Resúmenes Epistemonikos
← vista completaPublicado el 28 de agosto de 2015 | http://doi.org/10.5867/medwave.2015.6235
¿Noradrenalina o terlipresina para el síndrome hepatorrenal?
Noradrenaline or terlipressin for hepatorenal syndrome?
Resumen
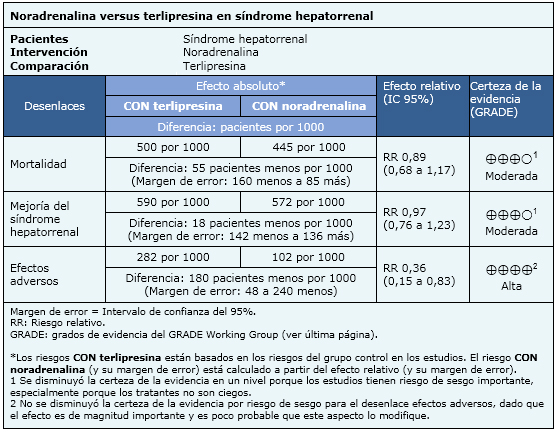
El síndrome hepatorrenal es una condición asociada a altísima mortalidad, que puede ser recuperada en ciertos casos con el uso de vasoconstrictores. Generalmente se considera que terlipresina es el tratamiento estándar, pero noradrenalina se ha planteado como una alternativa. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en 30 bases de datos, identificamos seis revisiones sistemáticas que en conjunto incluyen cuatro estudios aleatorizados. Realizamos un metanálisis y tablas de resumen de los resultados utilizando el método GRADE. Concluimos que noradrenalina y terlipresina son probablemente igual de efectivas en lograr mejoría del síndrome hepatorrenal y disminuir la mortalidad, pero que noradrenalina se asocia a menos efectos adversos, y tiene un menor costo.
Problema
El síndrome hepatorrenal constituye una condición asociada a alta mortalidad. Se produce por una intensa vasoconstricción renal causada por la interacción entre alteraciones hemodinámicas a nivel sistémico y portal, particularmente por vasodilatación del lecho arterial esplácnico. El aumento del volumen intravascular y un prolongado tratamiento con fármacos vasoconstrictores pueden revertir la falla renal en algunos pacientes. El uso de terlipresina mejora la función renal y disminuye la mortalidad, sin embargo tiene efectos adversos frecuentes, un costo alto y no se encuentra ampliamente disponible. Se ha planteado el uso de otros vasopresores como noradrenalina, la cual se encuentra ampliamente disponible y tiene un costo menor.
Métodos
Utilizamos la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en 30 bases de datos, para identificar revisiones sistemáticas y sus estudios primarios incluidos. Con esta información generamos un resumen estructurado, siguiendo un formato preestablecido, que incluye mensajes clave, un resumen del conjunto de evidencia (presentado como matriz de evidencia en Epistemonikos), metanálisis del total de los estudios, tablas de resumen de resultados con el método GRADE, y tabla de otras consideraciones para la toma de decisión.
|
Mensajes clave
|
Acerca del conjunto de evidencia para esta pregunta
|
Cuál es la evidencia. |
Encontramos seis revisiones sistemáticas [1],[2],[3],[4],[5],[6] que incluyen cuatro estudios controlados aleatorizados, reportados en 5 referencias [7],[8],[9],[10],[11]. |
|
Qué tipo de pacientes incluyeron los estudios |
Los estudios incluyeron pacientes adultos, con daño hepático avanzado (Child Pugh C). Dos estudios incluyeron pacientes con síndrome hepatorrenal tipo 1 [9],[11], un estudio incluyó a pacientes con síndrome hepatorrenal tipo 2 [8] y un estudio no discriminó por tipo de síndrome hepatorrenal [7]. El score de MELD oscilaba entre 20 y 30 puntos en tres estudios [7],[9],[11] y mayor a 30 puntos en uno [8]. La creatinina promedio osciló entre 2 y 3 mg/dl en todos los estudios. |
|
Qué tipo de intervenciones incluyeron los estudios |
Todos los estudios compararon uso de terlipresina comparado con uso de noradrenalina. La dosis de noradrenalina osciló entre 0,5 a 3 mg/hr. La dosis de terlipresina fue 0,5 a 2 mg cada 6 hrs en tres estudios [8],[9],[11] y un estudio [7] utilizó 1 a 2 mg cada 4 hrs. |
|
Qué tipo de desenlaces midieron |
Se midió mortalidad, mejoría de la función renal y eventos adversos. |
Resumen de los resultados
La información sobre los efectos de noradrenalina comparada con terlipresina está basada en cuatro estudios aleatorizados que incluyen 154 pacientes. Todos los estudios reportaron el desenlace mortalidad, mejoría del síndrome hepatorrenal y efectos adversos.
- Noradrenalina y terlipresina son probablemente igual de efectivas en lograr mejoría del síndrome hepatorrenal. La certeza de la evidencia es moderada.
- Noradrenalina y terlipresina son probablemente igual de efectivas en disminuir la mortalidad. La certeza de la evidencia es moderada.
- Noradrenalina tiene menos efectos adversos que terlipresina. La certeza de la evidencia es alta.
Otras consideraciones para la toma de decisión
|
A quién se aplica y a quién no se aplica esta evidencia |
|
| Sobre los desenlaces incluidos en este resumen |
| Balance riesgo/beneficio y certeza de la evidencia |
|
| Consideraciones de recursos |
|
|
Diferencias entre este resumen y otras fuentes |
|
| ¿Puede que cambie esta información en el futuro? |
|
Cómo realizamos este resumen
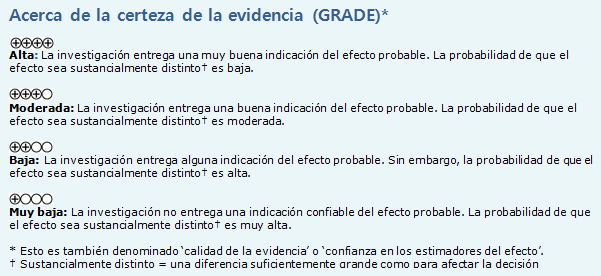
Mediante métodos automatizados y colaborativos recopilamos toda la evidencia relevante para la pregunta de interés y la presentamos en una matriz de evidencia.
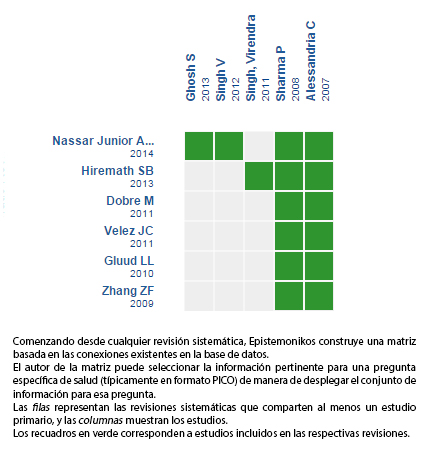 Tamaño completo
Tamaño completo Siga el enlace para acceder a la versión interactiva: Terlipresina versus noradrenalina para el síndrome hepatorrenal
Notas
Si con posterioridad a la publicación de este resumen se publican nuevas revisiones sistemáticas sobre este tema, en la parte superior de la matriz se mostrará un aviso de “nueva evidencia”. Si bien el proyecto contempla la actualización periódica de estos resúmenes, los usuarios están invitados a comentar en Medwave o contactar a los autores mediante correo electrónico si creen que hay evidencia que motive una actualización más rápida.
Luego de crear una cuenta en Epistemonikos, al guardar las matrices recibirá notificaciones automáticas cada vez que exista nueva evidencia que potencialmente responda a esta pregunta. El detalle de los métodos para elaborar este resumen están descritos aquí: http://dx.doi.org/10.5867/medwave.2014.06.5997.
La Fundación Epistemonikos es una organización que busca acercar la información a quienes toman decisiones en salud, mediante el uso de tecnologías. Su principal desarrollo es la base de datos Epistemonikos (www.epistemonikos.org).
Los resúmenes de evidencia siguen un riguroso proceso de revisión por pares interno.
Declaración de conflictos de intereses
Los autores declaran no tener conflictos de intereses con la materia de este artículo.

