Research papers
← vista completaPublished on November 21, 2018 | http://doi.org/10.5867/medwave.2018.07.7336
Association between hospitalization stay and diabetic foot: an analytical cross-sectional study in three Peruvian hospitals
Asociación entre tiempo de hospitalización y pie diabético: estudio transversal analítico en tres hospitales peruanos
Abstract
Introduction Diabetic foot is one of the main complications of diabetes mellitus; however, in hospitals of provinces from Perú, the relationship of this condition with hospital stay has not been calculated.
Objective To determine the association between hospitalization time and diabetic foot in three hospitals from Cusco, Perú.
Methods A cross-sectional study of secondary data analysis was conducted. We analyzed the data of patients with type 2 diabetes mellitus admitted to the internal medicine service between January and December 2016, in three tertiary hospitals in Cusco, Peru. Correlation coefficients and p-values were calculated using generalized linear models, with Gaussian family and identity function, adjusted by intervening variables. Values of p < 0.05 were considered statistically significant.
Results Of the 153 patients, 14% (21) had a diabetic foot diagnosis, and their median age was 61 years (interquartile range 56 to 68). Those who had a diabetic foot had on average 20 hospitalization days. A strong association was found between a diabetic foot and the number of hospitalization days (17 days more, p = 0.003); adjusted by six variables. Those patients with a history of hypertension had more hospitalization days (10 days more, p = 0.011) and those admitted to a hospital of the Ministry of Health, had fewer hospitalization days (10 days less, p = 0.032).
Conclusion The group of patients with diabetic foot had a longer hospitalization time. The longer hospitalization time could be due to complications of the disease or difficulties in management.
|
Key ideas
|
Introduction
Diabetic foot is one of the most important complications of diabetes mellitus. Around 25% of affected people will develop a foot ulcer during their lifetime, being more frequent in the age group 45-65 years[1]. In Peru, a diabetes prevalence of 7% has been reported in 2012[2], as well as a mortality of 3.9% in 2014[3].
According to an epidemiological surveillance report including about 3000 patients with diabetes from different hospitals in Peru, 30% of these patients experienced some vascular complications, having diabetic foot a prevalence of 6%[2].
Diabetic foot is one of the most disabling complications of diabetes. Local institutions such as the Medical Association of Peru (Colegio Médico del Perú) have assessed this situation and are creating strategies for its better handling[4]. This complication represents a higher disease burden and additional costs to the healthcare system[5],[6]. Patients are susceptible to inadequate management, risk of limb amputation, concomitant infections, and ulcers. These events increase the morbidity and mortality of those who suffer from this disease[7], resulting in high readmission rates and longer length of hospital stay[8].
There are few published studies in the provinces of Peru associating this complication with length of hospital stay. Thus, the objective of our study was to estimate the association between length of hospital stay and having diabetic foot among patients with type 2 diabetes admitted to three hospitals in Cusco (Peru) during 2016.
Methods
Design and population
We conducted an analytical cross-sectional study involving secondary data analysis of a previously published study[9], in inpatients between 1 January to 31 December 2016 with diagnosis of type 2 diabetes in three third-level regional reference hospitals in the city of Cusco, Peru: “Adolfo Guevara Velasco” National Hospital (establishment that belongs to the social security -EsSalud- and receives monthly contributions from its policy holders as opposed to other healthcare establishments in Cusco); Regional Hospital of Cusco; and “Antonio Lorena” Hospital, both hospitals of the Peruvian Ministry of Health (providing services mainly to people with integrated health insurance). It is important to study this population because Cusco is one of the main cities in the Andes of southern Peru where local patients as well as those referred from other Andean, and even Jungle, cities are treated. The entire data found in census sampling was used.
Selection of participants
We included all patients diagnosed with type 2 diabetes hospitalized in the internal medicine service in any of the hospitals above mentioned during 2016. They were then included in two groups: i) with diagnosis of diabetic foot, and ii) with other diagnoses different to the diabetic foot. Patients admitted only to be subjected to diagnostic or therapeutic procedures (renal biopsy, peritoneal dialysis catheter placement, pulses with corticoids) were excluded.
Study variables
To determine if a patient suffered from type 2 diabetes, we used the American Diabetes Association criteria. A physician, a doctor of internal medicine or an endocrinologist confirmed the disease. This diagnosis could be done in emergency or outpatient clinic[10]. The variable of interest was having diabetic foot, which was determined with the medical diagnosis recorded in the medical chart. The length of hospital stay was considered based on the number of hospitalization days (days in bed from admission to discharge). In addition, we included socio-educational variables: sex, age and education level, and clinical variables: length of time diagnosed with type 2 diabetes, and history of hypertension. We considered these variables because of their greatest relation to diabetic foot. As this was a secondary analysis of data, we could not access other variables that could have been involved in the main association.
Data analysis
The primary database was reviewed[9], and all variables described for this study were then selected. Data was then entered into a database in Microsoft Excel (version for Windows 2013), where information was organized. At this stage, the data quality control was performed.
To analyze the data, we used the statistical program Stata v.11.1 (StataCorp LP, College Station, TX, USA). We made a descriptive analysis of categorical variables using absolute and relative frequencies. To describe numerical variables, the median and the interquartile range were used according to the previous assessment of normality assumption using the Shapiro Wilk test. A bivariate analysis was applied to compare the groups of patients with and without diabetic foot (using the Chi square test for categorical variables and the rank sum test for quantitative variables) to determine if there were differences.
Analytical statistics were generated using the variable “hospitalization days” according to the variable of interest “having diabetic foot”. For this, we calculated the correlation coefficients and p-values by using generalized linear models with Gaussian family and identity link function (this is because the main variable was quantitative – number of hospitalization days). P - values < 0.05 were considered statistically significant.
Ethics
The primary study which database was used was reviewed and approved by the Ethics and Research Committee of the hospitals where this research was conducted: Red Asistencial (Healthcare Network) de EsSalud, Cusco (N° 016-CI-GRACU-ESSALUD-2017), “Antonio Lorena” Hospital of Cusco (N° 03-2017-UDPH-HAL-C), and Regional Hospital of Cusco (N° 029-2017-HRC-DE). In addition, we followed the recommendations and guidelines for Good Clinical Practice for Medical Research involving human subjects. We removed names from databases after collecting information from every patient. An anonymous list was used for the analysis.
Results
Of the 153 patients, 13.7% (21) of inpatients were diagnosed with diabetic foot; 16.7% of male patients had diabetic foot. The median age of patients with diabetic foot was 61 years (interquartile range 56 to 68), and 16.1% of patients suffered from hypertension and diabetic foot. The median length of time with diabetes, 13 years, was higher among patients with diabetic foot (interquartile range 7 to 20). Hospitals of the Ministry of Health: Regional (27.5%) and “Antonio Lorena” (11.5%) had the greatest number of patients with diabetic foot in comparison with “Adolfo Guevara Velasco” Hospital (2.0%) (Table 1)
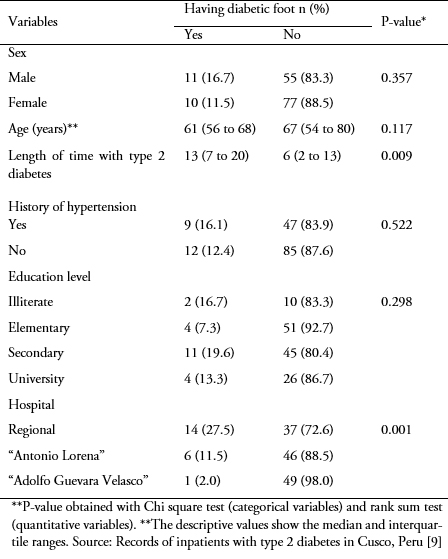 Full size
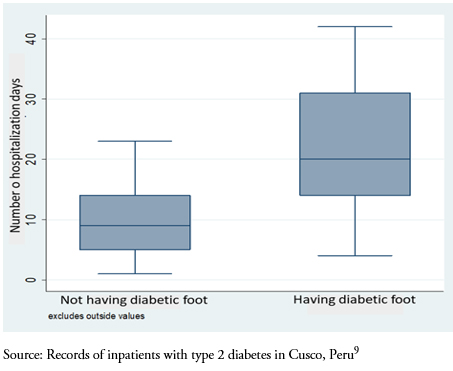
Full size The median number of hospitalization days among those with diabetic foot was 20 days (interquartile range: 14 to 31 days). For those without diabetic foot, the median was 9 days (interquartile range: 5 to 14 days) (Figure 1).
 Full size
Full size The average number of hospitalization days was 32 days. We found a significant association between having diabetic foot and the number of hospitalization days (17.0 days longer; 95% confidence interval: 5.7 to 28.3 days; p = 0.003); adjusted for six variables. Also, the number of hospitalization days for those who had a history of hypertension was higher (9.6 days longer, 95% confidence interval: 2.2 to 17.1 days; p = 0.011), and those at “Antonio Lorena” Hospital had a shorter length of hospital stay (9.6 days shorter, 95% confidence interval: 18.4 to -0.8 days; p = 0.032) (Table 2).
Discussion
According to the main finding of our research, there is a significant statistical difference in the length of hospital stay between patients with and without diabetic foot. Two systematic reviews conducted by the International Working Group on the Diabetic Foot confirm this finding[11],[12].
study in Singapore reported that the average length of hospital stays of patients with amputations due to diabetic foot was 6.5 times longer (53 days) than that of non-surgically treated diabetic patients[13]. In addition, a study in Korea reported that the average length of hospital stay was prolonged (37 days) for surgical drainage of ulcers8, and another study reported that wound severity is associated to a length of hospital stay longer than 5 weeks[14].
These studies confirm that treatment of diabetic foot involves a prolonged length of hospital stay. Therefore, it is considered a public health issue as it results in greater time and cost for a complication that can be preventable with proper education and monitoring. On the contrary, a study in the United States of America reported that the average length of hospital stay for this type of patients was 6 to 7 days in 2005-2010[15]. This may be due to the characteristics of the population itself, and better healthcare systems in the United States.
Another important finding was that the length of hospital stay was also associated with having hypertension, a concomitant disease closely linked to type 2 diabetes. According to a recent report in different Peruvian cities, hypertension is associated with type 2 diabetes, especially when it comes to drug treatment of both diseases. This report showing that there is an important number of patients who suffer from both diseases and do not receive proper treatment[16]. This has also been reported in hospitals in developed countries[17], where it has been shown that both diseases coexist in a great number of patients[18],[19]. There are reports of this association in countries such as China[20], where more than half of the patients with hypertension had also type 2 diabetes, which may be due to endothelial dysfunctions present in acute hyperglycemia[21],[22].
A study in Mexico reported an association of 47% between diabetes and hypertension[23]. Being a country with a similar context to ours, it shows the need to increase the efforts to prevent and treat non-transmissible chronic diseases in our population. As several studies state, and as shown by the Latin American consensus on hypertension in patients with type 2 diabetes and metabolic syndrome, these are the new epidemics of the 21st century[24].
The length of hospital stay was shorter in a hospital of the Ministry of Health (“Antonio Lorena”). This may be due to a lower severity of the disease of admitted patients or to a poorer management of this disease, which may show that a timely and proper management could greatly influence the outcome of many diseases[24]. We believe that it is important to promote primary prevention, especially if there are several reports in our setting showing that several groups of the economically active population are starting to have metabolic disorders[25],[26],[27], and that this may result in them being the new patients with chronic illnesses within some years.
A limitation of this study was information bias. Because this is a secondary data analysis, we couldn’t obtain additional information that could be used to adjust the association. However, most of the variables used were important for this association. In addition, we assessed different socio-economic populations (patients from hospitals of the Ministry of Health and the social security) of a province in Peru. A statistical limitation was using the variable of hospitalization days in its raw form when this should be normalized to be used with the identity link function. However, when trying to normalize it (logarithmic power), only tenths and hundredths of their values of association changed when performing the same analysis for all the variables. Thus, we decided not to normalize this variable, so it could be more easily interpreted (even though that would improve its use with the link function and residues). On the other hand, it is important to highlight that some confidence intervals were wide (for those having diabetic foot and hypertension). This may be due to a strong association between these variables and the hospitalization days, and due to the small sample size.
Conclusions
We concluded that in the study population there is a significant association between a longer length of hospital stay in Type 2 diabetic mellitus patients and having diabetic foot. In addition, that the number of hospitalization days was also associated to suffering from hypertension, and the population admitted to one of the hospitals under study.
We believe that Peruvian institutions engaged in health promotion and prevention should lead initiatives that promote better health styles, timely detection, and proper treatment of populations in risk of suffering these diseases as well as the development of financial investigations to determine health costs of this disease in our context[28],[29].
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Author contributions
CRM: conceptualization, data management, formal analysis, research, methodology, project administration, supervision, data submission, manuscript preparation (elaboration of original draft), writing (revision and editing). LP-T: conceptualization, data management, research, methodology, manuscript preparation (elaboration of original draft), writing (revision and editing). LM-C: conceptualization, data management, research, manuscript preparation (elaboration of original draft), writing (revision and editing). NA-A: research, methodology, project administration, supervision, data submission, manuscript preparation (elaboration of original draft), writing (revision and editing). EAR-A: research, project administration, writing (revision and editing). MEO-L: research, project administration, writing (revision and editing).
Competing interests
The authors have completed the ICMJE Conflict of Interest declaration form and declare that they have not received funding for the report, have no financial relationships with organizations that might have an interest in the published article in the last three years, and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the main author or the editorial management of the Journal.
Funding
The authors state that there were no external sources of funding.
Ethics statement
The primary study which database was used was reviewed and approved by the Ethics and Research Committee of the hospitals were this research was conducted: Red Asistencial (Healthcare Network) de EsSalud, Cusco (N° 016-CI-GRACU-ESSALUD-2017), “Antonio Lorena” Hospital of Cusco (N° 03-2017-UDPH-HAL-C), and Regional Hospital of Cusco (N° 029-2017-HRC-DE).
Data availability
This database is available in the Figshare data repository: https://doi.org/10.6084/m9.figshare.5606041.v1

