Short communications
← vista completaPublished on January 9, 2021 | http://doi.org/10.5867/medwave.2021.01.8097
How the COVID-19 pandemic affects specialty training: An analysis of a nationwide survey among otolaryngology residents in Chile
Impacto de pandemia COVID-19 en la formación de residentes: análisis de una encuesta nacional a residentes de otorrinolaringología en Chile
Abstract
Introduction Coronavirus disease 2019, or COVID-19, has become a global pandemic. Given that the highest viral load of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is found in the airway, otolaryngologists are at high risk of infection. As a result, multiple recommendations have emerged regarding protective measures for surgical teams, including suspending non-urgent procedures and surgeries.
Objectives To evaluate the impact of the COVID-19 pandemic on otolaryngology residency training programs nationwide.
Methods A cross-sectional survey-based study was completed in April 2020. The participants were recruited through an online survey, sent by email to all Chilean otolaryngology residents. Demographics, clinical activities, on-call shifts, COVID-19 infection status, exposure to COVID-19 patients, deployment to other specialties, diagnostic/therapeutic procedures, and surgeries performed were analyzed. Self-reported surgical data logs from previous years were used to compare results.
Results Forty-seven residents completed the survey (84% response rate); 64% of residents refer seeing patients ten days or less during April 2020. Commonly performed procedures such as flexible nasolaryngoscopy, rigid nasal endoscopy, and peritonsillar abscess drainage were not performed by over 40% of the residents in that month. Only 38% participated in surgeries, with an average of 0.6 surgeries as a first surgeon, a dramatic decrease in surgical exposure when comparing the data logs from previous years. Most residents refer the following measures taken by their residency program to improve residency training: bibliographic videoconferences (87%), online clinical case seminars (60%), weekly journal clubs (38%), among others.
Conclusions Clinical and surgical opportunities decreased dramatically during April 2020. Adjustments to the regular academic curricula should be considered to decrease the negative impact of this pandemic on residency training.
Main messages
- At the time of preparation of this study, no articles reported the effect of the COVID-19 pandemic on medical residents’ training in Chile.
- This study presents the objective decrease in Chilean otolaryngology residents’ procedures and surgeries due to the COVID-19 pandemic.
- A limitation of this study is the one-month follow-up during the pandemic.
- Other limitations are the absence of comparative data on functional endoscopic surgery and head and neck oncologic surgery due to incomplete historical self-reported data in these two clinical areas.
Introduction
On March 11, 2020, the World Health Organization declared the coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), as a global pandemic[1]. Given the high airborne viral load[2], otolaryngologists are at a high risk of infection as multiple procedures involve the airway, such as rigid nasal endoscopy, flexible nasolaryngoscopy, anterior nasal packing, tracheostomy, among others. These procedures can also cause aerosolization[3],[4].
As a result, guidelines have been created regarding the protective measures for performing these procedures, including suspending elective procedures and surgeries, minimizing on-call personnel, establishing resident rotation cohorts, and having the most experienced surgeon perform the procedure in the shortest time possible[5],[6],[7],[8].
Taking the above into consideration, and the fact that most otolaryngology outpatient clinics, procedures, and surgeries are optional, we suspected that the COVID-19 pandemic would negatively impact residency training due to the significantly reduced clinical and surgical opportunities[9].
To the best of our knowledge, as of this study’s date, no articles describe the effect of the COVID-19 pandemic on residents’ educational opportunities in Chile.
This study aims to explore the impact of COVID-19 on the otolaryngology residency training programs nationwide and describe the decrease in surgical exposure.
Methods
Clinical opportunity survey
We performed a cross-sectional survey-based study evaluating April 1 to April 30, 2020. There are currently five otolaryngology programs in Chile. Subjects were recruited through a 16-question Google form sent by email to all Chilean otolaryngology residents; the program directors provided contact information.
We obtained demographic data, post-graduate year, and the following information for April 2020: clinical activities, on-call shifts, COVID-19 infection status, exposure to COVID-19 patients, deployment to other specialties, diagnostic/therapeutic procedures performed, and surgeries (first and second surgeons only). We defined COVID-19 positive patients as confirmed by a reverse transcription-polymerase chain reaction and suspected cases when results were pending. Survey response was open from May 11 to May 18, 2020.
Clinical data logs
Historical data logs for specialty diagnostic and therapeutic procedures were only available from student self-reported data logs provided by one residency program from 2017 to 2019: Pontificia Universidad Católica de Chile. Meanwhile, surgeries performed by residents from years prior were only available from student self-reported data logs provided by two residency programs: Pontificia Universidad Católica de Chile and Universidad de Chile, with data from 2017 to 2019 and 2006 to 2016, respectively. Both data logs consisted of procedures or surgeries registered by the residents after their execution. No determination of sample size was required, given the nature of the study.
Data analysis and statistics
This study was approved by the Pontificia Universidad Católica de Chile Ethics Committee (protocol number: 200501001) on May 9, 2020. Electronic informed consent was obtained from all participants before data collection. The data collection was carried out anonymously in an encrypted database. When presenting normal distribution, the descriptive statistics will be expressed with mean and standard deviation. Otherwise, the median was used. The chi-squared test was performed for categorical variables. The means obtained were compared using the student’s T-test. Any P value < 0.05 (significance of 5%) was considered significant.
Results
Forty-seven residents answered the survey, corresponding to an 84% response rate and a mean age of 29.7 ± 3.2 years (range 25-35). Demographic details are shown in Table 1. Six percent of residents were placed initially in preventive quarantine as they belonged to a high-risk group for SARS-CoV-2 infection; 50% (n = 23) provided medical care to a confirmed or suspected COVID-19 patient during April 2020; of them, only 13% (n = 6) needed to undergo preventive quarantine; and one resident tested positive. The average suspected/confirmed patients evaluated per resident was 8.1 ± 8.7 (range 1-30 patients). Thirteen percent (n = 6) of the residents were deployed to a different department as needed by the health care center, with internal medicine being the most frequent (n = 5/6).
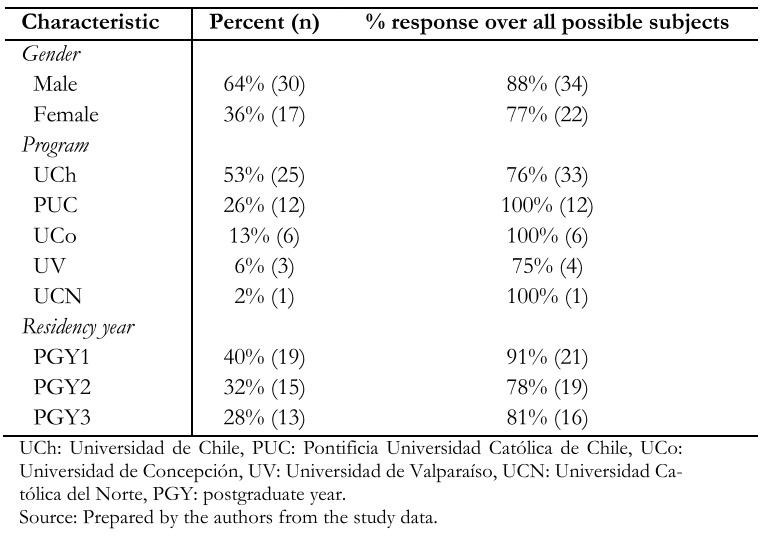 Full size
Full size Clinical activity
Clinical activities during April 2020 are summarized in Table 2; 65% of the residents spent less than ten days of the month at their corresponding medical health care center, and 68% examined less than eleven patients in outpatient clinics.
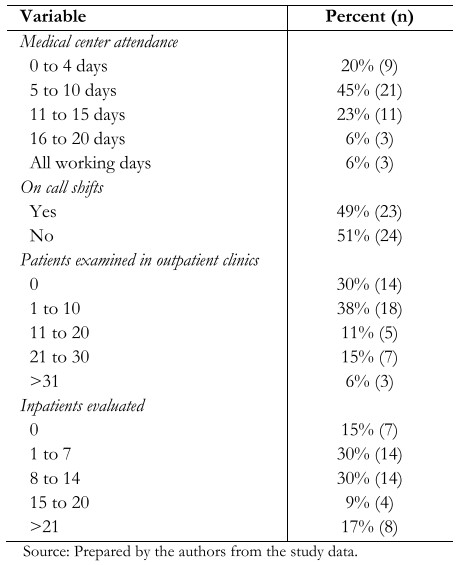 Full size
Full size Regarding commonly performed procedures, only 55% of the residents performed flexible nasolaryngoscopy, 34% rigid nasal endoscopy, and 21% peritonsillar abscess drainage as seen in Table 3. When analyzing the data obtained from the Pontificia Universidad Católica de Chile residency program, there was a significant decrease in the average procedure per resident for flexible nasolaryngoscopy (13.1 ± 7.5 vs 1.4 ± 1.5, P = 0.001), rigid nasal endoscopy (3.6 ± 2.9 vs 0.4 ± 0.7, P = 0.001), anterior nasal cauterization (0.8 ± 0.5 vs 0.1 ± 0.3, P = 0.002), and fiberoptic endoscopic evaluation of swallowing (3.6 ± 2 vs 0 ± 0, P = 0.000).
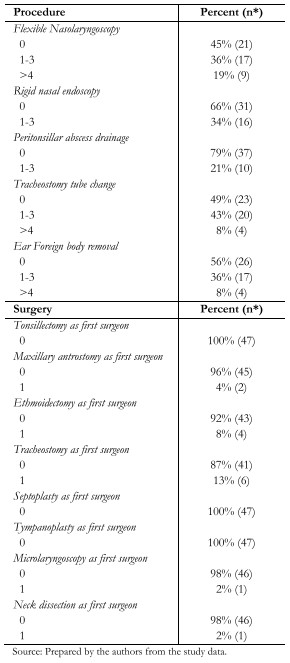 Full size
Full size Surgical activity
Of the residents surveyed, 62% (n = 29) did not participate in surgery; of the 18 that did participate, 67% (n = 12) performed as first surgeon, with an average of 0.6 ± 1.2 (range 0-5) surgeries per resident. The most commonly performed surgery was open tracheostomy (n = 6) followed by ethmoidectomy (n = 4), as seen in Table 3. As shown in Figure 1, we observed a dramatic decrease in surgical exposure when comparing data obtained from the Pontificia Universidad Católica de Chile and the Universidad de Chile.
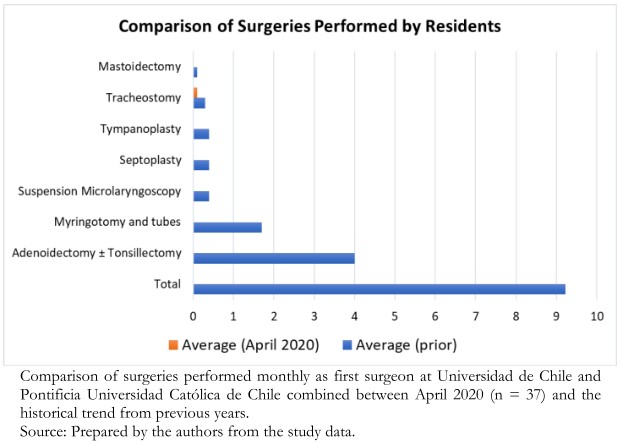 Full size
Full size Educational tools
Residents were asked to provide information relating to measures taken by their residency program in order to promote continuing education and distance learning. Most residents reference bibliographic videoconferences (87%, n = 41), and online clinical case seminars (60%, n = 28). Other measures included weekly journal clubs (38%, n = 18), bibliographical reviews (34%, n = 16), online surgical skills video analysis (15%, n = 7), simulation opportunities (17%, n = 8), and others (8%, n = 4).
Discussion
In this survey, we describe how the pandemic is undermining the education of residents in otolaryngology by reducing clinical and surgical opportunities. This was reflected in the procedures performed, with a significant decrease in flexible nasolaryngoscopy, rigid nasal endoscopy, and others. Furthermore, we believe that the most critical item affected is exposure to surgical opportunity; only 38% of the residents were involved in the operating room, and just 25% performed as the first surgeon for the entire month. We evaluated whether there was an association regarding the post-graduate year and being the first surgeon, but this was not significant (P = 0.0631). We believe that some of the factors that are possibly involved in the pandemic’s impact include the number of residents per hospital, mandatory quarantines depending on the city, and the population size for the different hospitals.
As it is uncertain when the pandemic will end, attention must be paid to provide residents with educational opportunities, especially regarding surgical skills. Some of the otolaryngology departments’ measures during April included videoconferences (bibliographical, case seminars, weekly journal clubs), bibliographical reviews, online surgical skills video analysis, and simulation opportunities.
At the moment our survey was completed, there were 65.393 cases[10]; we suspect that our activity level will be further affected as the peak of infection was in June. As many institutions arestill restricting outpatient clinics, we do not know how deeply this pandemic will impact our residency programs, we believe that measures should be taken by our sanitary authorities in order to insure a complete and proficient education of the current cohort of residents, also considering that otolaryngology is one of many surgical specialties that are most likely to be affected by the decrease in surgical cases.
We hereby describe the first experience showing an objective decrease in clinical and surgical activity secondary to the COVID-19 pandemic. There are concerns worldwide relating topostgraduate education and safety, Cai et al[11] performed a survey study evaluating 82 residents from 51 programs, and showed that 98% of the American programs enacted policy changesincluding a reduction in resident staffing surgeries, filtered respirator use for aerosol-generating procedures, and reduced frequency of tracheostomy care. Even though most of the residents surveyed felt satisfied with their department’s measures, they felt they were at greater risk than the attendants to get infected. However, procedures and surgeries performed were not evaluated.
This study’s limitations include the short period of evaluation (one month), lack of follow-up during the pandemic, and the lack of data regarding comparisons for functional endoscopic sinus surgery and head and neck oncology, because of incomplete data logs in those specific areas.
Conclusions
The COVID-19 pandemic is a new, aggressive, and long-lasting problem. There is no certainty regarding how deeply it will affect residency training. We show a sharp decrease in exposure to patients, procedures, and surgeries in otolaryngology. Further measures and close follow-up are required to cope with this ongoing adversity. Residency programs, with the support of the sanitary authorities, need to modify their current curricula to ensure resident safety and educational opportunities during the COVID-19 pandemic.
Appendix
Appendix: Survey “Education opportunities in the Otolaryngology training program during the COVID-19 Pandemic”.

