Research papers
← vista completaPublished on October 25, 2022 | http://doi.org/10.5867/medwave.2022.09.2581
Epidemiological and clinical characteristics of survivors of SARS-COV-2 infection: A descriptive study
Características epidemiológicas y clínicas de sobrevivientes a infección por SARS-CoV-2: estudio descriptivo
Abstract
Introduction In March 2020, the World Health Organization (WHO) declared a pandemic for coronavirus 19. Typical symptoms were fever, cough, asthenia, dyspnea, and muscle pain. Pulmonary and central nervous system compromise presented challenging characteristics for healthcare physicians. The objectives of this study were to identify epidemiological and clinical characteristics of SARS-COV-2 infection survivors in a region of Argentina and to determine differences between gender, age groups, year of infection, and evolution time since diagnosis.
Methods A descriptive and analytical cross-sectional observational study was carried out. A self-administered questionnaire was applied, which was available between August and December 2021.
Results Among 1868 individuals included, the mean age was 39.4 ± 13.9 years, and 72.8% were female. Arterial hypertension was the most frequent comorbidity (11.7%). The majority were outpatients (81.9%). The most frequent presentation symptoms at all ages were asthenia (83.7%), fever (54.9%), headache (60.8%), anosmia (64.8%), ageusia (53.2%), cough (54.4%) and myalgias (53.7%). For the 18 to 29 years old age group, the most prevalent presentation symptoms were: headache (69.4%), anosmia (69.1%), ageusia (60.2%), odynophagia (45%), and rhinitis/nasal congestion (46.9%). In the 30 to 64 years old age group, there was a higher prevalence of myalgias (55.8%), arthralgias (41%), and concentration/memory disorder (28.3%). Male showed higher prevalence of fever (64.9% versus 51.1%; p < 0.001) and pneumonia (23.5% versus 13.4%; p < 0.001). After 12 weeks from diagnosis, 38.1% of patients persisted with asthenia, 23.6% with anosmia/dysosmia, and 21.2% with concentration/memory disorders.
Conclusions Systemic symptoms were common to all age groups with coronavirus 19 disease; however, younger, and intermediate age groups presented a higher prevalence of central nervous system symptoms such as anosmia and cognitive disorders, respectively. Symptoms beyond 12 weeks of diagnosis reached slightly more than 10% of the participants.
Main messages
- COVID-19 is showing a more prolonged evolution than it appeared, with the appearance of different clinical pictures, which are very important to know and address. This also occurs in asymptomatic patients, which poses a subsequent health challenge.
- Given the recent appearance of coronavirus 19 disease, it is necessary to know its potential distinctive patterns and associated factors in order to act more rapidly from pharmacological and non-pharmacological intervention.
- This work has limitations such as reporting and temporality bias, as the data are self-reported; over- and under-representation of populations when disseminated through social networks; and participation or self-selection bias, among others.
Introduction
Since December 2019, a series of unexplained cases of severe pneumonia have been reported in Wuhan, China. This finding was quickly attributed to infection by a new coronavirus, coronavirus 2 (2019-nCoV) [1,2]. On February 11th, the World Health Organization (WHO) formally named it: coronavirus disease 2019 (COVID-19). On February 23rd, there were 77 041 confirmed cases of SARS-CoV-2 infection in China [1,3]. Finally, in March 2020, the COVID-19 disease was declared a pandemic by WHO [4].
Currently, the number of patients with COVID-19 is increasing dramatically in different countries, including Argentina. The worldwide figure is approximately 42 017 per million inhabitants [5]. In Argentina, the first case of COVID-19 was confirmed on March 3rd, 2020 [6]. About 97.5% of patients who develop symptoms do so within 11.5 days of infection. The most common are fever (83 to 98%), cough (50 to 82%), asthenia (25 to 44%), dyspnea (19 to 55%), and muscle pain (11 to 44%). Mild or asymptomatic cases are the most frequent. Some patients may present sputum production, rhinorrhea, chest tightness, odynophagia, nausea, vomiting, diarrhea, headache, ageusia, and anosmia a few days before the onset of fever, suggesting that fever is critical but not the only initial symptom of infection [7,8]. However, symptomatology varied from cohort to cohort according to the regions studied [9].
Clinical and epidemiological characteristics of this disease have been updated in recent months [10]. Initially, the most relevant ones were in China [11] and different countries where infection curves were high at the beginning of the pandemic [12,13,14,15,16]. Case series were also published in Argentina, where findings similar to those mentioned above were observed [17]. The appearance of more cases strengthened our understanding of this new disease and its multiple characteristics, such as pneumonia secondary to severe acute respiratory syndrome due to coronavirus 2 (SARS-CoV-2), with the form of presentation called "happy hypoxemia" [18,19], in which, despite hypoxemia was observed in all the affected patients, they had no sensation of dyspnea. Pulmonary and central nervous system affection [20,21] presented a challenge for clinicians. Therefore, knowing potential distinctive patterns and factors associated with this disease may help us deliver a faster pharmacologic and nonpharmacologic intervention. In addition, the disease is showing a much more prolonged course than expected, and with this, different clinical pictures are emerging, which are crucial to know and address [22,23]. This is happening even in asymptomatic patients, thus posing a further challenge [24,25,26].
This study’s objectives were to identify epidemiological and clinical characteristics of SARS-COV-2 infection survivors in a region of Argentina and to determine differences between gender, age groups, year of infection, and evolution time since diagnosis.
Methods
We conducted a descriptive and analytical cross-sectional observational study using a self-administered questionnaire (see supplementary material: https://drive.google.com/file/d/1CUCna7yaW7jpP1_USfudphfS4yGxNQ6m/view?usp=sharing), adapted from: https://covid-long.com/spanish/ and previously pilot-tested on 40 volunteers. It was distributed through social networks (Facebook: profile of Lecciones en Epidemiologia, site belonging to the Facultad de Ciencias Médicas de la Universidad Nacional del Comahue, Twitter: account belonging to the Cátedra de Fisiopatología de la Facultad de Ciencias Médicas de la Universidad Nacional del Comahue), telephone contacts and emails of patients with COVID-19 diagnosis, who were under home follow-up by the team of researchers of this study.
The questionnaire covered the following variables:
Participants were included according to the following selection criteria:
Ethics
This study was developed following the ethical guidelines of the Helsinki declaration (2013 version), CIOMS 2016 guidelines (guideline 22), and Ministerial Resolution 1480/11 (Argentina).
Informed consent headed the questionnaire (see supplementary material: https://drive.google.com/file/d/1CUCna7yaW7jpP1_USfudphfS4yGxNQ6m/view?usp=sharing). The participant was considered to consent if he/she completed and sent it by email. The study was approved by the Board of Directors of the Faculty of Medical Sciences of the Universidad Nacional del Comahue (identifierID: Resolution #110/21, August 24th, 2021), by the Commission of Ethics and Evaluation of Research Projects in Human Health of the province of Río Negro, (identifierID: Resolution 6301/21, September 3rd, 2021) and by the Ethics Committee for Scientific and Technological Research of the Universidad Abierta Interamericana (identifierID: Opinion #0-1075, September 27th, 2021).
Sample size
The sample was of the non-probabilistic casual type in relation to the individuals who agreed to answer. The sample size was estimated at 1655 cases, assuming the presence of 66% of the symptom fever (a midpoint of the prevalences published for Europe, Asia, and America) because it is one of the most prevalent symptoms in the presentation of the disease [26]. We worked with a margin of error of 5% and a confidence of 95%.
The questionnaire was available between August and December 2021.
The participants resided in the Ciudad Autónoma of Buenos Aires and the province of Rio Negro.
Non-response could not be estimated, given the dissemination characteristics of the data collection tool.
Statistical analysis
Nominal variables (sex, age, comorbidities, smoking, physical activity, previous immunosuppressive medication, method of diagnosis, presenting symptoms, hospitalization requirement, oxygen therapy, mechanical ventilation, medication received, probable site of infection, vaccination status prior to infection) are summarized as absolute frequency distribution, percentages and 95% confidence interval CI of the proportion. Quantitative variables (age and body mass index) are summarized as mean, standard deviation, range, and 95% confidence interval CI of the mean.
The following comparisons were performed:
-
Demographics: (gender, age, weight, height, comorbidities, smoking and physical activity, and previous immunosuppressive medication (including corticosteroids, cyclophosphamide, cyclosporine, azathioprine, and mycophenolate).
-
COVID-19 conditions: diagnostic method, presenting symptoms, diagnosis of pneumonia defined as the affirmative answer to the questions on pneumonia and confirmatory study (by chest X-ray and, or chest tomography), duration of symptoms, hospitalization requirement, hospitalization in a general ward with oxygen, hospitalization in intensive care with mechanical ventilation, medication received, persistent symptoms, probable place of infection, vaccination status prior to infection and date of infection.
-
Having had SARS-CoV-2 infection documented by positive quantitative polymerase chain reaction retrotranscription tests (RT-qPCR + test) or clinical and epidemiological criteria, positive rapid antigen test, or positive anti-SARS-CoV-2 antibodies.
-
Age greater than or equal to 18 years.
-
Residence in the geographical area covered by the pertinent authorizations according to the legislation in force (Ciudad Autónoma de Buenos Aires and the Province of Río Negro).
-
Consent to participate in this study.
-
Comorbidities, smoking, physical activity, previous immunosuppressive medication, method of diagnosis, presenting symptoms, hospitalization requirement, hospitalization in a general ward with oxygen requirements, hospitalization in intensive care with mechanical ventilation requirements, medication received, probable site of infection, vaccination prior to infection by age and sex.
-
Persistent symptoms by recovery time.
Comparisons were made employing bivariate absolute and percentage frequency distributions and χ2 calculation (in the case of qualitative variables).
Results
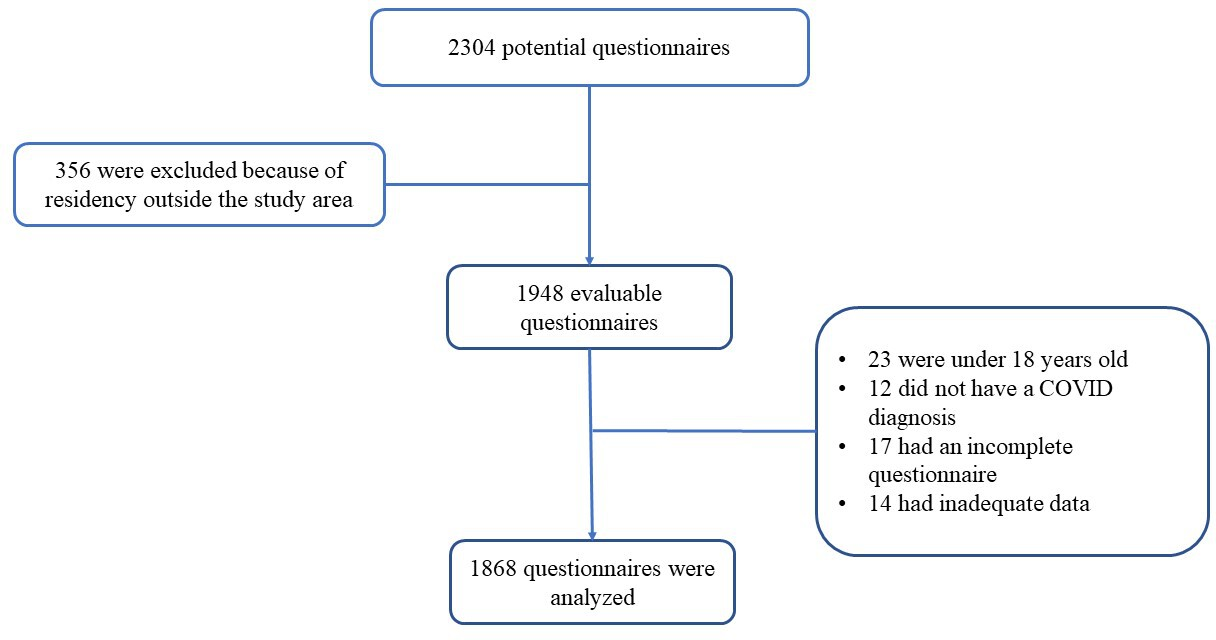
Following the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines for observational studies, 1868 questionnaires meeting all defined selection criteria and with complete data were analyzed (Figure 1).
Participant flow diagram.
Demographic and clinical characteristics are shown in Table 1. Among the 1868 individuals included in the analysis, the mean age was 39.4 ± 13.9 years. Regarding gender, 72.8% (1353) of the participants were female.
Gender comparison
Mean age in females was significantly lower than in males (41.8 ± 14.7 years versus 38.6 ± 13.5 years; t = 4.102, p < 0.001). In relation to presenting symptoms, females had a higher prevalence mainly of asthenia (84.9% versus 80.7%; χ2 = 4.854, p = 0.028), dyspnea (37.1% versus 32.1%; χ2 = 4.035, p = 0.045), odynophagia (39% versus 30.1%; χ2 = 14.088, p < 0.001), dorsalgia (51.4% versus 44.2%; χ2 = 7.476, p = 0.006), arthralgias (39.9% versus 33.9%; χ2 = 5.667, p = 0.017), headache (63.7% versus 52.6%; χ2 = 18.982, p < 0.001), anosmia (67.3% versus 58.0%; χ2 = 14.074, p < 0.001), chest pain (26.3% versus 19.9%; χ2 = 8.068, p = 0.005), rhinitis/nasal congestion (45.1% versus 34.3%; χ2 = 17.586, p < 0.001), nausea (15.4% versus 8%; χ2 = 17.336, p < 0.001), vomiting (8.1% versus 4.4%; χ2 = 7.780, p = 0, 005), diarrhea (25.9% versus 21.3%; χ2 = 4.0089, p = 0.043), dizziness (15.4% versus 11.0%, χ2 = 5.871, p = 0.015), concentration/memory disorder (29.7% versus 20.1%; χ2 = 17.047, p < 0.001) and lower hospitalization requirement (6.4% versus 12.5%; χ2 = 20.875, p < 0.001).
Meanwhile, males showed significantly higher prevalence of fever (64.9% versus 51.1%; χ2 = 28.434, p < 0.001) and diagnosis of pneumonia (23.5% versus 13.4%; χ2 = 27.780, p < 0.001). The most used medication in both groups was paracetamol, although, in the comparison by gender, it was higher in females (67.7% versus 61.4%; χ2 = 6.571, p = 0.010). No significant difference was found in vaccination status. Finally, concerning the possible place of infection for the total number of respondents, the most frequent were family, unknown place or environment, meeting in an enclosed space, and workplace. Comparison by gender shows that the workplace was mentioned in a higher proportion by males (22.9% versus 14.0%; χ2 = 42.455, p < 0.001) and cohabiting family in a higher proportion by females (37.3% versus 27.3%; χ2 = 42.455, p < 0.001).
Age comparison
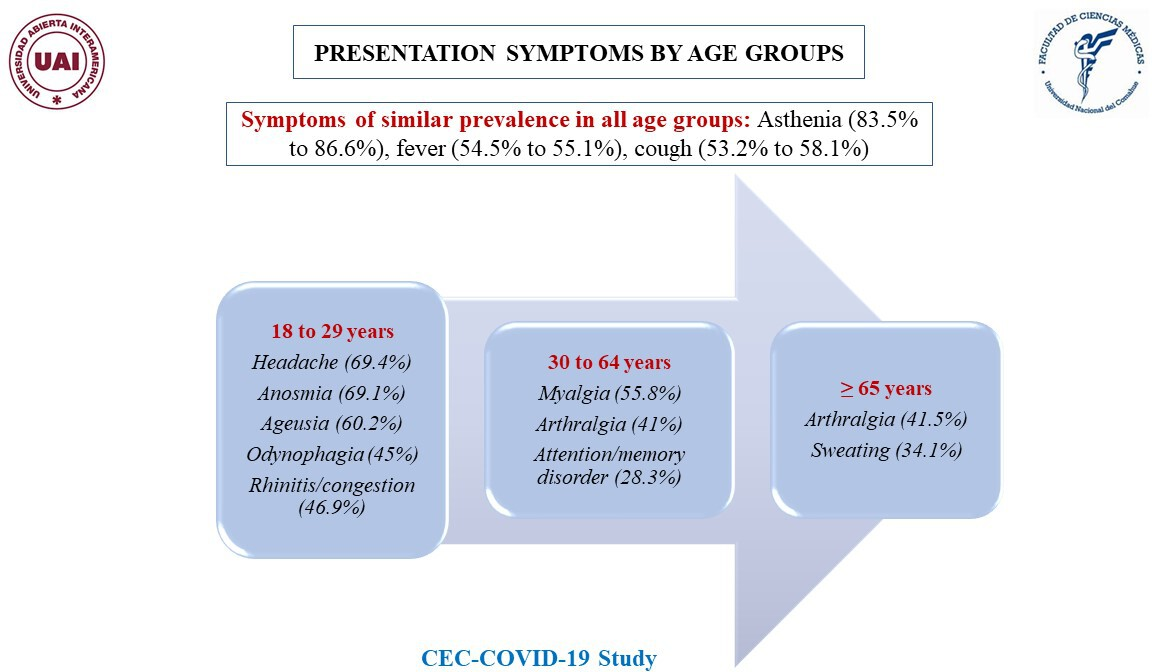
We observed a higher proportion of females in all age groups, particularly those under 65 years of age (18 to 29 years: 76.5%; 30 to 64 years: 71.9% and over 65 years: 59.8%). The most frequent comorbidity in those over 65 years of age was hypertension (57.3%), followed by diabetes (14.6%), autoimmune diseases (14.6%), and cancer (8.5%). These pathologies were of low prevalence in those under 65 years of age. Younger people, compared to the other age groups, showed a higher prevalence of smoking (16.1%) and physical activity (63.2%). The most prevalent presenting symptoms in the 18 to 29 years age group were headache (69.4%), dorsalgia (50.7%), anosmia (69.1%), ageusia (60.2%), odynophagia (45%), and rhinitis/nasal congestion (46.9%). In the 30 to 64 years age group, we observed a higher prevalence of dorsalgia (50.2%), myalgias (55.8%), arthralgias (41%), and concentration/memory disorders (28.3%). In comparison with the younger age groups, arthralgias (41.5%) and sweating (34.1%) were more frequent in those over 65 years of age (Figure 2). Symptoms such as asthenia and fever affected all age groups, showing no differences in their prevalence. The diagnosis of pneumonia was more prevalent in the older age groups (3.8% versus 20.0% versus 31.70%; χ2 = 88.238, p < 0.001).
Presentation symptoms by age group, stratified by frequency.
Hospitalization and mechanical ventilation requirements were more frequent in those over 65 years of age: 20.0% were admitted to the general ward with oxygen therapy and 4.3% to the intensive care with mechanical ventilation. The difference by age is statistically significant (χ2 = 64.789, p < 0.001). In comparison, we found that aspirin was more prescribed in patients over 65 years; the difference by age was statistically significant (2.1% vs. 5.3% vs. 9.8%; χ2 = 14.067, p = 0.001). The group under 30 years of age received more frequently paracetamol (70.4% vs. 64.9% vs. 61.0%; χ2 = 6.027, p = 0.049). Workplace transmission was more frequent in the 30 to 64 years old age group and of lesser relevance among those aged 65 years and older (11.2% vs. 20.3% vs. 3.7%: χ2 = 112.515, p < 0.001). Transmission by cohabitating relatives was more prevalent in the 18 to 29 years old age group (38.3% vs. 32.7% vs. 32.9%; χ2 = 112.515, p < 0.001). Although the highest percentage of participants were unvaccinated in all age groups at the time of infection, statistically significant differences by age were observed. The proportion of unvaccinated is lower at older ages, which is due to the availability of vaccines that initially covered older adults (89.3% vs. 75.3% vs. 61.0%; χ2 = 84.827, p < 0.001) (Table 2).
Year of infection comparison
The most prevalent symptoms in 2020 and 2021 infections included asthenia, anosmia, headache, fever, and ageusia. Dorsalgia (53.1% vs 47.4%; χ2 = 5.584, p = 0.018), arthralgias (43.8% vs 35.3%; χ2 = 12.823, p < 0.001), dyspnea (39.1% vs 33.8%; χ2 = 5.158, p = 0.023) and myalgias (57.9% vs 51.6%; χ2= 6.754, p = 0.009) were more prevalent in 2020 than 2021. While rhinitis/congestion (45.6% vs 36.2%; χ2 = 15.393, p < 0.001) and cough (57.1% vs 49.5%; χ2 = 9.915, p = 0.002) were significantly more prevalent in 2021 patients.
No difference was observed in relation to the diagnosis of pneumonia (15.6% vs 16.3%: χ2 = 0.135, p = 0.714).
Persistence of symptoms by time since onset of disease
The persistence of symptoms was analyzed in relation to weeks since the beginning of the disease, for which time was stratified into three groups: one to four weeks, five to 12 weeks, and more than 12 weeks. Most patients (1539) who completed the questionnaire had been suffering from the disease for more than 12 weeks.
The most frequent persistent symptom was asthenia, showing a statistically significant difference in the group of patients at weeks five to 12 in relation to the other groups (41.3% vs. 46.9% vs. 38.1%; χ2 = 7.483, p = 0.024).
In patients with a diagnosis of more than 12 weeks, the most frequent persistent symptoms besides asthenia were: concentration/memory disorder (26.8%), sleep disorders (24.3%), olfactory disorders (23.5%), and anxiety (21.2%).
Comparison by time elapsed showed that the following symptoms showed lower prevalence as they moved away from the date of diagnosis: ageusia /dysgeusia (28.3% vs. 20.9% vs. 15.6%; χ2 = 9.205, p = 0.010) and chest pain (13.0% vs. 10.3% vs. 6.6%; χ2 = 7.032, p = 0.030). The opposite situation was observed in relation to hair loss, which showed a higher prevalence (4.3% versus 11.0% versus 18.6%; χ2 = 15.017, p = 0.001) (Table 3).
Discussion
The objectives of this study were to determine: the epidemiological and clinical characteristics of SARS-CoV-2 infection survivors in a region of Argentina and the differences between gender, age groups, year of infection, and evolution time since diagnosis. Thus, we aim to characterize the pattern of presentation and evolution of COVID-19 disease. Even though these patients' epidemiological and clinical characteristics are well described to date, there is no clinical study describing them in Argentina in patients with mild to moderate COVID-19. It is essential to provide tools from each region, as differences in clinical presentations have been observed by region, state, country, or continent [9,26]. Most information on the clinical manifestations has come from publications in China, where fever (87% to 98.6%) and dry cough (59.4% to 67.7%) were the main symptoms associated with the disease [27,28].
This study showed that the mean age was similar to that published in European outpatient populations (39.17 ± 12.09 years) [16] aand lower than in outpatient populations in the state of Michigan, United States, where the mean age was 49.3 ± 15.7 years [29],as well as in New York City (58.0 ± 17.2 years)[30] . Certainly, the most notorious differences are in reference to those who required hospitalization, were ages older than 60 prevailed [31,32,32,33]. Assuming that comorbidities were not coexistent in the same patient, about 30% had some of those associated with worse prognosis, with arterial hypertension being the most frequently found (11.7%), mainly in males.
Presentation symptoms differed from those reported in other continents or countries, the most frequent being asthenia at 83.6% (Australia 7%), anosmia at 64.8% (Europe 47%; China 5%, Asia 12%), headache at 60.8% and fever 54.9% (China 76%; Europe 56%). [9,26].When analyzed by age, some presenting symptoms were more prevalent in younger age groups: headache, anosmia, and ageusia, exceeding the prevalence in intermediate age groups. Myalgias, arthralgias, and concentration/memory disorders were more prevalent in the latter. Finally, in those over 65 years of age, arthralgias (42%) and sweating (33.3%) were more frequent. Thus, in young age groups, the most prevalent presentation pattern was central nervous system symptoms, while in adults, it was systemic symptoms, perhaps suggesting that the tropism of the virus may vary depending on the age group. Comparison by gender showed that females had a significantly higher prevalence of central nervous system symptoms (anosmia, headache, concentration/memory disorder). On the other hand, they presented lesser upper airway symptoms (rhinitis/nasal congestion) and required less hospitalization (6.4%). Males had a higher prevalence of fever (64.9%) and required more hospitalization (12.5%). These findings resemble those of Chen J et al., where the fever was more frequent in males and nausea in females [34]. The findings previously mentioned may provide a more appropriate disease presentation pattern for our region.
Regarding the year of infection, during 2020, the most prevalent presenting symptoms, compared to those in 2021, were dorsalgia (53.1%), arthralgias (43.8%), and myalgias (57.9%); whereas rhinitis/congestion (45.6%) and cough (57.1%) were more prevalent in 2021. This difference is probably explained by the dominant variant(s) prevailing in these periods. In 2020, in Argentina, as in the rest of the world, the dominant variant was the original α variant [35], while in 2021, the dominant variants were γ, λ, and finally δ [36]. Zhenkui Hu et al. showed that individuals infected with the δ variant (B.1.617.2) presented a significantly lower prevalence of respiratory and systemic symptoms than the original strain [37].
The characterization performed in this study of COVID-19 disease showed some findings that may guide the primary care physician in differentiating it from influenza. For example, influenza shows a higher prevalence of high fever, cough, expectoration, and asthenia to a lesser degree [38,39]. Meanwhile, the findings in this population show that asthenia, anosmia, headache, and fever predominate in all age groups, unlike respiratory symptoms.
We observed that individuals who had a diagnosis of more than 12 weeks at the time of answering the questionnaire reported symptoms such as asthenia (38.1%), back pain (14.6%), arthralgias (15%), headache (19%), smell disorder (23.6%), taste disorder (15.6%), myalgias (15.1%), concentration/memory disorder (21.2%), anxiety (21.2%) and sleep disorders (24.3%). On the other hand, there is substantial variability in the literature regarding the prevalence of persistent symptoms since most publications define them from four weeks after the patient has recovered, others from 12 weeks; most of them are based on cohorts of outpatients [40,41].
It is likely that the symptoms considered relevant not only have a duration longer than three months but are also accompanied by other symptoms of lesser relevance and longer duration [42]. This has been published by Davis HE et al. for their study in which they conducted a questionnaire distributed through social networks such as Facebook and Twitter. The authors analyzed the response of 3762 participants and found more than 66 symptoms that lasted more than six months (cognitive or memory impairment affected between 55 and 60% of the participants, with no differences between age groups) [43]. In the cohort study followed by Blomberg B et al., they found that the 247 home-isolated patients with mild disease developed persistent symptoms beyond six months. Of these, 52% (32/61) of young adults aged 16 to 30 years had a loss of taste/smell (28%, 17/61), asthenia (21%, 13/61), dyspnea (13%, 8/61), concentration (13%, 8/61), and memory disorders (11%, 7/61). Symptoms such as mood disorders (26%), asthenia (80%), and perceived cognitive impairment (45%) had a negative impact on the resumption of work activities [44]. It is worth mentioning that the presence of prolonged COVID is not attributable only to a particular age group [45]. Thus, this new disease, which we call prolonged or persistent COVID, presents us with a new scenario in primary care, which we must incorporate, assuming the evolving clinical diversity.
Our study has several limitations. First, all data collected are self-reported, and questions on comorbidities were simplified to facilitate large-scale reporting. Both symptoms and diagnostic results may be subject to reporting and temporality biases, which may be relevant. Second, sampling using mainly social network dissemination will underrepresent people without appropriate devices or who are not social network users (including mostly older adult participants) and is likely to underrepresent patients severely affected by the disease. Third, although all participants underwent a consultation in a health service (they were tested for: presenting symptoms, being in contact with people with COVID-19 infection, being health care workers, or having had other circumstances that put them at risk of infection), participation in the study may have a participation bias -- also known as self-selection bias -- in which respondents with specific characteristics are more willing to participate in the research than others. Fourth, the results should be taken with caution because it was not possible to control the non-response factor as a bias due to the modality of dissemination of the questionnaire ; valid for those questionnaires that were answered through the link of the social networks mentioned, we only have the percentage of non-response in the 132 that were answered by telephone or email (percentage of non-response 2%). Fifth, we have the self-reporting bias of weight and height (for calculating body mass index) in relation to the measured parameters. However, according to published studies, the bias is based mainly on underestimation rather than overestimation [46,47], so the results in this study may show an underestimation of the number of obese people. Finally, the type of sampling would not allow robust external validity.
Conclusions
The population studied showed that at any age, the most frequent presenting symptoms were asthenia, headache, anosmia, ageusia, myalgias, and fever in more than half of the study population. In the age group between 30 and 64 years (the largest and mostly females), the most frequent symptoms were myalgias, arthralgias, and decreased concentration/memory. This may delimit a pattern of presentation in our region that may contribute to early identification and approach.
Finally, more than three-quarters of the patients with a diagnosis of more than 12 weeks still presented symptoms, being asthenia, anosmia, and decreased concentration/memory the most prevalent. This poses a new scenario, or perhaps a new disease, requiring further research to understand and address this challenge.

