Protocols
← vista completaPublished on August 4, 2020 | http://doi.org/10.5867/medwave.2020.07.7970
Effectiveness of telerehabilitation in physical therapy: A protocol for an overview in a time when rapid responses are needed
Efectividad de la telerehabilitación en terapia física: protocolo de una revisión global en tiempos que exigen respuestas rápidas
Abstract
Introduction Rehabilitation and physical therapy have been adapting to the telehealth era, increasing accessibility and improving the continuity of attention in geographically remote populations with disabilities. Due to the spread of infection by SARS-CoV-2, many professionals have had to adapt their work to telerehabilitation practices, which require the best evidence at short notice and in summarized form. In this context, this protocol has been developed to evaluate the effectiveness of telerehabilitation as a care strategy in physical therapy for different conditions, populations, and contexts.
Method and analysis An overview will be carried out in the format of a rapid review. It will include systematic reviews of different conditions, populations, and contexts, where the intervention to be evaluated is telerehabilitation by physical therapy. The outcomes considered will be clinical effectiveness depending on the specific condition, functionality, quality of life, satisfaction, adherence, and safety. A search will be carried out of the MEDLINE/PubMed, EMBASE, and Cochrane Library databases. Studies will be selected in duplicate with any discrepancies resolved by a third reviewer. Data extraction and risk of bias assessment will be carried out by a reviewer with non-independent verification by a second reviewer. The findings will be reported qualitatively by tables and figures.
Ethics and dissemination The principles of the value of the research question, the methodological rigor, scientifically qualified investigators, an independent evaluation of the protocol, and timely and accurate publication of the results will be complied with. The complete review will lead to the publication of at least one article, and the results will be widely disseminated at various levels of decision-making.
Register This protocol has been registered in PROSPERO with the number CRD42020185640.
|
Main messages
|
Introduction
Life exposes people to a continuous, dynamic cycle of improving and declining health. Prevention plays a basic role in ensuring that the state of optimum health is as prolonged and frequent as possible. Despite preventive efforts, various conditioners result in disease and a less than fully functional state of health, which evolves over time. In such situations, therapeutic and secondary prevention interventions are needed, including rehabilitation.
Rehabilitation includes a set of interventions necessary when a person suffers or is likely to suffer, limitations to his or her everyday life as a consequence of aging or a condition—such as a disease or chronic disturbance, lesion, or trauma[1]. The primary objective is to maximize people's ability to live, work, and learn as much as possible, improving functionality and quality of life. The impact extends to the community, society, and even the economy[2],[3].
World trends in health and aging require a substantial increase in rehabilitation services in all countries, especially low and middle-income countries. Thus, the World Health Organization (WHO) has recommended the integration of rehabilitation into health systems at the primary, secondary and tertiary levels, with a multi-disciplinary workforce, including services based in the community and hospitals; and if necessary, the provision specialized units for attention to hospitalized patients with complex needs[3]. Moreover, universal health coverage is identified as the third Sustainable Development Goal[4], for which countries must guarantee equal access to high-quality health services, including rehabilitation. One reflection of this challenge is the establishment of a global strategy led by the WHO called Rehabilitation 2030[5].
Rehabilitation is, by definition, an integral, multi-component, multi-disciplinary intervention. The ambit of the health condition or problem to be addressed, with other conditioners of the specific health system or availability of resources, determine which disciplines, professions, or components are the minimum required. One type of intervention frequently found in rehabilitation programs is physical therapy.
Physical therapy (or physiotherapy) is a service provided by a physical therapist (also known as a physiotherapist) to develop, maintain and re-establish movement and functional capacity in all stages of life. Physiotherapeutic interventions are required in circumstances in which movement and function are threatened, as functional movement is fundamental for health and optimal quality of life. Physical therapists work to prevent, treat, habilitate, and rehabilitate problems; to do this, they interact and work in teams with patients, other health professionals, families, carers and communities[6]. Thus, physical therapy interventions may be carried out as the sole treatment in certain conditions, but much more frequently, they are included in a more integral rehabilitation program.
The demand for rehabilitation and physical therapy services is increasing as the population ages and chronic, degenerative problems derived from the conditions of modern life increase. This demand sometimes leads to the saturation of services and the build-up of waiting lists[7], with consequent delays in treatment. In other circumstances, despite its known benefits, this resource is underutilized[8]. This underutilization is especially true for people of limited resources[9],[10], who prioritize other types of health needs, often more urgent and necessary for immediate survival.
In this scenario, where rehabilitation is necessary but insufficiently implemented, alternative rehabilitation models have been created to improve coverage while making the most of new types of resources, such as technology. Thus, rehabilitation has adapted to the telehealth era.
Telehealth is based on the use of telecommunications and virtual technology to provide health services outside traditional health centers when distance is a critical factor[11]. Telehealth is a dynamic concept that is in constant evolution as needs and technology evolve; terms like eHealth, mHealth, cyber-health, virtual health, or digital interventions have become common; these terms are not synonymous as they have distinctions[12].
Telerehabilitation is considered a branch of telehealth. It consists of a system for the control or monitoring of remote rehabilitation using telecommunications technologies. It has been proposed as a way of increasing accessibility and improving the continuity of attention in vulnerable, geographically remote populations with disabilities, with the potential for saving time and money[13],[14]. In the specific area of physical therapy, there has been discussion recently on the benefits and limitations of digital practice or telehealth; the object is to facilitate the effective provision of physical therapy services by improving access to attention[15]. Conditions or circumstances have also been identified in which physical therapy can be practiced by digital means, such as education on health conditions, promotion of independence, prescription of therapeutic exercise, advice on physical activity or an exercise plan, and follow-up and monitoring of the progress of patients previously treated face-to-face[16].
There are many models of telerehabilitation, or ways of delivering physical therapy services outside of a physical care center, which have been implemented around the world[17],[18],[19]. There are also many and varied studies that have sought to prove their effectiveness, comparing this form of intervention with face-to-face care, and even with non-delivery of the service in contexts where rehabilitation is not possible. Today, so many experimental studies are available on telerehabilitation or remote physical therapy that many systematic reviews have tried to summarize the scattered and contradictory findings of different models of telerehabilitation for different conditions.
In the current context, 2020, when infection by SARS-CoV-2 has spread around the world generating the COVID-19 pandemic, health services have had to adapt and prioritize telerehabilitation and the patients who receive treatment in care centers, limiting ambulatory attention and reinventing how healthcare providers attend to users in record time. Consequently, in addition to finding a safe, direct way of treating patients affected by COVID-19, an innovative method had to be found of providing rehabilitation or physical therapy; many care centers have abruptly modified how they deliver interventions to people in need for reasons unrelated with COVID-19[20]. Although the principal task is to contain the propagation of the infection and treat patients affected by COVID-19, the health system cannot allow the side effects of failing to attend to other health problems to get out of control.
In order to provide timely support to physical therapists with the best evidence available, we have assumed the task of compiling the available information, obtained from systematic reviews on the subject, in a rapid review format.
Research question
Is telerehabilitation an effective physical therapy attention strategy for different conditions, populations, and contexts?
Objective
To assess the effectiveness of telerehabilitation as a physical therapy attention strategy for different conditions, populations, and contexts.
Method
Design
An overview will be carried out in the form of a rapid review. The object of an overview also called umbrella review or review of reviews, is to provide a summary of evidence obtained from several systematic reviews, including a combination of different interventions, outcomes, conditions, problems or populations[21],[22]. This type of review arises from the need to compile the information from a variety of systematic reviews on a particular subject, basically to support decision-making[21]. There are different approaches to the design of an overview. We have selected a design to summarize the evidence on a single type of intervention (telerehabilitation) for different outcomes, conditions, and populations[22].
Rapid reviews have been developed as a rationalized approach to summarizing evidence to inform decisions on new issues faced by decision-makers or professionals in various ambits of health attention[23]. Apart from a much more limited time frame, this format differs from a systematic review in various aspects of its methodology, the application, and publication of which in turn are variable[24]. For this overview, we have considered: limiting the search sources, extracting data without duplication but with non-independent verification, and providing a descriptive summary of the findings.
This protocol has been structured following the PRISMA-P guidelines[25], and the overview report will likewise adhere to the PRISMA declaration for systematic reviews[26].
Eligibility criteria for the type of studies
Systematic reviews will be identified and considered eligible if they include an explicit, systematic review methodology, and the primary studies included are clinical trials. If a systematic review includes studies with observational designs, they will be included only when they contain desegregated data from clinical trials. Systematic review protocols and conference presentations will be excluded if the full text of the work is not available.
Eligibility criteria for participants and context
Systematic reviews on various conditions of interest (musculoskeletal, neurological, respiratory, cardiovascular, among others), populations (infants, children, adults, and the elderly) and contexts (primary, secondary and tertiary or specialist attention) will be included.
Eligibility criteria for intervention
Telerehabilitation by physical therapy: any intervention defined as the provision of rehabilitation with interventions in any area of physical therapy (musculoskeletal, neurological, respiratory or cardiac rehabilitation), carried out remotely or outside a usual attention center (health center) by a therapist distant from the patient/user, and using telecommunications technologies.
A systematic review will be included when the experimental arm consists of integral telerehabilitation with at least one component of physical therapy or when it contains a physical therapy treatment only.
Physical therapy will be understood as any of the interventions usually carried out by a physical therapist or physiotherapist as defined by the World Confederation for Physical Therapy[6]: therapeutic exercises, functional training, manual therapy, respiratory techniques and exercises, integumentary repair and protection techniques, electrotherapy and physical agents, and education.
Reviews that focus on physical activity will also be included only when they consider clinical outcomes (e.g., glycemic control). Similarly, reviews of self-management of health conditions (e.g., diabetes) will be included only when it is observed that the intervention considers exercise and its effects on a clinical outcome. Finally, reviews that consider mobile applications and monitors (e.g., pedometer) will be included only when they involves the active action of a physical therapist.
Systematic reviews assessing so-called virtual interventions (e.g., virtual reality) without remote supervision by a therapist and not explicitly stating that they are performed outside the health center will be excluded.
Eligibility criteria for comparison
Systematic reviews will be included where the comparison group is one of the following: presential rehabilitation (comprehensive with at least one component of physical therapy or physical therapy only), standard rehabilitation, no rehabilitation, or usual care.
Eligibility criteria for outcomes
The following primary outcomes will be considered:
- Clinical effectiveness for each condition (e.g., decrease of pain in fibromyalgia; increased range of movement after immobilization due to a fracture; diminution of dyspnea in COPD; an increase of VO2 max in coronary disease; diminution of spasticity in cerebral palsy, among others).
- Functionality conceived as the physical abilities which allow functional independence, measured with validated instruments widely used in the discipline (e.g., Action Research Arm Test, ARAT).
- Health-related quality of life, considering the physical, psychological, and social aspects of health, influenced by a person's experiences, beliefs, expectations and perceptions. Measurements should be by validated generic (e.g., SF-36) or condition-specific questionnaires (e.g., Chronic Respiratory Questionnaire, CRQ).
The following secondary outcomes will be considered:
- Satisfaction with the attention, assessed by questionnaires or subjective methods.
- Adherence, as defined by each review or primary study, contained in the reviews.
- Adverse effects, defined as the appearance of an undesired sign, symptom or medical condition.
Search strategy
A systematic search will be carried out in the following electronic databases:
- Medline/Pubmed
- EMBASE
- Cochrane Library
The search strategy will take a sensitive approach, using controlled (Mesh, EMTREE) and natural language. The search chains will be linked with the Boolean operators OR, AND, and the Systematic Reviews, Meta-Analysis, and Review limits will be applied, as available in each database.
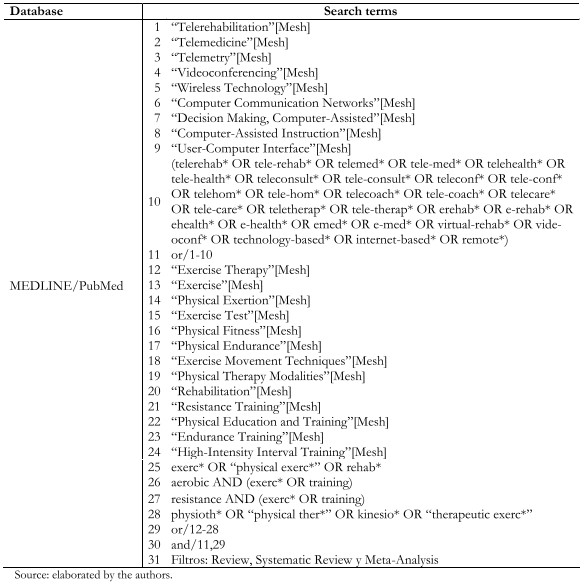 Full size
Full size Selection process
All the records resulting from each search will be exported to the Rayyan software[27]. Once the duplicate records have been eliminated, two investigators will screen by title and abstract. Then the full texts of the relevant records will be reviewed, also in duplicate. A third, more experienced reviewer will resolve any discrepancies in these two phases. The reasons for exclusions in the full-text phase will be described in a table.
Data extraction
The relevant information from each eligible document will be extracted by one investigator, and non-independent verification will be carried out by another investigator through the REDCap© platform (Research Electronic Data Capture software)[28].
The following data of interest will be extracted:
- General information on the review (journal, year of publication, research team, associated institutions, countries involved).
- Type of participants and conditions studied.
- Characteristics of the experimental intervention:
- Type of physical therapy.
- In a multi-component rehabilitation program or as a sole intervention.
- Telerehabilitation modality (video-conference, telephone call, text message, internet platform, etc.).
- Types of comparison.
- Outcomes reported.
- Qualitative and quantitative results obtained.
- Conclusions drawn.
Evaluation of the risk of bias
We will use the ROBIS (Risk of Bias in Systematic Reviews) tool. ROBIS has been designed, among other purposes, for use by investigators carrying out overviews of systematic reviews. It differs from other instruments used for critical analysis or exclusively for meta-analysis, and is not explicitly intended for assessing the risks of bias underlying the design, execution, and summary of a systematic review[29].
ROBIS is applied in three consecutive phases:
- Evaluation of the relevance of the review for the research question (in this case our overview).
- Identification of concerns with the review process, which contains four domains:
- Study eligibility criteria.
- Identification and selection of the studies.
- Data collection and study appraisal.
- Synthesis and findings.
- Judgment of bias in the review, where:
- The concerns for each domain of phase 2 are summarized.
- Three further questions are answered on the interpretation of the review findings.
- Overall evaluation is generated.
The ROBIS tool will be applied by one investigator, and non-independent verification of the results will be carried out by a second investigator.
Synthesis of results
Initially, the results of the selection process, the general characteristics, and the risk of bias of the included reviews will be described.
A qualitative report of the effectiveness findings will be made, summarized in tables and figures by the clinical area of rehabilitation or physical therapy involved. In the design and presentation of the tables and figures, the risk of bias of the included reviews will be considered, in order to systematically include this factor in the generation of conclusions. Depending on the number of reviews per clinical area, the results may be reported in different documents.
Ethical implications
Although a secondary study does not intervene directly on human beings, offering the assumption of no direct risk, annoyance, or discomfort for the study subjects, ethical norms must nevertheless guide the actions carried out (or not) in the framework of the study.
In carrying out our overview, we will comply with the principles on which ethical norms are based: the value of the research question, methodological rigor, scientifically qualified investigators, independent evaluation of the protocol, and, finally, accurate and timely publication of the results.
Notes
From the editors
The original version of this manuscript was submitted in Spanish. This English version was submitted by the authors and has been lightly copyedited by the Journal.
Authors' contributions
PS: conceptualization and proposed and wrote the protocol. MJO, RF, and RG contributed actively to protocol design, reviewed the manuscript critically, and approved it.
Conflict of interests
The authors declare that there is no conflict of interest.
Funding
This manuscript is within the framework of the activities of the project "FONDECYT Regular 2018", Grant N° 1181734, financed by the National Agency for Research and Development (ANID), Chile.
Register
The protocol is registered in PROSPERO under number CRD42020185640.

