Research papers
← vista completaPublished on September 12, 2019 | http://doi.org/10.5867/medwave.2019.08.7694
Factors associated with vancomycin-resistant enterococci colonization in a pediatric intensive care unit of Paraguay: A cross-sectional study on hospital charts
Factores asociados a colonización por enterococo sp resistente a vancomicina en una unidad de cuidados intensivos pediátricos del Paraguay: estudio transversal sobre historias clínicas
Abstract
Introduction Vancomycin-resistant enterococci (VRE) infections have become widespread and a challenge in hospitalized patients. The threat of infection by intractable enterococci and the possibility that vancomycin resistance could involve pneumococci or staphylococci advocate for careful surveillance of resistant strains.
Objective To determine the risk factors associated with VRE colonization in pediatric patients admitted to the Pediatric Intensive Care Unit (PICU) in the period between January 2012 and June 2013.
Methods We conducted a cross-sectional study analyzing the clinical histories of 140 patients admitted to the PICU (children from 1 month to 18 years) who underwent rectal swab cultures within 48 hours of admission. We calculated the odds ratios and confidence intervals of the risk factors for VRE colonization in the PICU, and then we used multiple logistic regression for the statistically significant variables.
Results VRE colonization was present in 18.6% of patients. The following variables were identified as risk factors associated with VRE colonization: prior hospitalization in the past year (odds ratio: 10.8; 95% confidence interval: 2.43 to 47.8; p = 0.001); prior use of one broad-spectrum antibiotic (odds ratio: 5.05; 95% confidence interval: 2.04 to 12.5; p = 0.000); use of two or more broad-spectrum antibiotics in past year (odds ratio: 5.4; 95% confidence interval: 1.5 to 18.4; p = 0.009); prior hospitalization in a high-risk area (odds ratio: 4.91; 95% confidence interval: 1.83 to 13.2; p = 0.000); hospitalization for more than five days in a high-risk area (odds ratio: 5.64; 95% confidence interval: 2.18 to 14.6; p = 0.000); and use of immunosuppressant drugs (odds ratio: 4.84; 95% confidence interval: 1.92 to 11.9; p = 0.001). In a logistic multiple regression the use of two or more broad-spectrum antibiotics (odds ratio: 4.81; 95% confidence interval: 1.01 to 22.8; p = 0.047) and prior hospitalization in past year (odds ratio: 7.84; 95% confidence interval: 1.24 to 49.32; p = 0.028) were identified as independent factors statistically associated with VRE colonization.
Conclusion Pediatric patients admitted for intensive care with a history of prior hospitalization in the past year and exposure to two or more broad-spectrum antibiotics have a greater risk of colonization by vancomycin-resistant enterococci.
Introduction
The evolution of antibiotic resistance evolution has become problematic worldwide[1]. First identified in the mid-1980s, vancomycin-resistant enterococci (VRE) have intrinsic resistance to most common antibiotics, can develop resistance to most other current antibiotics, and can transfer vancomycin resistance genes to other gram-positive organisms[2],[3],[4].
The largest reservoir of VRE is the gastrointestinal tract, and the human being can be a carrier. This contributes to the dissemination of VRE in hospitals[5]. Several previous studies on VRE risk factors have found that the following variables are associated with VRE colonization: exposure to previous antibiotics; previous and prolonged hospitalizations; use of antibiotics in the year prior to admission; surgical conditions; proximity of carrier patients; and exposure to equipment contaminated with VRE[6],[7],[8],[9],[10],[11],[12]. Children colonized with VRE in the gastrointestinal tract can transmit it by fecal-oral dissemination as well as by contaminated fomites[13].
The threat of infection by intractable enterococci and the possibility that vancomycin resistance can spread from enterococci to pneumococci or staphylococci underscores the importance of improved control measures and prevention of hospital infections; careful analysis of empirical antimicrobial schemes; reductions in the length of hospital stays; and follow-up surveillance evaluating the effectiveness of these types of steps and procedures[14],[15],[16].
At the time of the study, there were no data on the prevalence of VRE infection in pediatric intensive care units (PICUs) in our setting, nor regarding the factors associated with VRE colonization. Therefore, the objective of this study is to determine the risk factors associated with the colonization of VRE in pediatric patients admitted to an intensive care unit.
Methods
Study design and setting
This cross-sectional study was carried out in patients admitted to the pediatric intensive care unit (PICU) of Clinicas Hospital at the National University of Asunción, Paraguay, between January 2012 and June 2013. Clinicas Hospital PICU is a multipurpose referral unit with eight beds that serves hospitals in the Greater Asunción area (approximately 2.5 million inhabitants). The study protocol was approved by the Universidad Nacional de Asunción (UNA) Institutional Ethics Committee. Informed consent was not required because the study consisted of a review of medical records. Confidentiality of personal data was guaranteed with the use of encrypted files exclusively managed by researchers.
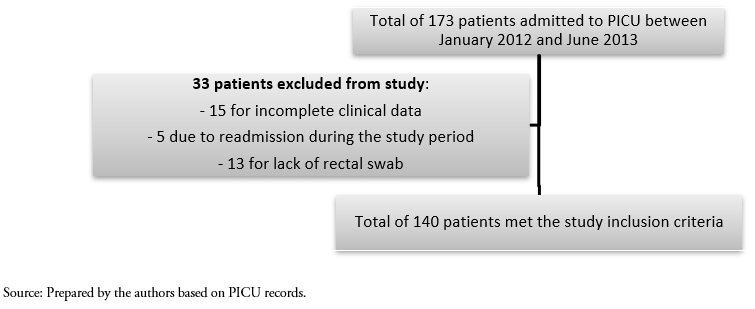
Convenience sampling was carried out using the medical records for all consecutive patients admitted to the PICU between January 2012 and June 2013. A total of 173 patients were admitted during the study period, of which 33 were excluded (15 for incomplete clinical data, 5 due to readmission during the study period, and 13 for lack of a rectal swab), resulting in a final sample of 140 patients (Figure 1).
Study sample
A total of 140 pediatric patients, ranging in age from 1 month to 18 years, were included in the study. Inclusion criteria were: 1) had a rectal swab within 48 hours of admission to the PICU to detect Enterococcus sp., with results available in the medical record; had complete medical records; and 3) admitted to the PICU during the study period. Exclusion criteria were: incomplete clinical data and not undergoing a rectal swab (which in most cases was due to lack of laboratory supplies). If a study subject was admitted to the PICU more than once, only the first admission was considered in the study.
At the time of the study, according to protocol, a rectal swab was supposed to be carried out for all PICU patients at or within 48 hours of admission. All patients were considered positive and subject to isolation until the return of the culture. Cases in which a swab was not taken had two main causes: administrative factors such as lack of supplies, or death of the patient within the first few hours of admission.
 Full size
Full size Laboratory testing
Rectal samples were collected with a wooden swab at or within 48 hours of admission to the PICU. The samples were placed in Stuart transport medium and sent to the PICU’s microbiology laboratory for cultivation in bile esculin azide agar with vancomycin (6 µg / ml).
Data analysis
Demographic and clinical variables, including age, sex, and primary or underlying diagnosis on the day of admission, were compiled from the clinical history of each patient. For the data analysis, patients were divided into two groups: positive rectal swab culture (VRE+) and negative rectal swab culture (VRE-).
Variables studied in the two groups included patients’ baseline characteristics; prior hospitalization(s) in the past year; and prior hospitalization in a high-risk area (hemato-oncology or intensive care) or a low-risk area (any other reason for pediatric hospitalization). The low- and high-risk area groups were divided into subgroups by length of hospital stay (≤ 10 days versus ≥ 11 days for low-risk areas and ≤ 5 days versus ≥ 6 days for high-risk areas).
Other variables that were analyzed included use of antibiotics in the past year and range of the antimicrobial spectrum (narrow versus broad, with the latter category including anti-infective agents with activity against both gram-positive and gram-negative bacteria). The antibiotics studied were those used in hospital settings, such as vancomycin and third generation cephalosporins (e.g., ceftriaxone or ceftazidime, as well as clindamycin, imipenem, or meropenem). Other variables that were studied included duration of exposure to or use of antibiotics (≤ 7 days versus ≥ 8 days); number of broad-spectrum antibiotics used (one versus two or more); use of invasive devices (defined as a central venous line, a bladder catheter, dialysis catheters, or mechanical ventilation); and use of immunosuppressants (defined as administration of antineoplastic therapy within 6 months prior to sampling, or prior bone marrow transplantation).
Statistical analysis
Continuous variables were expressed as mean ± standard deviation, assuming that the variables had normal distribution. Categorical variables were expressed as numbers and percentages. The t test was used to compare continuous variables and the chi-square test was used to compare categorical variables, with p < 0.05 considered significant. In the data analysis, the odds ratio and 95% confidence interval were determined for each variable. Multiple logistic regression analysis was performed on variables that were statistically significant during the bivariate relationship analysis. All statistical analysis was carried out using the EpiInfo 3.4 statistical package.
Results
A total of 140 patients met the study inclusion criteria, including admission to the PICU during the study period January 2012 to June 2013. Of these, based on the rectal swab results, 26 patients (18.6%) were positive for VRE and 114 (81.4%) were negative for VRE. No patient with a culture positive for VRE developed any disease associated with the bacteria.
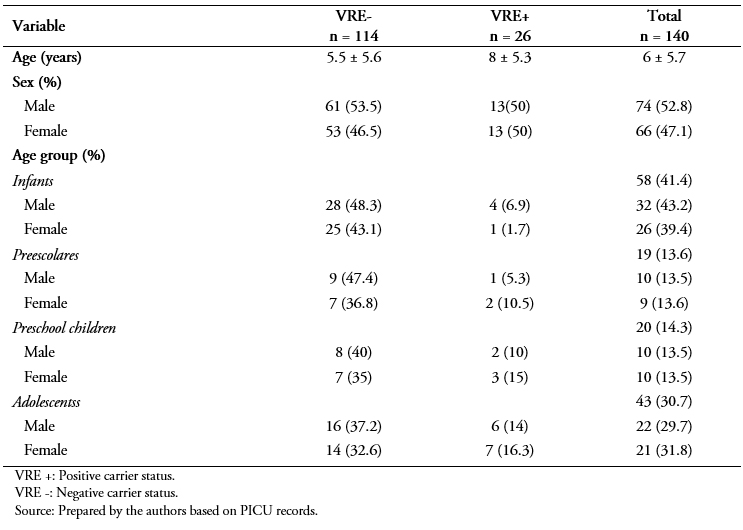
The average age for the patient sample was 6 ± 5.7 years and distribution by sex was 52.8% boys and 47.1% girls (p = 0.75) (Table 1). Patients with VRE colonization were significantly older than those without VRE colonization (8 ± 5.3 years versus 5.5 ± 5.6 years, p = 0.03) (Table 1). The frequency distribution by age group is shown in Table 1.
According to the data on comorbidities, 48 patients (34.3%) presented hematological pathologies (leukemia or lymphomas) and 21 (20%) had some type of tumor. A total of 36 patients (25.7%) did not present comorbidities. Hematological pathology (odds ratio: 5.4; 95% confidence interval: 2.2 to 13; p = 0.00) and lupus or immunodeficiencies (odds ratio: 18; 95% confidence interval: 1.8 to 18.1; p = 0.01) significantly increased the risk of VRE colonization (Table 2).
The main diagnoses for the patient sample upon admission to the PICU were shock (44 or 31.4%), postoperative conditions (17 or 12.1%), dengue (16 or 11%), and sepsis (10 or 7%) (Table 3). The frequency of the diagnoses was similar for both VRE+ and VRE- patients.
In the bivariate analysis, a statistically significant difference was observed for the following variables: previous hospitalization in past year (odds ratio: 10.8; 95% confidence interval: 2.43 to 47.8; p = 0.001); exposure to antibiotics for 8 or more days (odds ratio: 5.54; 95% confidence interval: 2.18 to 14.8; p = 0.05); exposure to two or more broad-spectrum antibiotics in the past year (odds ratio: 5.4; 95% confidence interval: 1.5 to 18.4; p = 0.009); prior hospitalization in a high-risk area (odds ratio: 4.9; 95% confidence interval: 1.83 to 11.9; p = 0.00); use of immunosuppressants (odds ratio: 4.84; 95% confidence interval: 1.95 to 11.9; p = 0.000); and hospitalization in a high-risk area for 6 or more days (odds ratio: 5.64; 95% confidence interval: 2, 18 to 14.6; p = 0.00). There were no significant differences for the following variables: antibiotic exposure for less than 7 days; no exposure to broad-spectrum antibiotics; prior hospitalization in a low-risk area in the past year; invasive procedures in the past year; and hospitalization in a low-risk area for ≤ 10 days (Table 4).
 Full size
Full size 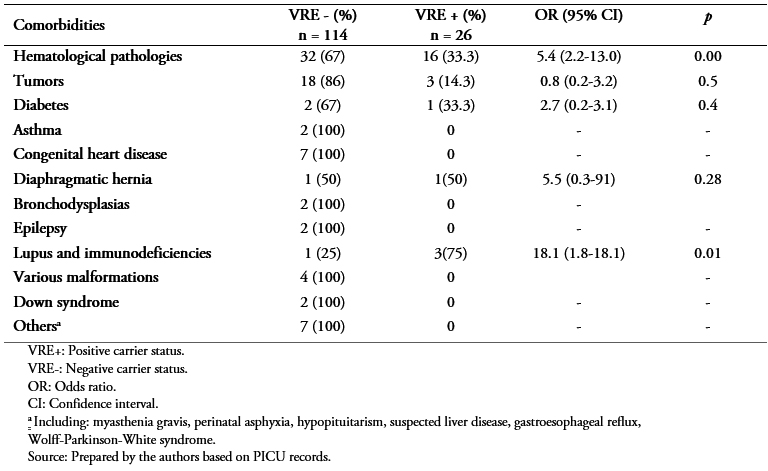 Full size
Full size 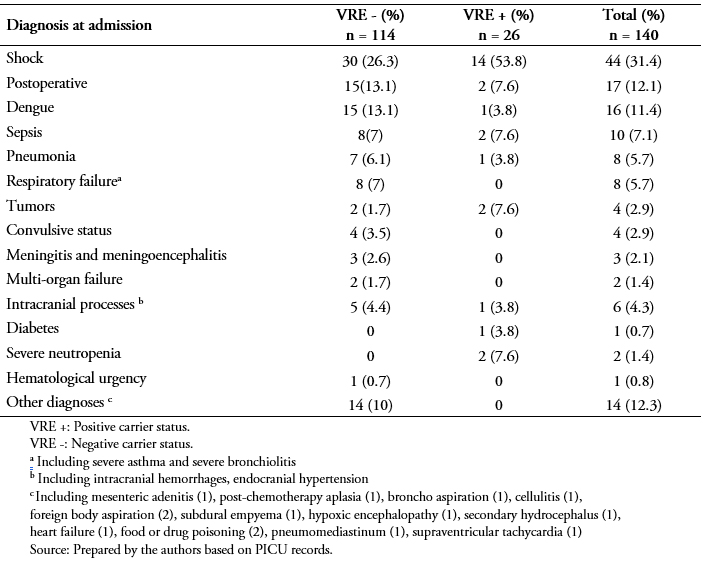 Full size
Full size 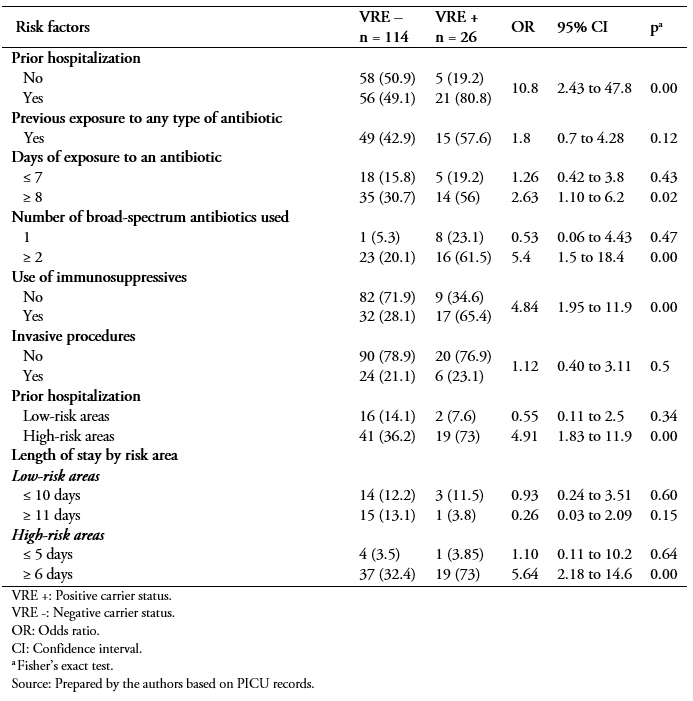 Full size
Full size The multiple logistic regression analysis for the variables that showed statistical significance is shown in Table 5. It showed that the factors associated with VRE colonization were use of two or more broad-spectrum antibiotics in the past year (odds ratio: 4.8; 95% confidence interval: 1.016 to 22.83; p = 0.04) and previous hospitalizations in past year (odds ratio: 7.84; 95% confidence interval: 1.24 to 49.32; p = 0.02).
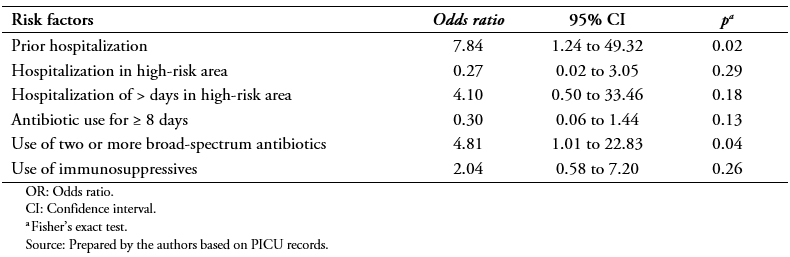 Full size
Full size Discussion
The main findings of this study were:
1) the prevalence of PICU VRE colonization was 18.6%,
2) the factors significantly associated with VRE colonization in PICU patients were prior hospitalization in past year and exposure to two or more broad-spectrum antibiotics.
In this study, 18.6% of the patients studied had VRE colonization. This frequency of colonization is similar to what was found in another study conducted in a Chilean reference hospital, outside the scope of Intensive care, in which 13% of the patients were VRE+[17].
In one study conducted in Brazil on VRE by Tresoldi et al.[4], a colonization rate of 8.0% was found. However, another study in Chile by Loyola et al. reported a VRE colonization rate of 23.1%[8]. In Argentina, Reale et al. reported a prevalence of VRE colonization of 17.9%[7]. In one study in Turkey by Sutcu et al., a 9.5% VRE colonization rate was found[18]. Another case-control study in Turkey by Ulu-Kilic et al.[19] retrospectively analyzed VRE surveillance data from a pediatric hospital for the period 2010 to 2014, and found a 3.75% rate of positive cultures among all patients examined.
In Pakistan, a study by Yameen et al. evaluating the local epidemiology of nasal and rectal VRE colonization in children admitted to the PICU found a rate of 2.7%[15].
Research results on VRE colonization in developed countries have been highly variable. In New Zealand, Briggs et al. found a colonization rate of 0.3%[20]. In the United Kingdom, Gray et al. found that gastrointestinal VRE colonization was 38.3% in hematology/oncology patients, decreasing to 11% in patients admitted to hepatology/gastroenterology units, and to only 2.3% in children in the PICU[21]. In Korea, Yoon et al. found a VRE colonization rate of 30.3%[5].
The overall frequency of VRE colonization can be considered high if the results obtained in a systematic meta-analysis review by Flokas et al.[22] are taken into account. The review included 19 studies covering a total of 20,234 children hospitalized in general ICUs and PICUs where VRE colonization was 5% overall (3% to 8% in general ICUs and 2% to 9% in PICUs).
Variations in prevalence could be attributed to several different factors, including type of hospital, patient characteristics, and sample collection techniques, as well as the effective use of recommended measures to control bacteria transmission[12].
Based on the results of this study, one factor associated with VRE colonization is prior hospitalization in the past year. According to the results of the study by Reale et al. in Argentina, another factor associated with VRE colonization is prolonged hospitalization (p = 0.0001)[7].
In Korea, Kim et al. found that hospitalization and its duration (odds ratio: 7.24; 95% confidence interval: 3.22 to 16.26; p = < 0.001) were both risk factors for VRE colonization[16]. The results from other studies concur with the findings from this study. For example, in Peru, Elizaga et al. found that patients with a prior hospitalization had a 3.6 times greater risk of VRE colonization (odds ratio: 3.6; 95% confidence interval: 1.6 to 8.4; p = < 0.004)[10]. Previous hospitalization can increase the risk of VRE colonization because there is a greater possibility of receiving broad-spectrum antibiotics, especially when the admission is due to a high-risk condition. A previous hospital stay could also lead to exposure to microorganisms intrinsically resistant to vancomycin and, therefore, the acquisition of the enterococcus through contact with another carrier or through contaminated fomites[5],[6].
Patients who had used two or more broad-spectrum antibiotics also had a higher risk of VRE colonization. According to Reale et al.[7], in Argentina, the use of vancomycin increased the risk of colonization with the bacteria (odds ratio: 5.15; 95% confidence interval: 1.22 to 21.76; p = 0.02). Other studies concur with the findings of this study. For example, Singh et al.[1] found that the use of ceftazidime combined with vancomycin increased the risk of VRE colonization 1.7 times (p = 0.004) and the use of vancomycin or ceftazidime alone represented an even greater risk (odds ratio: 50.39; 95% confidence interval: 3.77 to 672; p = 0.003; and odds ratio: 95.62; 95% confidence interval: 7.41 to 999; p = 0.001, respectively). LIkewise, Henning et al. observed that vancomycin and ceftazidime were the antibiotics most associated with VRE colonization (p = 0.002 and p < 0.001, respectively)[13]. In Chicago (USA), Elizaga et al. found that the previous use of any antibiotic increased the risk of VRE colonization sevenfold (odds ratio: 7; 95% confidence interval: 2.7 to 18.4; p = < 0.001), which increased to 13.5 when vancomycin was used (odds ratio: 13.5; 95% confidence interval: 1.6 to 111; p = 0.005)[10]. In Peru, Flores-Paredes found that use of antibiotics led to a sixfold greater risk (odds ratio: 6; 95% confidence interval: 1.13 to 31.7; p = 0.03)[12].
In Turkey, Sutcu et al. found an association between VRE colonization and previous use of glucopeptides (odds ratio: 12.8; 95% confidence interval: 1.9 to 26.6; p = 0.012)[18], and Özkaya-Parlakay et al. found that antibiotic exposure in the previous three months was significantly related to VRE colonization time (p = 0.004)[23].
Finally, a systematic meta-analysis review carried out by Flokas et al. found that prior exposure to vancomycin and ceftazidime was a significant risk factor for VRE colonization in hospitalized children (odds ratio = 4.34; 95% confidence interval: 2.77 to 6.82; and odds ratio = 4.15; 95% confidence interval: 2.69 to 6.40, respectively)[22].
Use of two or more broad-spectrum antibiotics is related to VRE colonization because these drugs generate high antibiotic pressure by altering normal intestinal flora, leading to selective growth of VRE. Colonization can persist for weeks to even years[24].
This study had several limitations, including its retrospective nature (as it was based on medical records) and small sample size as well as the non-determination of the broad-spectrum antibiotic(s) that had the greatest association with VRE colonization (since the analysis was limited to two main groups of antibiotics categorized according to their spectrum of action).
Studies with prospective and multicenter designs that could help validate the findings reported here are required.
Conclusion
Patients admitted to the PICU with a history of prior hospitalization within the past year and exposure to two or more broad-spectrum antibiotics have a greater risk of VRE colonization.
Knowledge of the prevalence of VRE colonization and associated risk factors allows for monitoring for the correct and timely use of infection prevention measures such as contact isolation and hand hygiene by health personnel and members of the family that help with child care, which should be applied in the care of all patients. Continuing education, the adoption of policies for rational administration of antibiotics, and adequate surveillance of cases could help decrease the rates of VRE colonization so should also be emphasized.
Notes
Roles and authorship contributions
LD, AA: conceptualization, data management, formal analysis, research, methodology, project management, data presentation, manuscript preparation (development of the original draft), writing (revisions and editions).
MG: formal analysis, research, methodology, supervision, data presentation, manuscript preparation (development of the original draft), writing (revisions and editions).
IR, LD, HJJ: conceptualization, data management, formal analysis, research, methodology, project administration, supervision, data presentation, manuscript preparation (development of the original draft), writing (revisions and editions).
Competing interests
The authors have completed the ICMJE conflict of interest declaration form and declare that they have not received funding for the completion of this report; have no financial relationships with organizations that might have an interest in the published article, in the last three years; and have no other relationships or activities that could influence the published article. The forms can be requested from the lead author or the Journal editor.
Funding
The authors declare that there were no external sources of funding.
Ethics
This study was reviewed and approved by the ethics committee of the Faculty of Medical Sciences of the National University of Asunción (Paraguay), according to note UNA_FCM_DIN 279/2018, dated December 11, 2018.

