Epistemonikos summaries
← vista completaPublished on January 17, 2018 | http://doi.org/10.5867/medwave.2018.01.7134
Bipolar or monopolar transurethral resection for benign prostatic hyperplasia?
¿Resección transuretral bipolar o monopolar para hiperplasia prostática benigna?
Abstract
INTRODUCTION Transurethral resection is currently considered as standard endoscopic treatment for lower urinary tract obstruction due to benign hyperplasia under 80 cc. Monopolar resection loops has been traditionally used but bipolar energy has recently displaced precedent technology. The purpose of this summary is to evaluate the efficacy and safety of both technologies.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified 13 systematic reviews including 32 primary studies, among them 31 randomized trials. We concluded although there may be no difference in terms of efficacy among both techniques, the use of bipolar energy reduces the incidence of transurethral resection syndrome and probably reduces the risk of bleeding that requires red blood cell transfusion.
Problem
Lower urinary tract obstruction caused by benign prostatic hyperplasia is a prevalent condition that causes bothersome symptoms and impaired quality of life. Occasionally, it can lead to complications that determine morbidity and mortality.
Transurethral resection has been traditionally considered standard endoscopic treatment for prostates of less than 80cc, being monopolar loops the most broadly used. However, its use is not free of complications such as transurethral resection syndrome, a clinical entity caused by the absorption of hypoosmolar fluids used in monopolar techniques. Bipolar diathermy emerged as an alternative that could be associated with a lower incidence of complications, provided by the use of isotonic solutions for the resection of the prostate. The purpose of this summary is to evaluate the clinical efficacy and safety of both techniques.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We identified 13 systematic reviews [1],[2],[3],[4],[5],[6],[7], This table and the review in general are based on the latter, since the observational study [57] did not improve the certainty of the evidence or provided additional relevant information. |
|
What types of patients were included* |
Patients with lower urinary tract obstruction due to benign prostatic hyperplasia who required endoscopic treatment were included. Patients with suspicion of prostate cancer or other causes of lower urinary tract obstruction were excluded. Average age ranged between 59 and 73 years in the different trials. Average prostate volume ranged between 39.5 and 82.5 cc. |
|
What types of interventions were included* |
Seventeen trials [15],[22],[26],[27],[31],[38],[39],[40],[42], Eight trials [14],[16],[20],[28],[32],[41],[50],[55] used Olympus TURis bipolar resectoscope. Three trials [43],[49],[58] used Vista CTR bipolar resectoscope. One trial [45], used AUTOCON II Storz resectoscope. The systematic reviews identified did not report which monopolar resectoscope was used in each trial. |
|
What types of outcomes |
Multiple outcomes were measured in the trials. They were grouped in the systematic reviews as follows: magnitude of the obstruction (maximum urinary output (QMax) in ml/seg measured by uroflowmetry, postvoid residual volume, symptoms and quality of life using the International Prostate Symptoms Score (IPSS). Perioperative parameters (duration of surgery, hospital stay, urinary catheterization time, red blood cell transfusion rate and incidence of transurethral resection syndrome were also measured), and late postoperative complications such as erectile dysfunction, urethral stenosis, bladder neck contracture, urinary incontinence, reintervention rate, among others were assessed as well. Follow-up median among the trials was 12 months with a range of 1 to 60 months. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of Findings
The information about the effects of bipolar versus monopolar transurethral resection of the prostate is based on 31 randomized trials that include 4670 patients.
Twenty-five trials reported red blood cell transfusion rate (3585 patients) [14],[15],[16],[19],[20],[22],[26],[27],[28],[30],[31],[32],[39],[42],[44],[45],[49],[50],[53],[54],[58],[59],[60],[61],[62], 25 trials reported the incidence of transurethral resection syndrome (3436 patients), [14],[15],[16],[19],[20],[22],[26],[27],[30],[31],[32],[39],[42],[44],[45],[49],[50],[53],[54],[55],[58],[59],[60],[61],[62], 11 trials measured IPSS at 12 months (1452 patients) [16],[20],[27],[39],[45],[53],[56],[57],[59],[60],[62] and 13 trials measured QMax at 12 months (1649 patients) [16],[19],[20],[27],[31],[39],[45],[53],[56],[57],[59],[60],[62].
The summary of findings is:
- The use of bipolar energy reduces the incidence of transurethral resection syndrome. The certainty of the evidence is high.
- The use of bipolar energy probably reduces the incidence of bleeding that require red blood cell transfusion. The certainty of the evidence is moderate.
- The use of bipolar energy probably makes little or no difference in IPSS at 12 months compared with the use of monopolar resectoscope. The certainty of the evidence is moderate.
- The use of bipolar resectoscope might make little or no difference in the QMax at 12 months compared with the use of monopolar energy, but the certainty of the evidence is low.
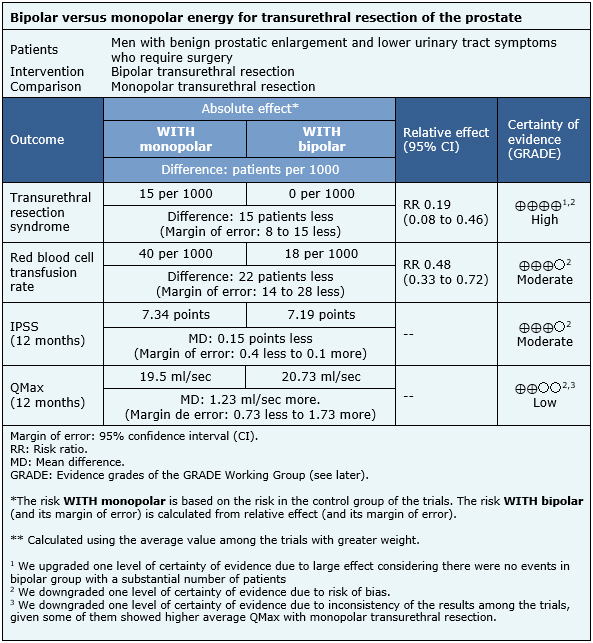
| Following the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
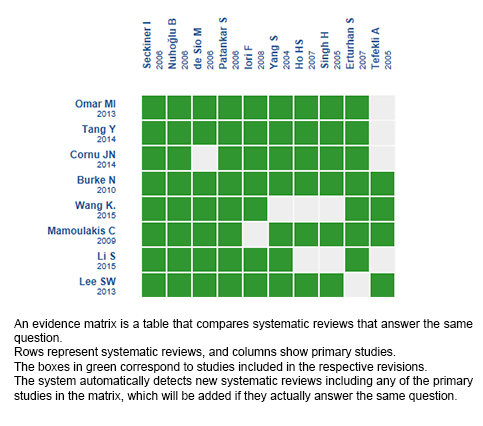
Follow the link to access the interactive version: Bipolar versus monopolar transurethral resection of the prostate for benign hyperplasia
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

