Research papers
← vista completaPublished on January 28, 2022 | http://doi.org/10.5867/medwave.2022.01.002510
Description of frequent and persistent symptoms of COVID-19 among older adults who attend senior centers
Descripción de síntomas frecuentes y persistentes de COVID-19 en asistentes a centros del adulto mayor
Abstract
Introduction COVID-19 not only acutely compromises people’s health but can also generate symptoms that remain weeks after the infection. Moreover, older adults may have different symptomatologic patterns than other age groups.
Objective To describe the acute and persistent symptoms of COVID-19 in older adult users of Social Security senior centers.
Methods A retrospective descriptive study was carried out by telephone call to older adults from five Peruvian senior centers, from July to September 2020, who reported being positive for COVID-19 in the last three months. Older adults were asked about associated symptoms, with a follow-up of up to four months.
Results The most frequent acute symptoms were cough, fever, headache, and myalgia. The mean num- ber of symptoms per person was one to three. We also found that 4.4% of COVID-19 cases had symptoms that persisted over three weeks
Conclusions Older persons in senior centers have a low frequency of persistent COVID-19 symptoms.
Introduction
By the end of April 2021 in Peru, the COVID-19 pandemic accumulated almost two million infections, of which approxi- mately 3.4% have died [1]. The older adults have been the most affected population, accounting for nearly 70% of COVID-19 deaths [2].
Although most recover entirely, those who experience severe COVID-19 disease and are hospitalized in the intensive care unit usually show sequelae symptoms due to disease complica- tions and iatrogenic harm [3]. These sequelae include hair loss, fatigue, anxiety, amenorrhea, insomnia, hyperexcitability, mem- ory impairment, and peripheral neuropathy. In this pandemic context, a family physician should identify and timely address these sequelae in primary care [4].
Some mild to moderate symptoms may appear for more than three weeks beyond acute infection, often referred to as pro- longed COVID syndrome, post-COVID symptoms, or post- acute COVID [5]. This condition appears to be present in almost 10% of SARS-CoV-2 infections within primary care [6].
Although there is still no consensus on terminology, when a patient experiences persistent symptoms for more than 12 weeks, such a condition is usually termed chronic COVID-19, or long COVID [7]. For the post-acute or chronic condition, the symptoms described by patients usually involve the respira- tory tract and the cardiovascular and nervous systems.
It has been described that older and frail adults may present symptom patterns that differ from younger people, which could be predictors of severity and subsequent complication [8]. Moreover, the negative impact on physical and mental health in older adults is greater than in the younger [6].
In Peru, approximately 30% of the population is enrolled in the Social Security subsystem (EsSalud). To date, 16% of the insured are older adults, which has increased over the years. Moreover, in this public health context, the older adults in Peru could reach 24% by 2050 [9]. For this reason, public health pol- icies should focus on improving the quality of life of older adults, considering their vulnerability to diseases such as COVID-19.
The structure of the Social Health Insurance allows older adults to access health and social benefits in health facilities and senior centers, respectively. The senior centers receive older adults only during the day, providing care and spaces related to physi- cal activity, art, music, cooking, mental health, and peer-to-peer living, among other services. At a national level, there are 126 senior centers whose users, in the context of the COVID-19 pandemic, have been monitored to prevent risks and disease. In this sense, the pandemic has generated the need to identify and track post-COVID-19 symptoms in older adults to provide timely healthcare. This study aims to describe the acute and prolonged symptoms of COVID-19 in older-adult users of the Social Health Insurance senior centers.
Methods
An observational, descriptive, retrospective study was conducted.
The population consisted of users of the Social Security Health Insurance (EsSalud) senior centers from all over Peru who reported a positive test for COVID-19 during July and September 2020. Patients were also asked about the date and type of test performed. Reviewing the literature, we identified 22 COVID symptoms [10]. Between October and November 2020, the older people were followed up by telephone by three interviewers. These were previously trained to identify COVID-19 symptoms that persisted beyond the acute period.
The older adults were asked about each symptom’s onset and end date. If any COVID symptoms were still present at the monitoring time, weekly follow-up was performed until the symptom(s) disappeared. Post-acute and chronic COVID-19 were defined as symptoms that persisted for more than 3 and 12 weeks from symptom onset, respectively [6].
A descriptive statistical analysis was performed to determine the frequencies and averages of symptoms. The numerical data were expressed as mean and standard deviation, taking into account the normal distribution of the data. Additionally, a generalized linear model (GLM) with Poisson family and Log function was developed to obtain Prevalence Ratios (PR) looking for an association between the variables of interest. Astatistically significant difference was considered when p <0.05. Statistical analysis was performed with the STATA 17.0statistical package (StataCorp, TX, US).
The present study was reviewed and approved by the ResearchEthics Committee for COVID-19from the Social HealthInsurance. The older adults participated voluntarily and anonymouslyafter obtaining their informed consent. The coded databasewas analyzed exclusively by the investigators.
Results
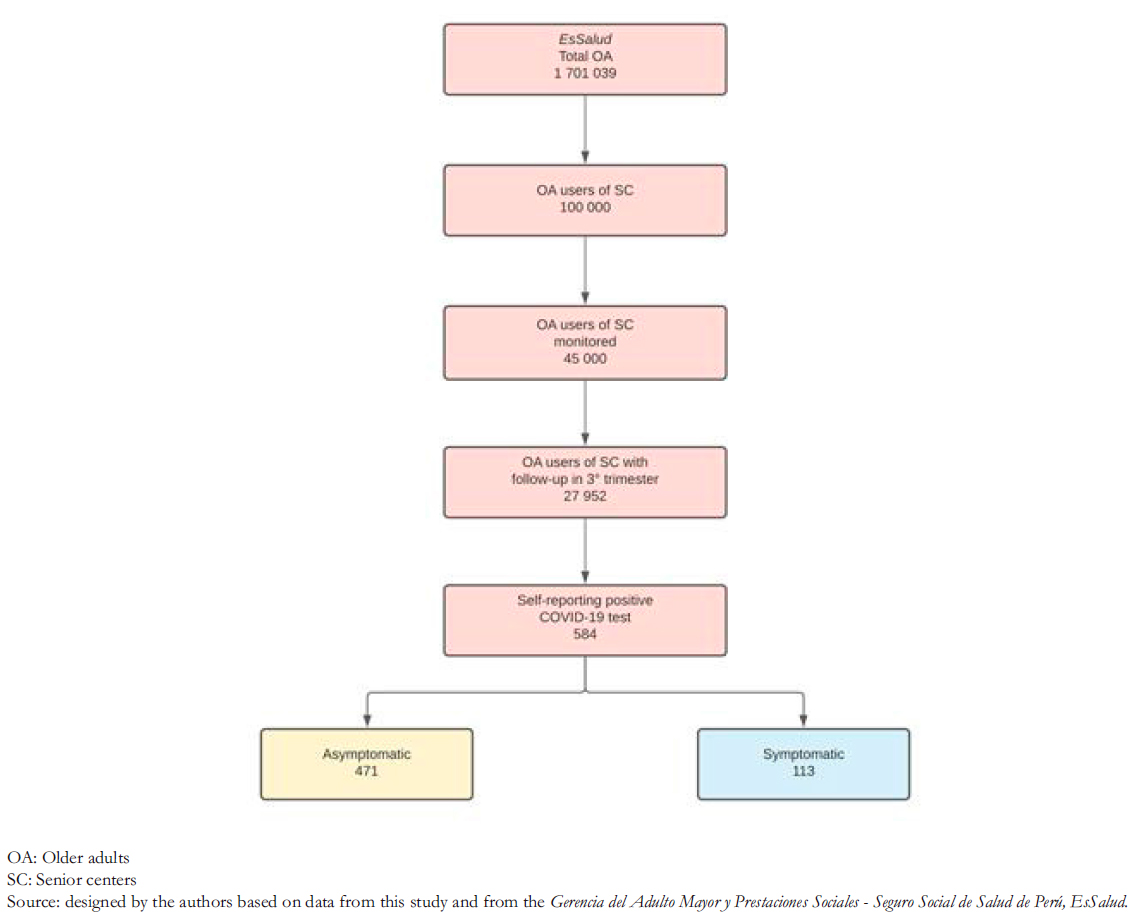
The Social Security Health Insurance (EsSalud) monitored 27 952 users of senior centers between July and September 2020.
Of these, 584 older adults reported having a positive test for COVID-19, with a cumulative incidence rate of 209 per 10 000, of which 113 (20%) were symptomatic (Figure 1).
The average age of the symptomatic older adults assessed by telephone was 71.3 ± 7.2 years, most were female, and only five had post-acute or chronic COVID-19 (Table 1).
Among the senior center users, the most frequent symptoms were cough (20%), fever (11%), headache (10%), and myalgia (19%). The symptoms with the longest duration were vértigo (98 days), myalgia (48 days), rhinitis (21 days), and fatigue (15 days) (Table 2).
Of the 19 symptoms reported by older adults, three remained for more than 21 days in five older adults. Cough was present for five and seven weeks, myalgia for seven weeks, and vertigo for 14 weeks (two cases). Moreover, 95.6% of symptomatic cases were defined as an acute infection, 2.7% as post- COVID-19, and 1.7% as chronic COVID-19.
Assuming asymptomatic patients as a control group, a bivariate regression with a generalized linear model between age and being symptomatic showed no significant association (PR: 0.99; 95% confidence interval: 0.97 to 1.02), nor between sex and being symptomatic (PR: 0.98; 95% confidence interval: 0.66 to 1.47). There was no significant association between age, sex, and having persistent COVID-19 symptoms.
 Full size
Full size 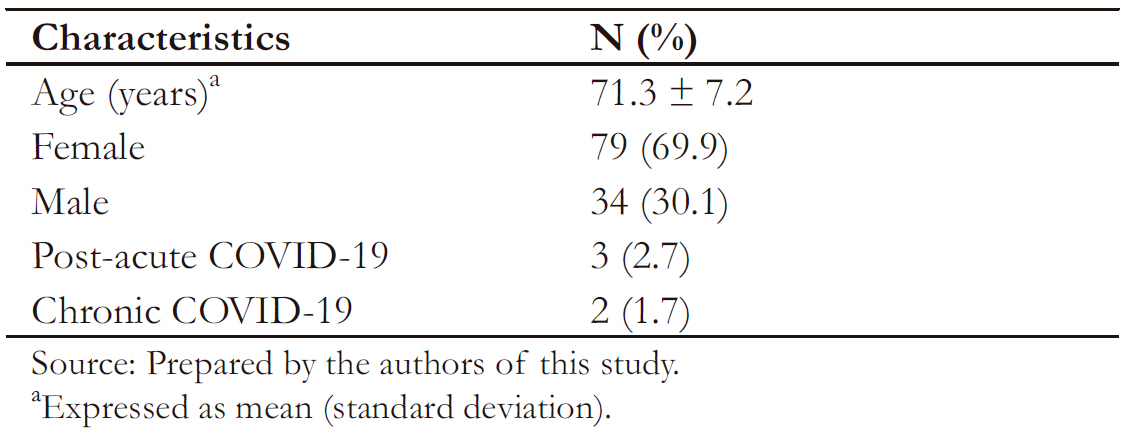 Full size
Full size 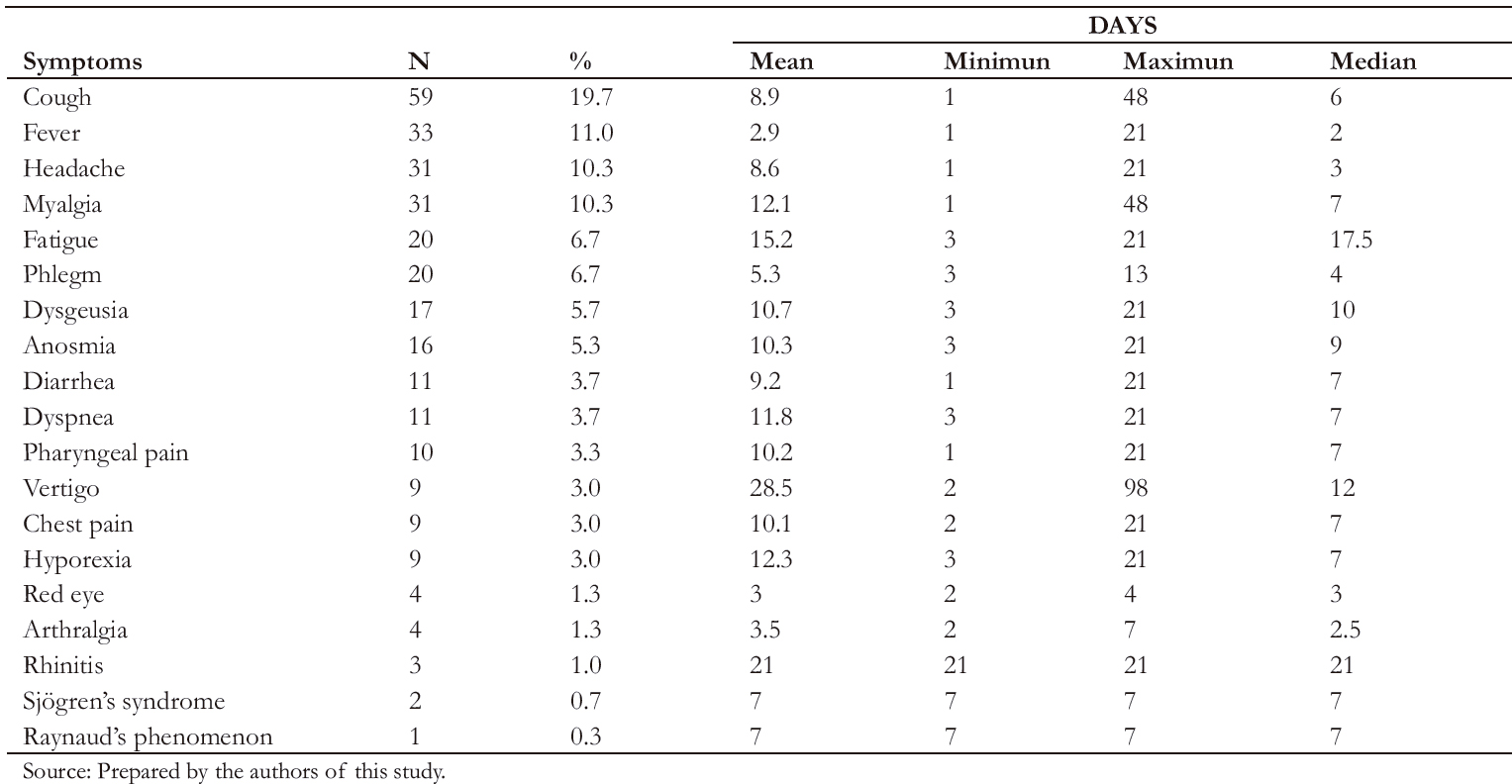 Full size
Full size 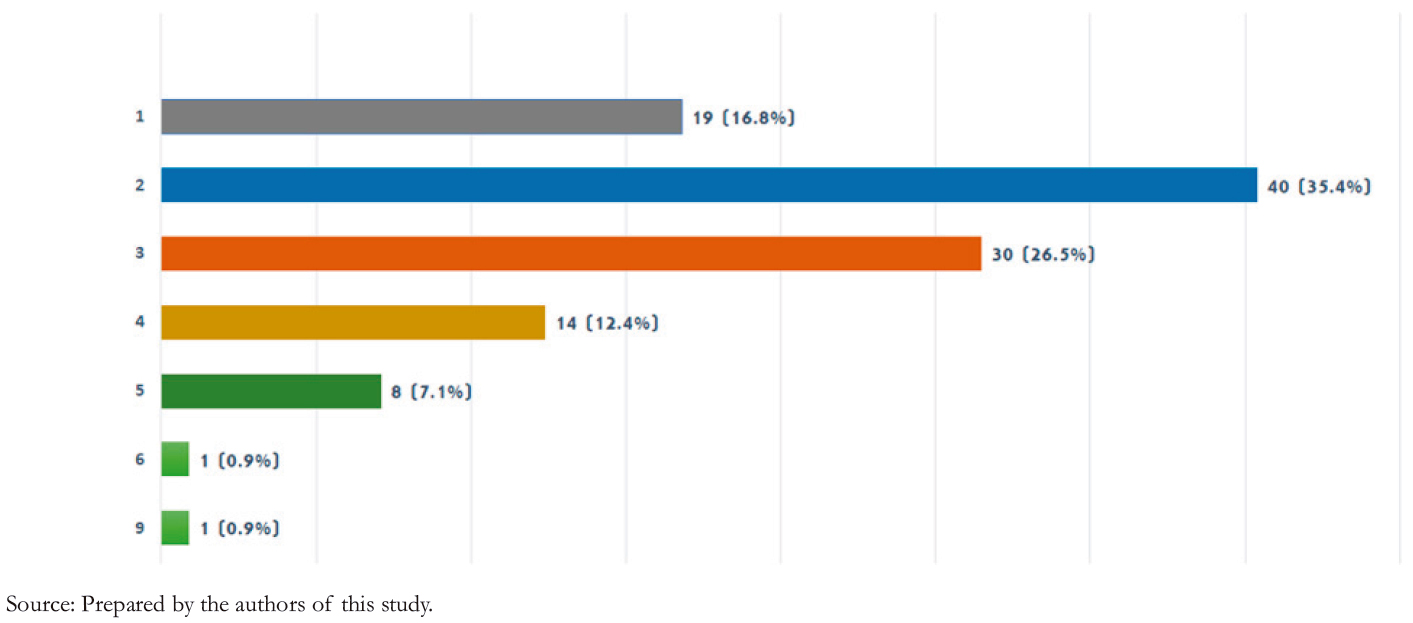 Full size
Full size Discussion
Social activities for older adults in the Social Health Insurance senior centers positively influence mental health, cognition, participation, reduction of physical symptoms, and social con- struction, among others [11],[12],[13]. In the context of the COVID-19 pandemic, these activities were conducted virtually through information and communication technologies. As older adults are a vulnerable population, the present study con- stitutes an effort of socio-health articulation that allows for comprehensive care, together with a substantial commitment to recognize problems and propose timely interventions among older adults.
Our study found that of the 113 symptomatic older adult users of the senior centers, 95.6% had acute symptoms. Only 4.4% had post-acute or chronic COVID-19 symptoms (i.e., for more than three weeks), which is lower than a study by Greenhalg et al. where they found 10% of post-COIVD symptoms in primary care [6]. Other studies have found that up to 27% of patients persist with some symptoms at the fourth month of follow-up. However, many of these studies included older adults post-hospitalization and post-intensive care unit admission, which could explain the higher sequelae symptoms [14].
We also found that the incidence of COVID-19 was lower than described by the Social Health Insurance for older adults (2% versus 7.3%, respectively). In addition, 80% of asymptomatic cases were identified in a population usually worsts affected by COVID-19. This number is much higher than Bliddal et al., which found 34% asymptomatic in non-hospitalized patients [15]. We believe asymptomatic or mild symptomatic cases could be underestimated due to recall bias, and some symptoms may not be associated with COVID-19. On the other hand, the fact that this is a self-care population that belongs to a senior center, a program that strengthens self-care competencies, could par- tially explain the low incidence of COVID-19 and the reduced persistence of symptoms.
Although self-reporting of diagnosis has a recall bias, it is a method used during the pandemic without access to individual laboratory evaluation results [14]. Our study attempted to address this bias by querying the date and type of examination performed.
Our study took the Italian study by Carfi et al. as a basis for symptoms, identifying 19 out of 22. In this Italian study con- ducted in patients after hospital discharge, 22 persistent symp- toms were identified at the acute phase of COVID-19, at an average follow-up of two months. This study found that half of them had at least three persistent symptoms, identifying fatigue, dyspnea, arthralgia, and chest pain as the most per- sistent [10].
Although persistent symptoms were few, they ranged from 22 to 98 days. In a descriptive study (n = 4812), symptoms lasted more than 28 days in 13.3%, more than eight weeks in 4.5%, and more than 12 weeks in 2.3% of patients, which resembles our study. Most studies have evaluated persistent symptoms after hospital discharge with an average follow-up of three months [16],[17],[18],[19]. Some have evaluated it for six months [18],[20], and ours did for two months.
The most frequent symptoms vary according to each investiga- tion. However, fatigue, dyspnea, anosmia, cough, ageusia, and headache are usually present [21],[22],[23], and most studies are in line with ours that cough and headache as frequent. A similar study identified dyspnea, cough, and fatigue as the most fre- quent symptoms of post-acute COVID-19 [24], and another publication described that symptoms could remain for three months [25].
Our study did not evaluate the presence of comorbidities. However, it is necessary to consider multimorbidity as a factor associated with persistent symptoms since arterial hypertension and diabetes mellitus have already been associated with post- COVID [26],[27]. Not identifying comorbidities in our study lim- its findings on a relationship between COVID-19 infection and post-COVID symptoms, either by the infection or by adverse effects of drugs used to treat these chronic conditions.
Conclusions
This study found that older adults in senior centers have a low frequency of post-COVID-19 symptoms. From the analysis performed, it is clear that there are still many questions about persistent COVID-19 symptoms, including their definitions, consequences, and who is at risk of manifesting them [28].
We consider it essential to expand our knowledge on post-acute and chronic COVID-19 in the Peruvian population, especially older adults. This information could allow the development of guidelines and protocols to reduce the disabling effect that this condition could generate.
Notes
Contributor roles
PJC: participated in the writing, statistical analysis, final approval and is responsible for all aspects of the work. ZRA: participated in the drafting, writing, final approval and is responsible for all aspects of the work. MSCF: participated in the conception, drafting, final approval and is responsible for all aspects of the work.
Acknowledgments
We want to thank the staff of the Gerencia del Adulto Mayor y Prestaciones Sociales for their willingness to collaborate with our study.
Competing interest
The authors completed the ICMJE conflict of interest statement and declared that they did not receive funds for this article; they have no financial relationships with organizations that may have an interest in an article published in the last three years, and they have no other relationships or activities that may influence the publication of the article. Forms can be requested by contacting the responsible author or the Editorial Board of the Journal.
Ethics
The Specific Research Committee for COVID-19 approved the present study with document S/N which is available upon request addressed to the corresponding author.
Language of submission
Spanish.

