a uterine perforation, this case is presented. Its objective is to emphasize the importance of an early diagnosis of abdominal ectopic pregnancy, which leads to an adequate treatment and that guarantees the survival of the patient.
Clinical case
A 31-year-old African female patient, housewife, with a history of chronic hypertension. Nine weeks prior to admission, voluntarily attempted to terminate pregnancy of eight weeks gestational age by uterine cavity curettage; gestational age obtained by use of last menstrual period date and confirmed by ultrasound. The day after the attempt, the patient started to present hypogastric abdominal pain and minimal vaginal bleeding like spotting and she went to her local clinic for consultation. She was diagnosed with post-abortion acute pelvic inflammatory disease by clinical assessment, without ultrasound. Treatment with antimicrobials (amoxicillin and metronidazole) and analgesics (paracetamol) was started for seven days. This led to improved pain, although sporadic spotting bleeding continued daily.
Three weeks after the treatment, bleeding was more sporadic and, but the pain started again on the same region of the abdomen, taking the left side and the back. For this reason, she went back to her local clinic where she was diagnosed with a urinary tract infection, which was treated with ciprofloxacin and paracetamol for 14 days, showing clinical improvement.
Two weeks after the last treatment, she continued with much more sporadic bleeding. On this occasion abdominal pain was more intense and was accompanied by nausea, small morning vomiting and asthenia for five days. Due to this signs and symptoms, she came to casualty in our hospital. Casualty doctor assessed her as a patient with a history of controlled hypertension on amlodipine, regular menstrual periods of five days every 30 days, with a normal last menstrual period of 16 weeks and 6 days prior, and an obstetric history of two previous normal deliveries. The history of voluntary attempt to terminate pregnancy nine weeks ago was also obtained.
Positive data on the physical examination showed hypogastric and left iliac fossa tenderness on abdominal palpation, palpable mass with slight rebound tenderness. Speculum examination showed a long, posterior and closed cervix with little dark blood in the vaginal fundus. Bimanual examination findings: vagina with normal temperature, a soft cervix with positive cervical motion tenderness, a non-bulging posterior pouch, and an enlarged, regular, and soft uterus. A left, soft, irregular and tender adnexal mass was also palpated.
Vital data signs showed a respiratory rate of 17 per minute, a heart rate of 88 beats per minute, a blood pressure of 107/66 millimeters of mercury and a temperature of 36,4 Celsius degrees. With the data obtained through anamnesis and physical examination, clinical diagnoses of post-abortion endomyometritis and left tubo-ovarian abscess were made, with the need to rule out products of conception in the uterine cavity.
In order to confirm those diagnoses, complementary investigations were performed and it was decided to discuss the case with the specialist to perform an ultrasound, who re-examined the patient and made diagnosis of abdominal ectopic pregnancy due to the clinical presentation and the results of the investigations (Table 1).
 Full size
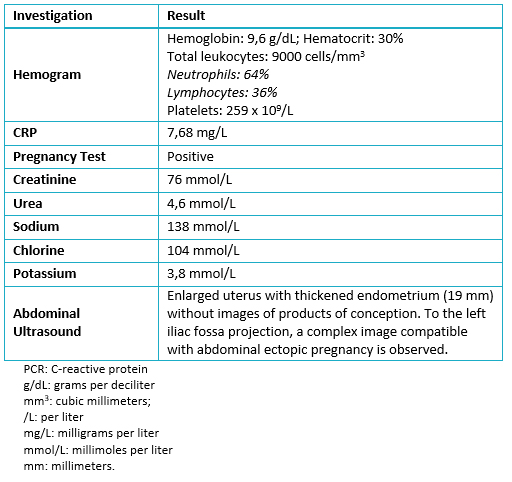
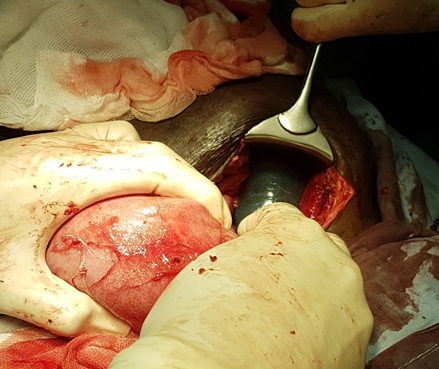
Full size Considering the diagnosis, an emergency exploratory laparotomy was performed. An ectopic pregnancy was found in the abdominal wall of the left iliac fossa (Figure 1), with placenta attached to the parietal peritoneum of this area and to the omentum. Part of it protruding through the perforated area on the anterior wall of the uterus (Figure 2), probably iatrogenic at the time of termination of pregnancy.
 Full size
Full size 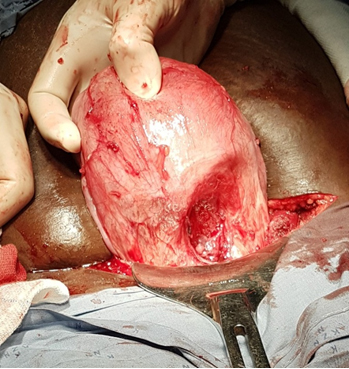 Full size
Full size Manual fetal removal was performed in the amniotic sac and the placenta was also removed (Figure 3). The procedure was completed by curettage of the uterine cavity through the opening caused by the uterine perforation, extracting products that were sent for histopathology investigation. The intervention was concluded with the suturing of the perforation in two planes with chromic catgut (Figure 4).
 Full size
Full size 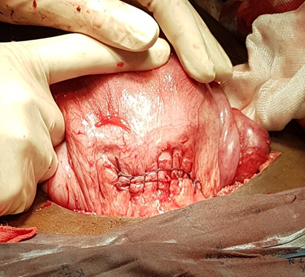 Full size
Full size Subsequent to surgery, the patient recovered favourably. She was discharged 72 hours after surgery, with outpatient follow-up at day 10 and 30 subsequently. She didn’t present with any postoperative complications and her clinical picture resolved completely.
Discussion
Abdominal implantation of an ectopic pregnancy may occur primary or secondary. The Studdi Ford criteria of 1942 are still followed to consider that it is a primary implantation. These criteria are:
- The two tubes and ovaries must be normal, with no evidence of recent or remote trauma.
- There should be no evidence of utero-peritoneal fistulas.
- Pregnancy should be confined exclusively to the peritoneal surface, unrelated to tubal fimbriae, which implies the possibility of secondary implantation after a tube nidation [5].
In this context, the majority of secondary abdominal pregnancies are due to abortion or rupture of a tubal pregnancy, or follow an ovarian implantation. More rarely they are due to a rupture of some part of the uterus. Within this latter cause, it most frequently occurs by rupture of a uterine horn or a previous scar [5], [6].
Implantation secondary to iatrogenic uterine perforation after curettage of the uterine cavity, is only reported in the literature by four authors.These are Wu et al, in Taiwan in 2008; Tubid in India in 2011, Seol et al, in South Korea in 2012, and in 2013 by Chauhan et al, also in India [7], [8], [9], [10].
The diagnosis of secondary abdominal pregnancy is complex, because it presents with very varied non-specific clinical features depending on the site of initial and definitive implantation, gestational age that it reaches and even the probability of passing unnoticed until the term, and becoming an intraoperative finding with perinatal results many times favourable [11].
Wu et al, presented a case of a 23-years-old nulliparous patient who underwent curettage for voluntary termination of pregnancy, similar to the case presented. She underwent laparotomy for uterine perforation when she went to the clinic 19 days after termination of pregnancy attempt complaining of pain and abdominal distension, with signs of peritonitis and hypovolemic shock. The diagnosis of ectopic pregnancy was quickly performed with the help of ultrasound [7].
Furthermore, Tubid also presented a 35-years-old woman who had a voluntary abortion four weeks earlier and consulted complaining of abdominal pain only. It was initially diagnosed as a normal early pregnancy with an ovarian cyst, when he found a soft and enlarged uterus with a left adnexal mass. Subsequently, a secondary abdominal pregnancy was concluded by transvaginal ultrasound [8].
A study by Seol et al, presents a case very similar to the present one; is a 36-year-old patient with a history of voluntary termination of pregnancy through curettage eight weeks earlier. She presented a picture of abdominal pain with spotting vaginal bleeding, which was interpreted in her local clinic as placental remnants, so she was again subjected to dilatation and curettage. Thus, two weeks later she continued with a similar picture, an ultrasound was performed and a reported of an intrauterine mass like a trophoblastic disease and possible pelvic inflammatory disease, which was treated with antimicrobials. When the clinical picture did not solve, she went to the hospital where the diagnosis of secondary abdominal pregnancy was made using ultrasound and tomography [9].
Finally, Chauhan et al, reported a 21-year-old female patient with a history of uterine curettage due to fetal anomalies at 16 weeks and seven days. She consulted complaining of abdominal pain and an increased uterus of around 12 weeks of gestation with signs of infection; it was interpreted as an endometritis or post abortion product of conception. It was decided to perform ultrasound that showed fetal parts in the left iliac fossa that was confirmed by tomography [10].
All cases have in common the history of termination of pregnancy through dilatation and curettage, with recurrent abdominal pain and the presence of an enlarged and soft uterus with palpable or visible adnexal mass through imaging studies that allows definitive suspicion of abdominal pregnancy, very similar to the case presented.
Once the definitive diagnosis has been made, most of the authors agree on the need for surgical management through exploratory laparotomy. It is at this time that unexpected challenges also arise to ensure adequate haemostasis; especially when deciding whether to remove the placenta from its implantation site, which in most cases is strongly attached to neighbouring organs in search of vascularization [11], [12].
In many cases the placenta, or part of it, is retained or is attached to the uterus itself, then a hysterectomy must be performed. In other cases, placental insertion occurs in non-vital organs such as the omentum or the tube, so the organ must be excised together with the placenta. In case of adhesion to vital organs such as the anterior wall of the rectum, the colon, or small intestine, the most prudent is to excise the umbilical cord as close to the placenta and leave it in place [13], [14].
Leaving the placenta at the implantation site requires further medical management, with the use of parenteral methotrexate and follow-up with serial investigations of β-Human Chorionic Gonadotrophin levels and ultrasound. However, it is not free of complications such as infection, intestinal occlusive pictures or secondary bleeding. Therefore, medical management requires close monitoring of the patient [15].
Some limitations to this presentation are; first, we did not take images of the ultrasounds performed which would have improved the quality of this presentation. Secondly, it was impossible to locate the histological result of the sample of the uterine cavity curettage performed during the surgical procedure, an aspect that would have confirmed the secondary implantation of the pregnancy in the abdominal cavity.
Conclusions
Uterine perforation during curettage of the cavity may go unnoticed. For this reason, in a patient with such a history and recurrent abdominal pain, one should consider the possibility of an ectopic pregnancy.
The clinical picture of an abdominal pregnancy secondary to uterine perforation is variable and non-specific, and may lead to misdiagnosis such as pelvic inflammatory disease, urinary tract infection or post abortion products of conception.
Abdominal ultrasound is a complementary examination of high value in the definitive diagnosis of abdominal ectopic pregnancy.
The laparotomic management is the most advisable in these cases, with the removal of the foetus and placenta, especially, if the placenta is implanted in the abdominal wall or the omentum, without affecting other vital abdominal organs.
Notes
Ethical aspects
The informed consent requested by Medwave, has been signed by the patient; A copy of this was sent to the editorial board of the Journal.
Conflicts of Interest
The authors have completed the ICMJE declaration of conflicts of interest form, and declare that they have not received funding for the report; Not having financial relationships with organizations that might have interests in the published article in the past three years; And not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

