Research papers
← vista completaPublished on January 17, 2018 | http://doi.org/10.5867/medwave.2018.01.7143
Risk factors for low birth weight according to the multiple logistic regression model. A retrospective cohort study in José María Morelos municipality, Quintana Roo, Mexico
Factores de riesgo de bajo peso al nacer según el modelo de regresión logística múltiple. Estudio de cohorte retrospectiva en el municipio José María Morelos, Quintana Roo, México
Abstract
INTRODUCTION Low birth weight has been an enigma for science over time. There have been many researches on its causes and its effects. Low birth weight is an indicator that predicts the probability of a child surviving. In fact, there is an exponential relationship between weight deficit, gestational age, and perinatal mortality. Multiple logistic regression is one of the most expressive and versatile statistical instruments available for the analysis of data in both clinical and epidemiology settings, as well as in public health.
OBJECTIVE To assess in a multivariate fashion the importance of 17 independent variables in low birth weight (dependent variable) of children born in the Mayan municipality of José María Morelos, Quintana Roo, Mexico.
METHODS Analytical observational epidemiological cohort study with retrospective temporality. Births that met the inclusion criteria occurred in the "Hospital Integral Jose Maria Morelos" of the Ministry of Health corresponding to the Maya municipality of Jose Maria Morelos during the period from August 1, 2014 to July 31, 2015. The total number of newborns recorded was 1,147; 84 of which (7.32%) had low birth weight. To estimate the independent association between the explanatory variables (potential risk factors) and the response variable, a multiple logistic regression analysis was performed using the IBM SPSS Statistics 22 software.
RESULTS In ascending numerical order values of odds ratio > 1 indicated the positive contribution of explanatory variables or possible risk factors: "unmarried" marital status (1.076, 95% confidence interval: 0.550 to 2.104); age at menarche ≤ 12 years (1.08, 95% confidence interval: 0.64 to 1.84); history of abortion(s) (1.14, 95% confidence interval: 0.44 to 2.93); maternal weight < 50 kg (1.51, 95% confidence interval: 0.83 to 2.76); number of prenatal consultations ≤ 5 (1.86, 95% confidence interval: 0.94 to 3.66); maternal age ≥ 36 years (3.5, 95% confidence interval: 0.40 to 30.47); maternal age ≤ 19 years (3.59, 95% confidence interval: 0.43 to 29.87); number of deliveries = 1 (3.86, 95% confidence interval: 0.33 to 44.85); personal pathological history (4.78, 95% confidence interval: 2.16 to 10.59); pathological obstetric history (5.01, 95% confidence interval: 1.66 to 15.18); maternal height < 150 cm (5.16, 95% confidence interval: 3.08 to 8.65); number of births ≥ 5 (5.99, 95% confidence interval: 0.51 to 69.99); and smoking (15.63, 95% confidence interval: 1.07 to 227.97).
CONCLUSIONS Four of the independent variables (personal pathological history, obstetric pathological history, maternal stature <150 centimeters and smoking) showed a significant positive contribution, thus they can be considered as clear risk factors for low birth weight. The use of the logistic regression model in the Mayan municipality of José María Morelos, will allow estimating the probability of low birth weight for each pregnant woman in the future, which will be useful for the health authorities of the region.
Introduction
Low birth weight has been an enigma for science through the ages. Multiple research works have been carried out regarding the causes that produce it and the effects it causes [1].
Birth weight is undoubtedly the most important determinant of a newborn's chances of experiencing satisfactory growth and development. Therefore, currently, the rate of newborns with low birth weight is considered a general indicator of health [2] since it is of multifactorial cause, coming from both maternal and fetal and environmental problems [3].
Usually these children have multiple problems later in the perinatal period, in childhood and even in adulthood. Among these problems are poor adaptation to the environment and different physical and mental impediments that become evident when school age arrives [4].
Low birth weight is an indicator that allows predicting the probability of survival of a child. In fact, there is an exponential relationship between weight deficit, gestational age and perinatal mortality. In addition, it is important to indicate that a percentage of full term children (37–41 weeks of gestation) who have low birth weight have different sequelae of variable severity –especially in the neurological sphere– and hence the importance of predicting the presentation of low birth weight [5],[6].
A very common problem in scientific research is to determine the effects of each of the explanatory variables in some response. In past ages it was advised that each factor be studied at the same time, with a test of statistical significance. Later, Fisher indicated that important advantages are obtained if several factors are combined in the same analysis [7].
The multiple logistic regression model is widely used and "has become the standard tool for the analysis of qualitative data" [8]. Multiple logistic regression is one of the most expressive and versatile statistical instruments available for the analysis of data in the clinical and epidemiological spheres as well as in public health. Its origin dates back to the sixties with the important work of Cornfield, Gordon & Smith on the risk of coronary heart disease [9]. Thanks to the contribution of Walker and Duncan in the subject of estimating the probability of occurrence of certain event in function of several variables [10], the multiple logistic regression evolved towards the form in which we know it today. Its use is universalized and expanded since the early eighties, mainly due to the computer facilities available since then.
The following is a history of the variables that have been considered risk factors for birth weight in different studies and that are included in ours.
Maternal ages under 20 years and over 35 years. Duanis & Neyra [11] report that maternal age ≤ 19 years represents a fundamental risk factor for children to be born with a weight < 2,500 gr. A study conducted by Liang et al. [12] reports that as maternal age increases (≥ 36 years), newborns tend to have a decreasing weight.
Maternal weight under50 kg. Fedrick & Adelstein [13] observed that women with pre–pregnancy weight < 50 kg have a higher proportion of low birth weight products than women with a higher weight.
Maternal height < 150 cm. Hernández–Cisneros et al. [2] report that an anthropometric variable that must be taken into consideration is height, since the fact that the pregnant woman has a height < 150 cm increases the risk of a child born with low birth weight.
Pathological personal history. Among the risk factors for low birth weight that have been found more frequently in studies conducted by Hernández–Cisneros et al. [2] we have high blood pressure during pregnancy and cervical vaginal sepsis. Several authors have reported the association between low birth weight and factors such as chronic hypertension [14], kidney diseases [15], thyroid diseases, cardiorespiratory diseases and autoimmune diseases [16].
Age of menarche ≤ 12 years. Harfouche [17]; Beal [18]; and Langer & Arroyo [6] report age of menarche ≤ 12 years as a risk factor for low birth weight.
Primiparity (one delivery) and multiparity (≥5 deliveries). Bergner & Susser [19] report primiparity and multiparity (≥ 5 births) as risk factors for the presentation of low birth weight. Primiparity has been associated with low birth weight in studies conducted by Silva et al. [20]. Najmi [21] reports that the history of more than five births is identified as a risk factor for low birth weight.
Antecedents of abortion. Rosell–Juarte et al. [22] report that a factor associated with low birth weight is the history of abortion(s). Abortions and previous deaths reduce birth weight by 18 and 29 g and increase the probability of low birth weight by 0.6% and 1.3%, respectively.
Obstetric pathological history. Abdulrazzaq et al. [23] report that the history of previous deliveries with low birth weight constitutes a risk factor for the development of products with low birth weight. Becerra et al. [24] found that the presence of previous perinatal death is a strong predictive factor for subsequent prematurity and low birth weight.
Low socioeconomic level. An investigation carried out by Goldenberg et al. [25] reports that low birth weight comes more frequently from mothers with unfavorable economic conditions.
Civil status "not–married". Bortman [26] reports that the risk of having children with low birth weight is associated more frequently with "unmarried" women. Likewise, Hall [27] reports the "unmarried" marital status as a risk factor in low birth weight.
Smoking. Rosell–Juarte et al. [22] point out that a risk factor of connotation in their tribute to low birth weight is smoking that exerts its negative influence both by causing prematurity and by causing intrauterine malnutrition.
Alcoholism. Among the factors that increase the probability of low birth weight have been cited the substance alcohol consumption that according to Rama–Sastry [28] together with its metabolites crosses the placenta and acts on the fetus producing in 84% of cases, according to Elorza [29] and Aguilar [30], deficiencies of prenatal and postnatal growths that explain a birth weight lower than gestational age and the poor response to nutritional intervention during childhood.
Starting prenatal care at or after week 20 of pregnancy. Arias & Tomich [31] report the start of prenatal care at or after week 20 of pregnancy as a risk factor associated with the presentation of low birth weight. Cabrales–Escobar et al. [32] revealed a statistically significant association between low birth weight and late pregnancy control (after the first 14 weeks).
Number of prenatal consultations under six. Arias & Tomich [31] report ≤ 5 prenatal consultations as a risk factor associated with the presentation of low birth weight. Halpern et al. [33] report that low birth weight is associated with both prenatal care initiated late (after the 13th week of gestation) and by an insufficient number of prenatal visits (< 6).
Female gender of the product. Research papers by van den Berg [34] report the female gender of the product as a risk factor associated with low birth weight. A study conducted by Jewell et al. [35] reports that, as expected, boys at birth weight an average of 111 g more than girls, thus reducing the probability of being born with low birth weight.
The general objective of the present study is to evaluate, in a multivariate manner, the specific weights of 17 independent variables in the low birth weight (dependent variable) of products born in the Mayan municipality of Jose Maria Morelos, Quintana Roo, Mexico.
The specific objectives were:
- To evaluate the independent contribution of each of the 17 explanatory variables in low birth weight through the estimated coefficients of the multiple logistic regression model and the corresponding odds ratio values.
- Estimate the logistic regression function that allows estimating the probability of a pregnancy ending with a child with low birth weight from the values of certain factors that act as independent variables or explanatory variables.
In summary, using the multiple logistic regression model, the present work was aimed at estimating the coefficients of 17 independent variables with data of children born in the Mayan municipality of José María Morelos, Quintana Roo, Mexico and their mothers. Its ultimate purpose is to detect those explanatory variables or risk factors that could be modified through public health interventions, health education programs and changes towards healthy lifestyles while having a function (estimated locally) that allows estimating the probability of low birth weight of a mother's product based on the values of its explanatory variables.
Methods
Epistemic approach
Quantitative, empirical–inductive, probabilistic, positivist, neopositivist or logical atomist approach [36].
Study design
Analytic observational epidemiological cohort study with retrospective temporality [37].
Inclusion criteria
Newborns between 37 and 41 weeks of gestation were included, born in the Integral José María Morelos Hospital of the Ministry of Health, during the period from August 1, 2014 to July 31, 2015.
Exclusion criteria
Multiple births, newborns with congenital diseases (for example: Down syndrome) and newborns who did not have all the information required during the period between August 1, 2014 and July 31, 2015.
Sample
Births (which met the inclusion criteria) occurred at the Integral José María Morelos Hospital of the Ministry of Health, corresponding to the Mayan municipality of José María Morelos, during the period from August 1, 2014 to July 31, 2015. The total number of registered newborns was 1,147, with 84 (7.32%) children with low weight and 1063 (92.68%) with normal weight (greater or equal to 2,500 grams).
The Mexican state of Quintana Roo is divided into 11 municipalities, seven of which (Benito Juarez, Cozumel, Felipe Carrillo Puerto, Isla Mujeres, Jose Maria Morelos, Lazaro Cardenas and Othon Pompeyo Blanco) were created on October 8, 1974 jointly with the elevation to the rank of "Free and Sovereign State" of the old "Federal Territory of Quintana Roo"; the eighth municipality, Solidaridad, was created in 1993; the ninth municipality, Tulum, in 2008; the tenth municipality, Bacalar, in 2011; and the eleventh municipality, Puerto Morelos, in November 2015 [38].
Operational definitions of the variables
- Maternal age. Period of time elapsed from the date of birth of the mother until the date of delivery. It was registered in years. Maternal ages ≤ 19 and ≥ 36 years were considered as possible risk factors
- Maternal weight. Amount of mass that houses the body of a person. It was registered in kilograms. A maternal weight at the beginning of pregnancy <50 kilograms was considered a possible risk factor.
- Maternal stature. Height of a person measured from the feet to the head. It was registered in cm. A maternal stature < 150 cm was considered a possible risk factor.
- Pathological personal history. It was recorded as "yes" or as "no". A pathological personal history was considered a possible risk factor.
- Age at menarche. Age at which the first menstrual cycle was presented. It was registered in years past. An age at menarche ≤ 12 years was considered a possible risk factor.
- Parity. Number of pregnancies reaching viable gestational age of the mother, including the current one. Possible risk factors were one childbirth (primiparity) and ≥ 5 births (multiparity).
- Abortion(s) history. Interruption of pregnancy due to natural causes or deliberately provoked. It was registered as "yes" or as "no". A history of abortion(s) was considered a possible risk factor.
- Pathological obstetric history. They were recorded as "yes" or as "no". A pathological obstetric history was considered a possible risk factor.
- Socioeconomic level. Level of well–being of a household, that is, the level at which the needs of a family are met. It was registered as "low" or as "medium". A low socioeconomic level was considered a possible risk factor.
To determine the socioeconomic level, the state health services that provide medical-care services through their units, apply the tab that contains the classification of the different services with six levels of "recovery fees" for each service. These levels are applied based on the score that results from the socioeconomic tab established at the national level as follows:
0–3 points: "Exention"
4–6 points: "1" Low
7–9 points: "2" Low
10–12 points: "3" Low
13–17 points: "4" Low
18–21 points: "5" Medium
22–25 points: "6" High
To calculate the scores, the points obtained with each of the following aspects that make up the quality of life are added according to the scheme described below:
Family group: 10 and + members (0), from 7 to 9 members (1), from 4 to 6 members (2), from 1 to 3 members (3).
Occupation: unemployed (0), underemployed (1), worker (2), employee (3), technical (4), professional, entrepreneur or executive (5).
Income (summation of the monthly amount of income contributed by each of the productive members of the family group): no salary (0), less than the minimum wage (1), minimum wage (2), more than the minimum wage (3), from 2 to 3 minimum wages (4), from 4 to 5 minimum wages (5).
Economic situation: indigent, has no income to solve basic needs (0); deficit, up to 99% of expenses can be covered (1); balance, 100% of expenses can be covered, without surplus (2); solvent, covers basic needs, has availability for savings or unforeseen expenses and has a surplus of up to 25% of your income (3); surplus, has an excessive provision of resources to cover expenses and a surplus of more than 25% of income with respect to its expense (4).
Type of housing: without housing (0), jacal or hut (1), neighborhood or improvised room (2), popular house or apartment (3), residential house or apartment (4)
Number of bedrooms: one room (0), one bedroom (1), two bedrooms (2), three bedrooms (3), four or more bedrooms (4).
- Civil status. Situation in which a person is according to his or her circumstances and legislation and to which the law grants certain legal effects. It was registered as single, married, divorced, separated, free union and widow. Subsequently, the single, divorced, separated, free union and widowed civil status were recoded as "unmarried". The "unmarried" marital status was considered a possible risk factor.
- Smoking. It was registered as "yes" (smoking ≥ 10 cigarettes per day) or as "no". “Yes was considered a possible risk factor.
- Alcoholism. It was registered as "yes" (drinking a beer daily, or drinking intoxicating drinks at least three times a week) or as "no". “Yes” was considered a possible risk factor.
- Week of gestation at the beginning of prenatal care. It is measured in weeks, from the first day of the woman's last menstrual cycle to the current date. It was registered as "from or after week 20 of pregnancy" or as "before week 20 of gestation". "From or after week 20 of gestation" was considered a possible risk factor
- Number of prenatal consultations. It was recorded as "≤ 5 prenatal consultations" or as "≥ 6 prenatal consultations". It was considered a possible risk factor to have "≤ 5 prenatal consultations".
- Product´s gender. It was registered as "masculine" or as "feminine". The "feminine" gender of the newborn was considered a possible risk factor.
Table 1 shows the dependent variable and the independent variables according to their recoding for the multiple logistic regression analysis.
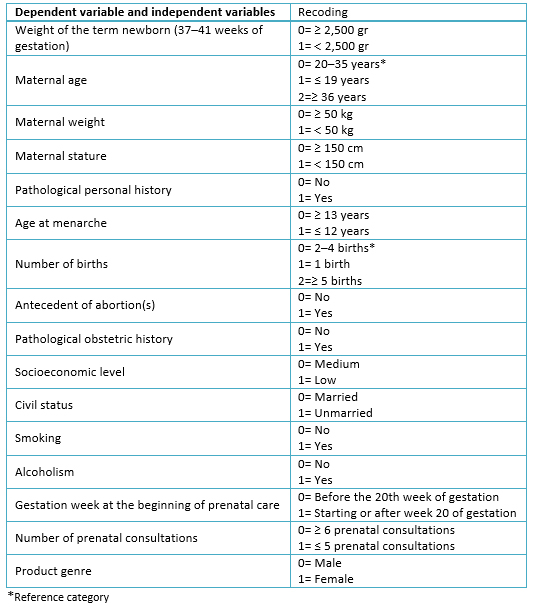 Full size
Full size Data processing
Data were collected from the Medical Records Department of the "Hospital Integral Jose Maria Morelos" of the Ministry of Health during the study period. These data were collected from the clinical records of the newborns and the clinical records of the mothers.
The data was reviewed (quality control of the information); classified and recoded according to the scheme presented in Table 1. For the elaboration of the figures, Microsoft Office Excel 2007 software was used. Finally, to estimate the independent association between the explanatory variables (potential risk factors) and the response variable (effect), a multiple logistic regression analysis was performed using the IBM SPSS Statistics 22 software. The level of significance was accepted as 0.05.
On the multiple logistic regression model [39]
The multiple logistic regression model used in the study is summarized with the following formula
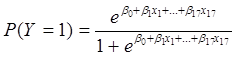
Where:
P (Y = 1) = Likelihood of being born with low weight; the "xi" represents the values of the independent variables with i = 1, 2,..., 17.
The estimations of the parameters β of the model are obtained by maximum likelihood method, these estimations allow in turn to estimate the probability of low birth weight in a given woman, substituting in the formula the values of x for the value presented by the given woman.
The logistic regression model is presented very often in the following formula:
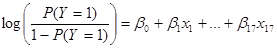
or similarly:
From this presentation way, it is easy to understand the meaning of the odds ratio since
is also known as the odds of P(Y=1), in this case odds of low birth weight (probability of low birth weight/probability of no low birth weight). It can be shown with relative ease that eβi represents the odds ratio that allows the comparison of two categories of the corresponding explanatory variable i, when the others remain constant.
Therefore, to compare two excluding categories of the explanatory variables the odds ratio is used. With the logistic regression equation we have that, if an explanatory variable is dichotomous, like all those included in this study, the category that is considered a risk factor is coded as 1 and the other category is coded 0, eβi is the odds ratio equivalent to low birth weight odds in the category coded as 1 divided by the low birthweight odds in the coded category 0. For example, if the variable "maternal weight" is the variable x2, eβ2 represents the odds of low weight in mothers with weight less than 50 kg divided by the odds of low birth weight in mothers with weight greater than or equal to 50 kg, when the other variables do not vary. In addition, as is known, every logistic coefficient (β) with a negative value gives rise to a value of the odds ratio < 1.
To estimate the probability of low birth weight for the product of a given mother, the estimated values of the coefficients of the logistic function are used and the value corresponding to the given mother and her product (for sex that it is the only child variable included). That is, x = 1 if the factor is present and x = 0 if it is absent.
Ethical aspects
The data were collected in the Medical Records Department of the "Hospital Integral Jose Maria Morelos". These data were collected from the clinical records of the newborns and from the clinical records of the mothers with the authorization of the hospital management. No information was extracted from the files that would allow the mother or the child to be identified.
Results
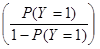
The results of the multiple logistic regression analysis are presented in Table 2. Of the 17 independent variables studied, 13 (76.47%) resulted with values of odds ratio > 1 and four (23.53%) with values of odds ratio < 1.
 Full size
Full size Four of the 13 independent variables with odds ratio values > 1 had coefficients significantly greater than 0 (significant positive contribution): maternal stature less than 150 cm (odds ratio = 5.160, 95% confidence interval: 3.08 to 8.65); pathological personal history (odds ratio = 4.78, 95% confidence interval: 2.16 to 10.59); pathological obstetric history (odds ratio = 5.01, 95% confidence interval: 1.66 to 15.18) and smoking (odds ratio = 15.63, 95% confidence interval: 1.07 to 227.97 ). These four variables showed an associated p value <0.05 (Table 2).
In the same order of things, nine of the 13 independent variables with values of odds ratio > 1 were not statistically significant (non-significant positive contribution). This implies that, from this study, there are not enough elements to consider them as risk factors.
The four independent variables that resulted with values of odds ratio < 1 (negative contribution) were: alcoholism, low socioeconomic level, beginning of prenatal care on or after gestation week 20, and female sex of the product. None of these variables reached a coefficient significantly different from 0. In particular, alcoholism showed a coefficient greater than 11,000 that resulted in an odds ratio lower than 0.0005, probably due to a very low number of women with alcoholism such as it is defined for the study (Table 2).
The Hosmer–Lemeshow test is a distribution contrast. The null hypothesis (H0) is that there are no differences between the observed values and the expected values given by the model. The alternative hypothesis (H1) is that there are or do exist differences between the observed values and the expected values. Consequently, the rejection of the null hypothesis here indicates that the model is not well adjusted [40]. In the present study, the p value for her test was 0.873. Consequently, the null hypothesis (H0) is not rejected and thus the model is not rejected for lack of adjustment. Indicating that there are no elements to think that this multiple logistic regression model is not suitable for the data of the 18 variables (one dependent variable and 17 independent variables) measured in the 1,147 newborns studied (x² = 3.821, df = 8; p = 0.873).
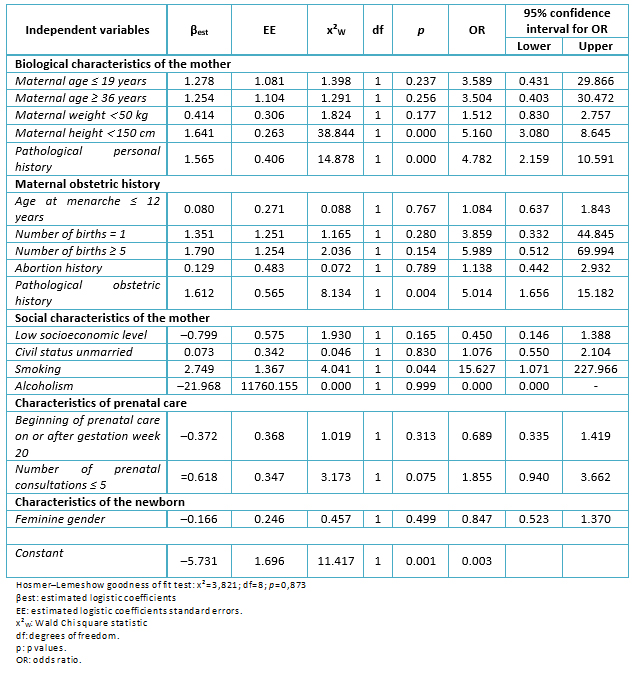
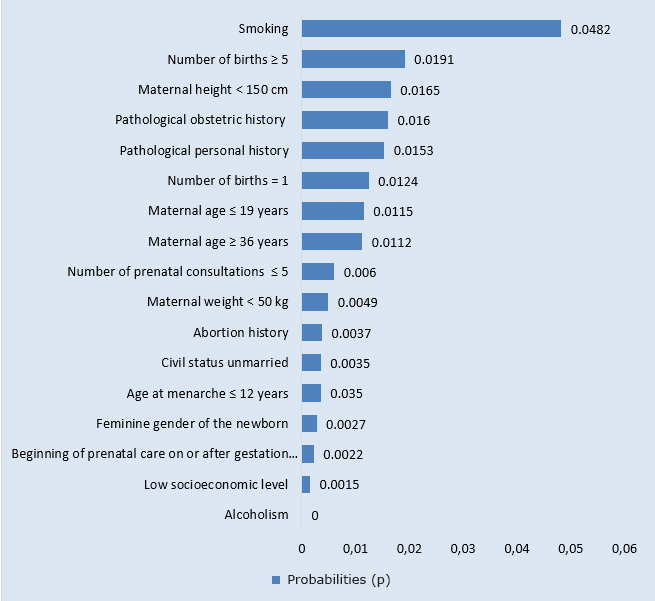
Figure 1 shows the values of the odds ratios in ascending numerical order according to the 17 independent variables.
 Full size
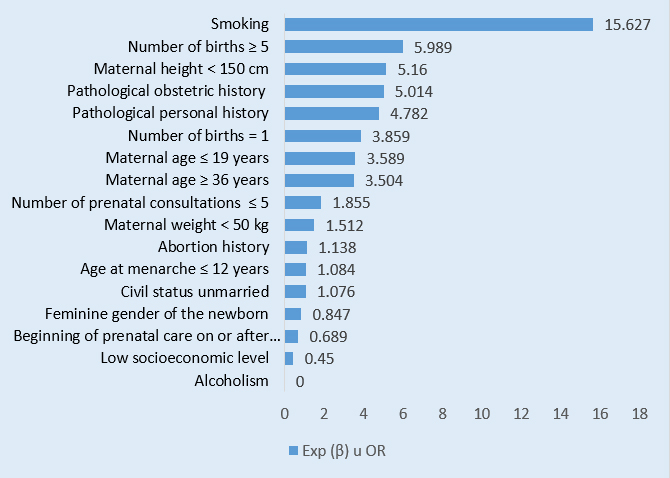
Full size With the coefficients of the model, the probabilities of having a child underweight for women who presented only that risk factor were estimated. The values of these probability estimates, in numerical ascending order, for each of the 17 independent variables or potential risk factors, are presented in Table 3.
 Full size
Full size The probability of having a low birth weight child in a female smoker is estimated at 0.05 (5%), indicating the importance of this risk factor, with respect to the others.
 Full size
Full size Discussion
Regarding the general objective, the contribution of 17 explanatory variables in low birth weight (dependent variable or response variable), in children born in the Mayan municipality of José María Morelos, was evaluated in a multivariate manner (considering each variable independent of the others), Quintana Roo, Mexico.
Regarding the first specific objective, the Exp(β) or odds ratio values of the multiple logistic regression model were used to evaluate the contribution (positive, negative or null) of each of the 17 independent variables. Thirteen of the 17 independent variables resulted with values of Exp (β) or odds ratio> 1, which indicates a positive contribution in low birth weight, for this sample. Only four of these variables could be considered risk factors.
With reference to the second specific objective, the values of the estimated logistic coefficients (β) were used for the development of the multiple logistic regression model in order to estimate the probability of occurrence of the response variable (low birth weight) in mothers with only that possible risk factor for each of the 13 explanatory variables that resulted with odds ratio > 1.
The hypothetically risk factors for low birth weight found in the Mayan municipality of José María Morelos and that can be modified through public health interventions, health education programs and changes to healthy lifestyles are:
- Civil status "unmarried".
- Maternal weight < 50 kilograms.
- Number of prenatal consultations ≤ 5.
- Maternal age ≥ 36 years.
- Maternal age ≤ 19 years.
- Number of deliveries (births) ≥ 5.
- Smoking.
A research paper [41] reports the multivariate evaluation of 19 independent variables in low birth weight, in four health service institutions (Mérida Regional Hospital of the Institute of Security and Social Services of State Workers, General Hospital Dr. Agustín O'Horán and Hospital Materno Infantil, both of the Health Service of Yucatán, and the Ignacio García Téllez National Medical Center of the Mexican Institute of Social Security of the city of Mérida, Yucatán, Mexico The total number of registered newborns was 28,282, with 3,434 (12.14%) cases and 24,848 (87.86%) controls. Due to not meeting the inclusion criteria, 2,888 (10.21%) were excluded, with 1,859 (64.67%) cases and 1,029 (35.63%) controls, and 718 (2.54%) were removed, with 414 (57.66%) cases and 304 (42.34%) controls. Consequently, 24,676 newborns were studied (87.25 %), with 1,161 (4.70%) cases and 23,515 (95.30%) controls, during the period from February 1, 2005 to January 31, 2008.
Considering the values of the odds ratio from this work, the positive contribution in ascending numerical order of the following 18 (94.74%) risk factors is recorded:
- Abdominal type of delivery or birth path.
- Beginning of prenatal care on or after week 20 of pregnancy.
- Abortion history.
- Pathological obstetric history.
- Number of prenatal consultations ≤ 5.
- Maternal age ≥ 36 years.
- Female gender of the product.
- Number of births = 1.
- Low socioeconomic level.
- Personal pathological history.
- Age at menarche ≤ 12 years.
- Marital status "unmarried".
- Smoking.
- Number of deliveries ≥ 5.
- Intergenesic interval ≤ 24 months.
- Maternal weight< 50 kilograms.
- Alcoholism.
- Maternal height < 150 centimeters.
A second research work [42] reports the multivariate evaluation of 19 independent variables on low birth weight. During the period from January 1 to December 31, 2009, births meeting the inclusion criteria were recorded, at the Hospital Clinic "C" of the Institute of Security and Social Services of State Workers; Dr. María del Socorro Quiroga Aguilar General Hospital, from the Ministry of Health of the state of Campeche; and General Hospital of Zone No 4 of the Mexican Institute of Social Security; all of them belonging to the Health Services of Isla del Carmen, Campeche, Mexico.
The total number of newborns studied was 1,174, with 85 (7.24%) low birth weight newborns and 1,089 (92.76%) who did not have this condition. All of the births met the inclusion criteria. To evaluate the specific weights of the independent variables, the odds ratio values of the multiple logistic regression model were used. Odds ratio values > 1 indicated the positive contribution in ascending numerical order of the following 14 (73.68%) variables for that sample:
- Age at menarche ≤ 12 years.
- Marital status "unmarried".
- Abortion history.
- Abdominal type of delivery or birth path.
- Maternal weight <50 kilograms.
- Number of prenatal consultations ≤ 5.
- Number of births = 1.
- Maternal age ≥ 36 years.
- Maternal age ≤ 19 years.
- Pathological obstetric history.
- Pathological personal history.
- Number of deliveries ≥ 5.
- Maternal height <150 centimeters.
- Smoking.
Conclusions
With the study, three characteristics of the mother and one of the child have been detected that can be considered risk factors for low birth weight. The generation of this new knowledge and the subsequent presentation of the final investigation report to the head of the José María Morelos Integral Hospital, is of vital importance, since the neonatology service of this health services institution will be able to help to avoid problems that newborns with low birth weight must face.
It is worth remembering that newborns with low birth weight have multiple problems later in the perinatal period, in childhood and even in adulthood. Among these problems are the poor adaptation to the environment and different physical and mental impediments that become evident when they arrive to school age [4]. In addition, it is important to indicate that a percentage of term children (between 37 and 41 weeks of gestation) who have low birth weight, suffer from sequelae of variable severity (especially in the neurological sphere). That is the importance of being able to predict the presentation of low birth weight [5],[6].
With slight variations, it can be concluded that the results obtained in this study are consistent with the results obtained in studies conducted in other geographical areas of the southeast of the Mexican Republic [41],[42].
The performance of the multiple logistic regression analysis is relevant to the objectives of the present study and not to the performance of 17 bivariate analyses. That is, 17 simple logistic regression analyzes. This is supported by Fisher [7], who reported that important advantages are obtained if all the factors are included in the same analysis, stating that "multiple bivariate comparisons are not only tedious, but, most importantly, the probability of error (global alpha) increases as the number of comparisons increases, bringing the overall probability of error to a prohibitive level".
Finally, the estimated function can be used to estimate the probability of each new mother of having a low birth weight newborn in this Mayan municipality, with local data making the predictions more valid.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the Hospital Integral José María Morelos, Quintana Roo, Mexico, was aware of this study and its possible publication in a biomedical journal.
Declaration of conflicts of interest
The authors have completed the ICMJE Conflict of Interest declaration form, and declare that they have not received funding for the report; have no financial relationships with organizations that might have an interest in the published article in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the author responsible or the editorial management of the Journal.
Financing
The authors state that they received financial support from the PROMEP Teacher Improvement Program, Mexico.
Editor's note
The principal or responsible author asserts that this manuscript is an honest, accurate and transparent transcription of the study being reported; that no important aspects of the study have been omitted; and that discrepancies between the study results and those anticipated (if relevant) have been recorded and explained.

