Research papers
← vista completaPublished on June 29, 2017 | http://doi.org/10.5867/medwave.2017.05.6989
Medical compliance to evidence-based clinical guidelines on secondary prevention of coronary heart disease in a hospital from Lima, Peru: a retrospective study
Adherencia médica a las guías clínicas basadas en evidencia sobre prevención secundaria en enfermedad coronaria en un hospital de Lima, Perú: estudio retrospectivo
Abstract
INTRODUCTION Cardiovascular disease is the leading cause of mortality worldwide. When an acute myocardial infarction occurs, it is necessary to establish secondary prevention measures, which can reduce mortality by 50%. Clinical guidelines state that the optimal medical treatment is based upon four groups of drugs: antiplatelet drugs, statins, beta-blockers and angiotensin-converting-enzyme inhibitor or angiotensin II receptor antagonist.
OBJECTIVE To determine physician compliance to evidence-based clinical practice guidelines on secondary prevention of coronary heart disease.
METHODS Retrospective, observational study in Hospital Cayetano Heredia in Lima, Peru. The study included patients with confirmed acute coronary syndrome from February 2011 to February 2013. Medical records, laboratory results and medical therapy at discharge were collected and were compared to the American Heart Association type I, evidence level A recommendations. In addition, patient follow-up visits to the outpatient cardiology clinic at 1, 3 and 6 months after discharge were analyzed.
RESULTS The study population included 143 patients. Eighty-nine (89) patients were admitted with the diagnosis of unstable angina and non-ST-segment elevation (62.2%) and 54 had ST-segment elevation myocardial infarction (37.8%). Forty patients (28%) received all four recommended medications at discharge, which decreased at 1, 3 and 6 months after discharge to 12.6%, 7% and 3.5% respectively. The results showed a significant reduction in patient compliance to follow-up visits with a 48% reduction at the first visit to 10% on the last visit.
CONCLUSION Medical compliance to guidelines recommendations in secondary cardiovascular prevention is suboptimal with a compliance score under 50%.
Introduction
Cardiovascular disease constitutes the major cause of incapacity and death worldwide, with acute myocardial infarction being the most frequent clinical manifestation [1]. Cardiovascular risk factors initiate the atherosclerotic process which may lead to asymptomatic clinical manifestations that progressively evolve to the final stages of the disease [2]. Once complications such as acute myocardial infarction are present, measures directed at reducing the risk of recurrence and mortality must be initiated, which constitutes the objective of secondary prevention. It is estimated that these therapeutic measures may reduce mortality by 50% [3].
In 2011, the American Heart Association published the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2011 Update”, which gathers the principal recommendations about lifestyle changes, control of cardiovascular risk factors and the prescription of specific drugs with Class I Recommendation and Level of Evidence A due to their benefit in secondary prevention [4]. These drugs include: antiplatelet agents, statins, beta-blockers, and renin-angiotensin-aldosterone system modulators (angiotensin-converting-enzyme inhibitors or angiotensin II receptor antagonists) [4]. These four pharmacological groups constitute the optimal medical treatment which, despite having shown to significantly reduce recurrence and mortality [5],[6],[7],[8] are employed much less than expected. There are studies in Brazil, Korea and Australia reporting medical compliance to these recommendations between 50 and 70% [9],[10],[11].
Diverse studies recognize that physician’s knowledge and compliance with clinical practice guidelines is suboptimal [12]. Despite the healthcare system and the patient being generally held as responsible, the physician’s role is also determinant in the compliance with therapeutic practices established by clinical guidelines. The objectives of this study were to determine the adherence of physician’s prescriptions to the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease” as indicated at discharge from hospitalization and in outpatient follow-up of patients diagnosed with coronary disease; and to evaluate if the adherence of the prescription’s varied with the type of myocardial infarction, age, comorbidities (such as diabetes and hypertension) and pharmacological group.
Methods
Study design
Observational, retrospective cohort study. The clinical histories of patients who were hospitalized and followed in outpatient visits due to established coronary disease at Hospital Cayetano Heredia in Lima, Peru were reviewed during the period comprised between February 1st, 2011 and February 28th, 2013.
Population
For the identification of cases, the registry of patients hospitalized and evaluated by the Cardiology Service with the initial diagnosis of Acute Coronary Syndrome was reviewed to verify compliance with one of the established definitions in the “Third Universal Definition of Myocardial Infarction” [13],[14]. Clinical histories of patients with definitive diagnosis of ST-elevation acute myocardial infarction, non-ST-elevation acute myocardial infarction or unstable angina were consigned. Patients were catalogued with acute myocardial infarction if they met two of the following criteria: clinical, biochemical (troponin elevation) and electrocardiographic (ST segment alteration, T wave and/or new left bundle branch block), as established by the AHA Clinical Practice Guidelines [15].
Procedure
After verifying the inclusion criteria, data concerning to clinical and demographical characteristics (age, gender, blood pressure at discharge and cardiovascular risk factors such as hypertension, diabetes mellitus, obesity and smoking) were registered. Pharmacological prescriptions indicated at discharge by the hospitalization team were registered from the non-electronic health record. Pharmacological prescriptions indicated by the cardiology team during outpatient follow-up visits at the first, third and sixth month after discharge, were likewise registered. In regard to pharmacological treatment for secondary prevention, the standard considered was the recommendations in the American Heart Association’s clinical practice guidelines with recommendations type I, level of evidence A. Data from the clinical histories was blindly extracted by two investigators and the data was then verified with a cardiologist for the final registry.
Study variables
The primary study variable was the “adherence to guidelines” defined as the compliance with recommendations or protocols considered as official, recognized or elaborated by the institution [16]. In our study, this was evaluated by the percentage of discharge indications that complied with the recommendations of the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease”, which contains the recommendations with level of evidence IA pertaining to the use of antiplatelet agents, statins, beta-blockers and renin-angiotensin-aldosterone system modulators (angiotensin-converting-enzyme inhibitors or angiotensin II receptor antagonists).
In order to evaluate if some clinical or demographical characteristics of the study population werer related to the adherence to medical prescriptions, data was recollected on gender, age, diagnosis (ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, unstable angina) and cardiovascular risk factors such as, hypertension, type 2 diabetes mellitus, smoking, dyslipidemia and obesity.
Statistical analysis
The data was analyzed with the statistical package STATA version 13. Descriptive statistics were calculated as proportions and 95% confidence intervals, means and standard deviations for quantitative data. For categorical variables, the percentage of agreement between the pharmacological prescription for coronary disease and the AHA’s 2011 Clinical Guidelines recommendations. For the comparison of proportions, the exact Chi2 test was employed. Continuous variables were compared with Student’s t Test and the Wilcoxon’s sum of ranges test depending on their type of distribution. A p value ≤ 0.05 was considered for statistical significance.
Ethical considerations
This study was approved by the Ethics Committee of both, Hospital Cayetano Heredia and Universidad Peruana Cayetano Heredia; from Lima, Peru.
Results
A total of 206 patients with acute coronary syndrome were identified according to the clinical histories registry kept by the Cardiology Service, out of which 23 histories did not fulfill the diagnostic criteria, 25 were not found in the archive and 10 did not match the patient’s name in the registry. One hundred and forty-three histories remained that did comply with the inclusion criteria. Sixty nine patients had records for the first follow-up visit, 33 patients for the 3rd -month visit and 15 patients for the 6th -month visit.
Patient characteristics
The demographical and clinical characteristics of the patients are described in Table 1.
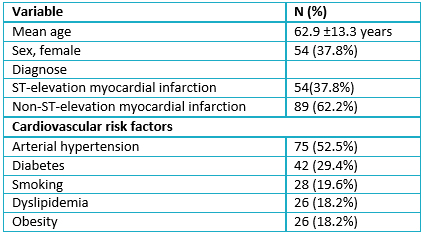 Full size
Full size Pharmacological treatment prescribed at discharge and at follow-up
The four therapeutic strategies selected for secondary prevention by the reference guideline were only indicated in 40 (28%, 95% CI: 20.8-36.1%) patients at discharge, and only in 12.6% (95% CI: 7.1-18.4%), 7% (95% CI: 3.4-12.5%) and 3.5% (95% CI: 1.1-8%) at the first, second and third follow-up outpatient visits, respectively. The proportion of patients who received the Class I Evidence Level A recommendations stipulated in the AHA’s clinical practice guidelines were as follows: antiplatelet agents (as monotherapy or combined) were the most prescribed, in 125 (87.4%, 95% CI: 80-92.5%) patients. Statins were prescribed in 109 (76.2%, 95% CI: 67-83.7%), renin-angiotensin system modulators were prescribed in 82 (57.5%, 95% CI: 45.9-68.1%). Beta-blockers were prescribed in 72 (50%, 95% CI: 37.9-62%) (Table 2).
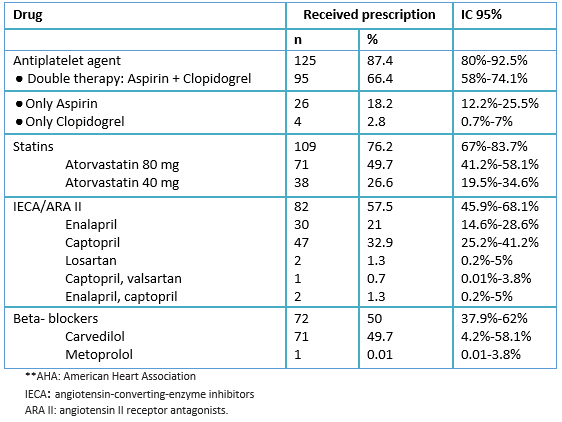 Full size
Full size The patients with ST-elevation myocardial infarction had a higher percentage of complete therapeutic prescription at discharge in comparison with non-ST-elevation myocardial infarction (46.3% vs 21.4%, p = 0.002). No statistically significant differences were found between the groups classified by hypertension and diabetes regarding the percentage of complete prescriptions at discharge. The patients who received antiplatelet agents and statins were younger than those who did not receive this indication (for antiplatelet agents: 63.1 ± 12.7 vs 68.5 ± 14.1 years, p = 0.02; for statins: 63.9 ± 13.1 vs 68.4 ± 13.7 years, p = 0.02). Association for other pharmacologic drugs was not significant.
Pharmacological treatment prescribed only in follow-up
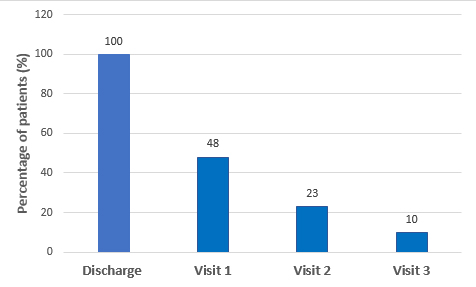
An important reduction in the patients’ adherence to outpatient follow-up visits with the Cardiology Service was observed from the first to the sixth month after discharge, from 48% (IC 9%: 39.8-56.8%) at the first visit down to 10% (95% CI: 5.9-16.7%) at the last visit (Figure 1). Aspirin and statins were the drugs most prescribed while renin-angiotensin system modulators and beta-blockers were the least prescribed at all follow-up visits (Table 3).
 Full size
Full size 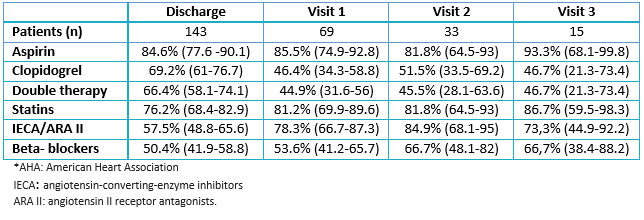 Full size
Full size Discussion
The adherence of medical prescriptions to the recommendations of the American Heart Association’s clinical practice guidelines at discharge in our study was 28%, one of the lowest reported in the literature. Similar studies have been carried out in various countries which show an adherence greater than 50%. One study carried out in New Zealand and Australia reported an adherence of 71% both in patients with a diagnosis of ST-elevation myocardial infarction and non-ST-elevation myocardial infarction; other associated factors identified were having had a cardiac catheterization during hospital admission, having had a catheterization or surgical myocardial revascularization prior to hospitalization and a past medical history of hypertension [11]. On the other hand, in Korea a study (n = 9294) found that 50.4% of patients were discharged with a prescription including the four pharmacological groups previously mentioned while the patients who had been submitted to catheterization had the highest rate of prescription and those who had been submitted to surgical myocardial revascularization, the lowest [9]. In Latin America, a study in Brazil (n = 1150) found that the proportion of patients who received the four pharmacological groups was close to 60% [10]. Thus, we can observe that compliance with the recommendations was lower in our study. This is a relevant finding for public health as measures can be taken to improve this parameter since it is known that these actions reduce mortality and the number of hospitalizations in patients with established coronary disease [3],[4].
Regarding the drugs indicated, antiplatelet agents constitute the principal pharmacological group prescribed upon discharge from hospitalization (87% of patients) with the greater percentage corresponding to double therapy (66%). These findings agree with some described in the Southeast of Asia and Malaysia where double therapy was indicated in 70% and 81.5% of patients, respectively [17],[18]. Regardless, differences about the administration of aspirin as monotherapy have been observed. In Spain, prescription of aspirin alone reaches 74% [6] and in Brazil 92% [10], showing that aspirin monotherapy is still greater that double therapy in other regions. It may be postulated that double therapy is still not prescribed in a routinely due to some physicians not taking into consideration the evidence presented in the last years or not having had access to this information [19]. On the other hand, there is still a percentage of patients that do not receive even one antiplatelet drug.
The prescription of statins in our study reaches 76%, in spite of the conclusive evidence in regard to their importance in high risk patients [16],[20], similarly to other studies [18],[21]. Beta-blockers were prescribed in 50.3% of patients upon discharge, while in Brazil and Korea the percentage of patients who receive this indication was greater [9],[10]. Our study did not register data regarding the presence of medical conditions that may contraindicate the use of these drugs, such as bradycardia, systolic hypotension, asthma or allergic reaction to this drug [22]. Angiotensin converting enzyme inhibitors and Angiotensin II receptor blockers were indicated in 57.3% of patients; a lower level than in other countries such as Brazil and Australia [10],[23]. The indication of these classes of drugs is based on the benefit for patients with diminished ventricular function, parameter which could not be evaluated in our study [16],[20].
The poor adherence of patients to outpatient follow-up visits with the Cardiology Service is notorious, with 48% of patients at the first visit and only 10% at the 6-month visit. This may be impacted by an inadequate communication between the patient and the hospitalization team at the time of discharge [24] or patients having sought an outpatient consult with other specialists such as Internists due to not having had an opportune appointment with the Cardiologist. Some studies have evaluated programs to improve adherence after discharge such as systems with text messaging or electronic reminders and a greater diffusion of investigation occurring inside the hospital [25],[26],[27]. Some of these programs may be applied in our setting. It is necessary to keep in mind that this study was carried out in an area where the majority of the population belongs to a low socioeconomic status which may have an influence on the patients’ access to health education.
Diverse factors have been identified in the literature that may have an influence on the low adherence physicians have towards clinical practice guidelines. In the first place, some studies report a lack of knowledge or familiarity with the guidelines, it could be due the quantity of information, the time one must invest in being informed or the guideline’s accessibility. Other factors must be considered, such as not agreeing with the clinical guidelines due to not considering them applicable to their patients due to cost-benefit considerations or lack of trust in the authors of the guidelines [21]. This is surprising since the hospital where this study was carried out is university affiliated which would lead one to expect a higher compliance with guidelines. Likewise, there are external factors, such as a patient’s lack of tolerance for the medication and lack of coverage of the medications by the public health insurance [21],[28].
Other factors that must be considered are the limitations of this study, including its retrospective design which does not permit determining causality in the relationship established between the variables. Another limitation is the fact that variables such as ejection fraction and clinical contraindications to specific drugs, which may have altered the number of patients who could receive a certain drug, were not included in the study registry. Likewise, 12% of patients’ clinical histories were lost which did not allow consideration of the entire sample. Lastly, the study was performed at a National Hospital in Lima, Peru which limits its external validity and the value of generalizing its findings to other realities, which is why it would be ideal to perform similar studies in other regions.
Regarding this study’s strengths, it is the first one to consider the physician’s adherence to prescription guidelines for established coronary disease in our region. Also, it constitutes an important aspect that will contribute to improvements in the follow-up of patients with coronary disease so as to diminish their risks.
Conclusions
There is a low physician compliance to clinical guidelines; 28% at discharge and 12% at first outpatient follow-up, according to our study carried out in a hospital in Lima, Peru. Secondly, antiplatelet agents (as monotherapy or combined therapy) were the most commonly prescribed pharmacological group. Thirdly, there was a 51.7% reduction in patient adherence to outpatient follow-up visits at the first visit. Since there are consequences in morbidity and mortality to the low adherence to clinical practice guidelines, studies are needed to evaluate the barriers preventing an adequate prescription and interventions that may improve physicians’ adherence to these guidelines’ recommendations.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the ethics committee of the Cayetano Heredia Hospital and the ethics committee of the Peruvian University Cayetano Heredia of Lima, Peru, was aware of this study and its possible publication in a biomedical dissemination journal.
Declaration of conflicts of interest
The authors have completed the ICMJE declaration of conflicts of interest form, and declare that they have not received funding for the report; Not having financial relationships with organizations that may have interests in the published article in the past three years; And not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

