Research papers
← vista completaPublished on April 7, 2022 | http://doi.org/10.5867/medwave.2022.03.002553
Seroprevalence and estimation of the impact of SARS-CoV-2 infection in older adults residing in Long-term Care Facilities in Chile
Seroprevalencia y estimación del impacto de la infección por SARS-CoV-2 en personas mayores residentes en centros de larga estadía en Chile
Abstract
Introduction Older adults are at a higher risk of severe illness and death from COVID-19. This vulnerability increases in those who live in long-term care facilities due to overcrowding, greater physical dependence, and contact with health workers. Evidence on the impact of the pandemic on these establishments in lowand middle-income countries has been scant. This study aims to determine the seroprevalence of SARS-CoV-2 in older people residing in long-term care facilities and estimate the impact of infection after the first wave of the pandemic.
Methods A cross-sectional design with 2099 residents in three regions of Chile was carried out between September and November 2020. Measurement of antibodies was performed with a rapid test. The impact of SARS-CoV-2 infection was estimated with seropositive residents, those who had a history of positive polymerase chain reaction tests, and those who died from COVID-19. Bivariate analysis with the region, sex, age, history of COVID-19, physical dependence, and serological results were performed. In addition, we performed a correlation analysis between the seroprevalence of the centers by the municipality and the rate of confirmed cases.
Results The seroprevalence of SARS-CoV-2 antibodies in the three regions was 14.7% (95% confidence interval: 13.2 to 16.3%), the infection impact was 46.4%, and the fatality rate was 19.6%. A significant correlation was found between the seroprevalence of older adults residing in long-term care facilities and the cumulative incidence by municipalities.
Conclusions The seroprevalence of older adults residing in long-term care facilities was higher than the general population. The high impact of infection among this population at the end of the first wave of the COVID-19 pandemic is similar to other countries. The centers' environment is directly related to COVID-19 infection. Morbidity and mortality monitoring systems should be implemented promptly to establish prevention and control measures.
|
Main messages
|
Introduction
Coronavirus disease 2019 (COVID-19) is an acute respiratory disease that affects the entire population. However, the disease is aggravated in older adults, increasing the fatality rate. Immunosenescence (the loss of adaptive immune functions) and the usual chronic comorbidities expose older adults to a greater risk of severe disease [1],[2],[3],[4].
Older adults have a greater frequency of atypical manifestations, such as malaise, normal temperature, agitation or confusion, anorexia, or gastrointestinal symptoms. Likewise, dementia patients have a higher risk of cognitive alterations with COVID-19. These characteristics hinder early screening and timely management in this population [5],[6].
Globally, the fatality rate under 70 years of age is between 0.3% and 3.5%, while over 80 years, it falls between 15% and 22.7% [4]. Given the age-related vulnerability, long-term care facilities (LTCFs) for older adults were the focus of major concern during the pandemic [7]. In October 2020, a report including 21 countries indicated that 46% of COVID-19 deaths were in people residing in these centers. Countries such as Belgium, Ireland, Spain, the United Kingdom, and the United States reported one death for every 25 residents in LTCF [8], while the information in Latin America is scarce.
Severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) infection can spread rapidly within these centers due to the characteristics of residents and staff. One study identified that LTCFs have up to four times the seroprevalence of SARSCoV-2 antibodies compared to the general population (odds ratio: 4.53; 95% confidence interval: 3.19 to 6.45) [9]. Key factors include a high staff turnover, increasing the risk of introducing the virus, and close contact between residents and caregivers due to the dependence and frailty of older adults. Furthermore, overcrowding, precarious sanitary conditions of the facilities, and a high prevalence of concomitant illnesses, among others, facilitate virus transmission [3],[10].
Despite its relevance, there is a lack of robust evidence on COVID-19 monitoring and prevention measures in LTCFs, which could have helped timely detection and mitigation of virus transmission and impact on these centers [11],[12].
Symptomatology-based detection should not be the only way to determine COVID-19 infection in this specific group [13],[14] since 30% to 43% of polymerase chain reaction (PCR) positive patients are asymptomatic. Therefore, timely detection is crucial in improving measures to deal with the outbreak [11],[15]. Another essential consideration is the level of community transmission where the LTCF is located. It has been pointed out that communities with a higher rate of COVID-19 infections are associated with a higher number of cases and deaths in these centers than in communities with lower infection rates [16].
Seroprevalence studies can accurately estimate virus spread within LTCFs and may aid strategic aspects regarding outbreak control by detecting asymptomatic cases and assessing factors associated with virus transmission [17],[18].
As of August 2021, epidemiological studies in Chile showed that individuals over 60 years accounted for 6% of all COVID-19 cases and 82% of the total accumulated deaths (38 989/47 504), resulting in a case-fatality rate of 14% among infected patients [19],[20].
Most LTCFs in Chile are non-profit public residences or support centers, depending on the National Service for the Elderly (SENAMA). They are intended for older people who require a protected environment and specific care to maintain their health and functionality for biological, psychological, or social reasons. The resident population is 60 years or older and has a high vulnerability, few family networks, and a high prevalence of cognitive impairment [21].
On April 2 2020, health safety measures for these centers mainly focused on intensifying COVID-19 prevention measures (physical distancing, hand washing, use of masks, and improving ventilation), preventing residents from leaving the center or going to shared spaces, and prohibiting visitors [22].
Studies in developed countries have shown the great impact of the pandemic on institutionalized older adults. However, there is no detailed information in Chile on the number of infections and the impact of COVID-19 on LTCFs. Therefore, this study aimed to determine the seroprevalence of SARS-CoV-2 infection among older adults residing in LTCFs in three regions of the central area of Chile between September and November 2020 and estimate the impact of infection after the first wave of the pandemic.
Methods
Study design, setting and participants
We conducted an observational cross-sectional study on a population of 5577 older adults residing in 105 public LTCFs in the three central regions of Chile: Valparaíso (23 centers, 985 older adults), Metropolitan (64 centers, 3899 older adults), and O'Higgins (18 centers, 693 older adults). The study was designed as a census for all LTCRs and its residents within the three regions. Participation could be authorized by the resident, by a responsible family member if the resident presented cognitive impairment, or by the director of the LTCF. The sampling method corresponded to non-probabilistic convenience sampling. However, a minimum sample of 896 subjects with 95% confidence, 3% error, and maximum variability of 50% was considered to ensure compliance with the proposed objectives.
Variables and data collection Instruments
The measurement of antibodies against SARS-CoV-2 was performed with the 2019-n-CoV Ab test (Colloidal Gold) from the manufacturer Innovita (Tangshan) Biological Technology Co Ltd. of China. It is a rapid test that uses a capillary blood sample obtained by puncturing the skin, which delivers results in 10 minutes. The sensitivity reported by the manufacturer is 87.3% (95% confidence interval: 80.4 to 92%), with a specificity of 100% (94.2 to 100%) [23]. The researchers verified these indicators by analyzing 27 samples of confirmed (hospitalized) cases of COVID-19 by RT-PCR, with more than 14 days of symptoms and 30 negative samples of pre-pandemic serums. The result showed 90.3% sensitivity and 100% specificity of the test.
The test result was measured a maximum of 15 minutes after the puncture. The appearance of a band in IgM or IgG was considered positive, negative was considered in the absence of bands, and inconclusive when the reading was not possible. In addition, the rapid test cassette was photographed, which allowed the research team to carry out a second reading in 77.8% of the tests (1633). A Kappa concordance analysis was performed to evaluate differences between both observations, which showed an agreement of 93.4%, higher than expected by chance of 75.1%, with a K-index = 0.7342, statistically significant (p-value < 0.001), and with good concordance (scale between 0.61 and 0.80).
A datasheet was also completed for each participant that included: LTCF, municipality and region, age, sex, history of COVID-19 with RT-PCR confirmation and having any degree of physical dependence. This information was collected through an App designed for the study through mobile phones.
The fieldwork was carried out between September and November 2020 by previously trained LTCF delegates related to the health area.
We also estimated the impact of the infection, i.e., the total population affected by COVID-19, including infections, diseases, and deaths. For this estimate, we used information from the National Service for the Elderly (SENAMA) that reported COVID-19 deaths between March and November 2020 for each center participating in the study. This information also allowed estimating indicators of lethality and mortality.
The cumulative incidence rate of confirmed cases of COVID-19 by municipalities was obtained from the Ministry of Health data as of November 12, 2020 [24]. These were correlated with the LTFC seropositive rate by municipalities.
Analysis
The seroprevalence was obtained from the proportion of older adults with positive results for antibodies against SARSCoV-2 from the total number of study participants, calculating the 95% confidence interval using the exact binomial method. The results were adjusted according to the sensitivity and specificity of the diagnostic test and compared with the crude seroprevalence, based on the Rogan and Gladen methodology with 95% confidence interval by the Blaker method [25].
Bivariate analyses of SARS-CoV-2 seroprevalence were performed according to region, sex, age, history of COVID-19, and physical dependence. Results were expressed as odds ratio and 95% confidence intervals.
A scenario of total residents affected by COVID-19 was constructed, given the number of deaths before the study and the possible drop in the level of antibodies after the infection, adding those who died from COVID-19 and people with a previous positive RT-PCR history but who obtained negative results in the rapid antibody test. With this scenario, we estimated the total number of people affected by COVID-19 by adding the subjects with positive IgG/IgM, people with negative IgG/IgM but a history of positive RT-PCR, and deaths from COVID-19. Thus, the prevalence of people affected by COVID-19 and the fatality and mortality from COVID-19 in LTCF residents was estimated.
Finally, at the LTCF level, the proportion of centers that presented at least one resident with antibodies against SARSCoV-2 was calculated.
The correlation between the seroprevalence of SARS-CoV-2 antibodies in LTCF by municipality (per 100 residents) and the cumulative rate of confirmed cases of COVID-19 by municipality (per 100 000 population) were analyzed using the Spearman test (rho) since the variables did not have a normal distribution (verified through the Shapiro-Wilk test).
 Full size
Full size Ethics
The Scientific Ethics Committee of the Universidad del Desarrollo approved the study. Participation was voluntary. The older adults signed informed consent in written form when they had the cognitive ability to do so. Otherwise, authorization was requested from a family member responsible for the resident or the technical director when they did not have a guardian or family member. The confidentiality of the information was safeguarded, and the data were analyzed in an anonymous and aggregated manner.
Results
Participant characteristics
Of the 105 public and non-profit SENAMA facilities in the included regions, 66.7% (70 centers) agreed to participate. A total of 2099 older adults were recruited and tested for antibodies from a universe of 3048 residents (68.9%). The participation rate varied from 60.9% in the Metropolitan Region (37 centers, 1183/1943 residents) to 78% in the Valparaíso Region (16 centers, 414/531 residents) and 87.4% in the O'Higgins Region (17 centers, 502/574 residents).
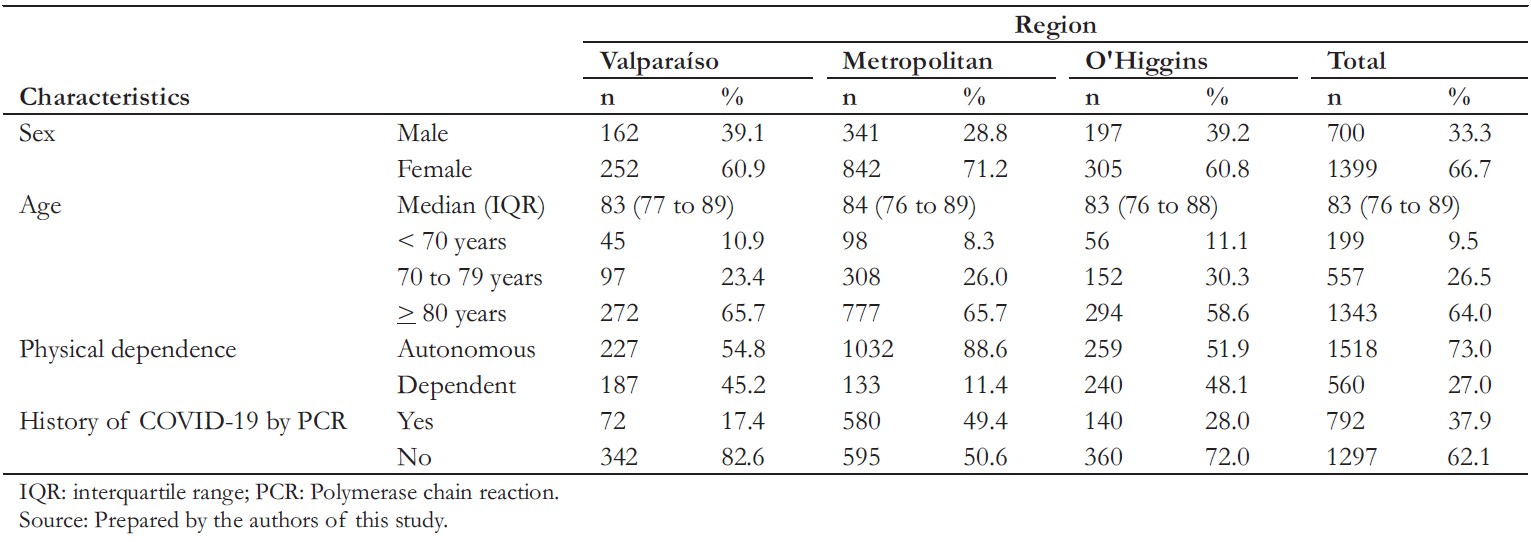
We found that 66.7% of participants were female, with a median age of 83 years (interquartile range: 76 to 89) with a maximum and minimum age of 104 and 39 years. Moreover, 73% of subjects were autonomous, and 37.9% had a history of COVID-19 by RT-PCR (Table 1).
Seroprevalence of antibodies against SARS-CoV-2
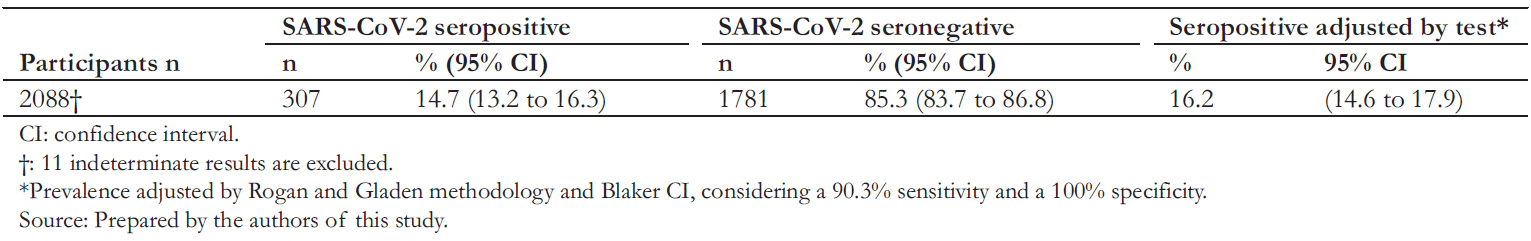
The 61.4% (43 centers) of LTCFs studied had a resident with a positive result for antibodies against SARS-CoV-2. Seroprevalence reached 14.7% (95% confidence interval: 13.2
to 16.3). This number increased to 16.2% (14.6 to 17.9%) when corrected according to the performance of the test (Table 2).
Significant differences were observed in seroprevalence according to sex, region of the LTCF, but not by age subgroups. The highest seroprevalence was observed in the Metropolitan Region and the lowest in Valparaíso, with a statistically significant difference between regions (odds ratio: 1.7; 95% confidence interval: 1.2 to 2.4). Men were almost twice more likely to have antibodies against SARS-CoV-2 than women (1.9; 1.5 to 2.4) (Table 3).
The history of COVID-19 diagnosis appears strongly associated with seropositive residents (odds ratio: 5.0; 95% confidence interval: 3.9 to 6.5) (Table 3). Of the total number of seropositive residents (306), 29.4% did not have a history of COVID-19 (90 residents).
 Full size
Full size 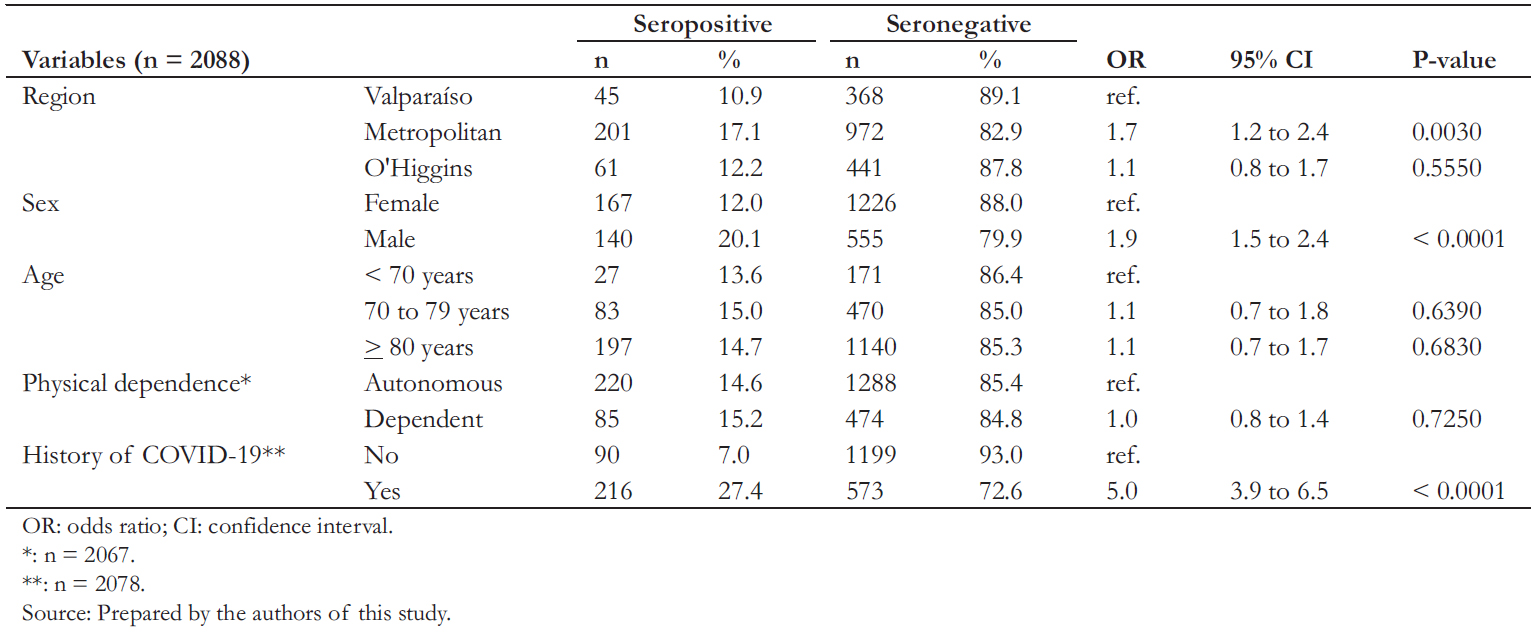 Full size
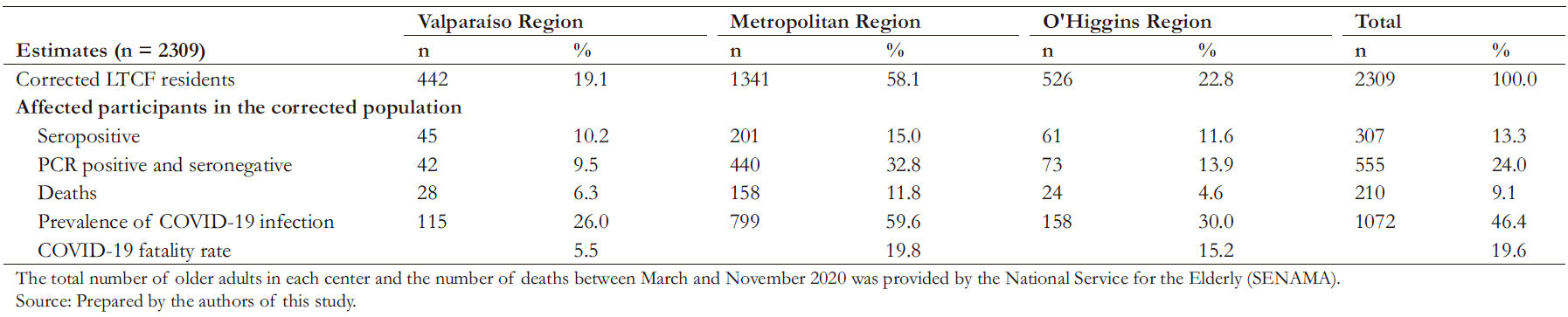
Full size Estimation of the impact of infection: deaths, fatality Rate, and infection prevalence
Table 4 shows the estimate of deaths from COVID-19 for the study population, which corresponded to 9.1%, with a fatality rate of 19.6%. Both mortality and fatality were higher in the Metropolitan Region. Considering the estimate of death, plus those who presented antibodies against SARS-CoV-2 and those seronegative but had a history of COVID-19 by PCR, we found a total COVID-19 infection prevalence of 46.4% (1072 residents).
Correlation between seroprevalence of SARS-COV-2 antibodies In LTCF residents and municipality cumulative incidence rate
The seroprevalence of LTFC residents by municipalities was positively and significantly correlated with the frequency of the disease (rate of confirmed cases) at the municipality (rho = 0.4229; p-value = 0.0042). In contrast, there was no correlation between seroprevalence and the number of residents per center (p-value = 0.3374). Despite the dispersion of the data, Figure 1 shows a linear relationship between the seroprevalence and the municipality cumulative incidence rate.
Discussion
After the first COVID-19 wave, we found a seroprevalence of 14.7% in LTCF residents, higher than the seroprevalence identified in the general population in a similar period (10.4%) [26]. When considering older adults with positive RT-PCR, those who were seropositive, and deaths from COVID-19, the estimated total impact increases to 46.4%. In other words, just under half of LTCF residents at the beginning of 2020 had been infected with COVID-19.
The highest seroprevalence (17%) was identified in the Metropolitan Region, matching with the highest epidemic activity compared to other regions – characterized by a high incidence rate, mortality, fatality, and excess deaths [27]. This observation is consistent with the correlation obtained between the LTCF seroprevalence and the incidence of COVID-19 in the respective municipality. The seroprevalence of our study is similar to studies conducted on health workers of institutions within conditions of greater vulnerability and susceptibility to COVID-19. Additionally, it has been reported that these workers act as a bridge population. This personnel rotates between care centers and residences for older adults, favoring viral transmission between these facilities [3],[10]. This situation replicates in the centers assessed in this study.
Published studies of seroprevalence in LTCFs for older adults have high variability in their findings. A study in London showed seropositivity rates between 10.7% to 56.5% in centers without previous outbreaks and between 41.9% to 84% in those with two or more outbreaks [28], which is higher than reported in this study. A systematic review also reported a seroprevalence of 59.2% (interquartile range: 39.7 to 78.8%) where healthcare institutions and LTCFs were studied [29]. In contrast to the above (and in line with this study), there was a seroprevalence of 11.5% (95% confidence interval: 7.5 to 16.6%) reported in Brazil – where immunochromatography was used at four to five months from the first COVID-19 case in the country [30]. These findings illustrate the difficulty of establishing comparisons between countries, given that the characteristics of older adults in LTCFs can vary. Also, a higher impact of COVID-19 has been suggested in nursing homes than in LTCFs [31].
 Full size
Full size 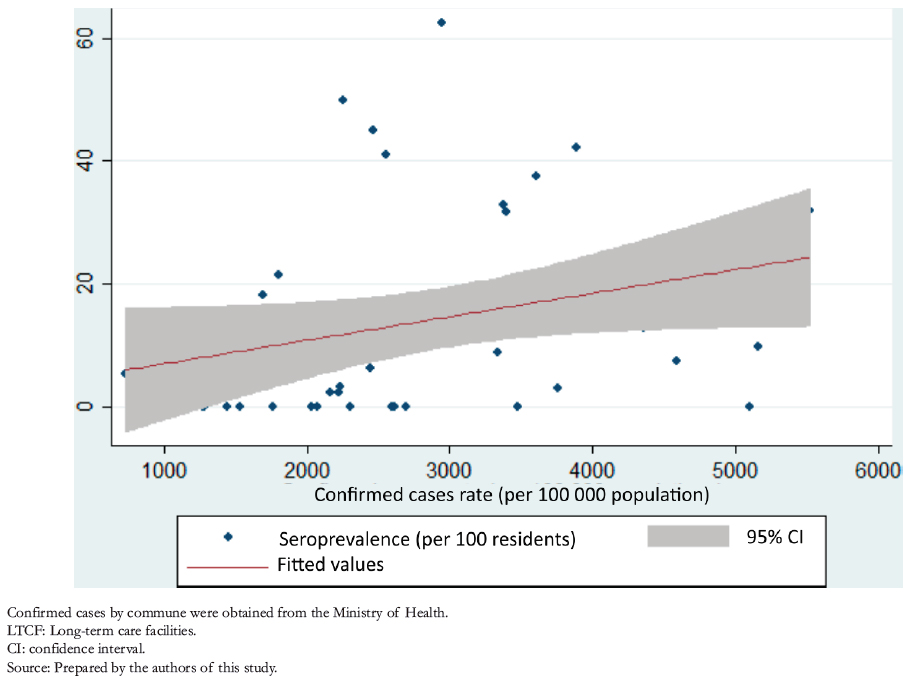 Full size
Full size We found that the seroprevalence was positively correlated with the municipality cumulative incidence rate, indicating that the infection within the LTCFs is related to the transmission in the environment where they are located, in line with other studies [16],[32]. This finding suggests that the control measures in these centers – particularly in timely screening, the isolation of positive cases, and the isolation of resident and worker contacts – should be improved [2]. It has been reported that LTCF workers who lived in high-incidence communities were an important risk factor for infection [10]. Regarding prevention measures, Chile (like many countries) implemented the recommendations of the World Health Organization [33] and restricted visits to these centers [22]. However, this strategy may have been late in the onset of the outbreak, explaining the high incidence and mortality seen in LTCFs [34].
On the other hand, unfavorable structural conditions have been described in non-profit LTCFs and with a higher number of beds per room [35]. Lack of space restricts the adequate distancing between residents and workers, an important barrier for viral transmission [3],[10].
This study found 29.4% of seropositive cases without a history of positive RT-PCR for COVID-19, similar to other studies in the general population [36]. In a study in the general population of Chile, this percentage corresponded to 36% [26],[37], a difference explained by higher monitoring, which allowed better detection of SARS-CoV-2. The low seroprevalence in people who had a history of COVID-19 by RT-PCR (27.4%) can be explained by asymptomatic cases that did not seroconvert due to lower antibody production [2],[38]. Given the contingency of the pandemic, we could not corroborate the history of symptoms. The low number of seropositivity in those who had a previous history of positive RT-PCR can also be explained by the timing of the study. The Metropolitan Region had the lowest seropositivity in those with a history of COVID-19 (23.8%) and presented its peak of cases a month before Valparaiso and O'Higgins Regions (41.7% and 34. 3%). Studies report a loss of antibodies between three and six months after disease onset [2],[39],[40]. Moreover, it could also be explained by immunosenescence, which may be aggravated due to the fragility of older adults in LTCFs [41]. From another perspective, the test’s sensitivity may explain the low seroprevalence found [42]. The ELISA technique has been indicated as the best option for serological studies [2].
Although the participation rate was 69%, a limitation that should be considered is the convenience sampling due to the entry restrictions of some centers and the refusal of some LTCF residents to participate. Despite the above, the initially estimated sample size was surpassed, including 2099 older adults. It should also be noted that the three regions studied concentrate over 70% of facilities in the country. Another limitation inherent to seroprevalence studies is survivor bias. Countries have reported high mortality in LTCFs in the first pandemic wave [8],[43]. The fatality estimated in this study is 8.5 times higher than the current fatality rate of the Chilean population (2.3%) [24] and 1.45 times higher in cases over 60 years old (13.8%) [19]. A similar fatality rate was reported in the United States, with 18.4% in those over 65 years [44], while a Brazilian study reported a 25% fatality rate [30]. However, fatality varies between countries due to the quality of monitoring, cause of death definitions, and population age structure [45]. At the analysis level, we should note the limitation of some estimates used as denominators, mainly in deceased and residents of the centers during the study.
Despite these limitations, this is the first study in Chile on older adults residing in LTCFs and represents an essential contribution to decision-making aimed at this highly vulnerable group. Another strength is the high number of participants and the analysis of the disease impact in the centers of three cities in Chile. In addition, this study’s collaborative work and institutional partnerships should be highlighted. In all, this study may transfer knowledge to decision-making and nurture new research focused on generating information promptly and for outbreak control, all of which is relevant considering that transmission continued within these centers despite the active monitoring of SARS-CoV-2.
Conclusion
We found a higher seroprevalence among older adults residing in LTCFs than the general population and a high seroprevalence among residents without a history of COVID-19 diagnosis.
A high impact of COVID-19 was estimated by including information on the history of positive RT-PCR and deaths. Given that the LTCF environment is directly related to the infection presented within it, timely prevention and control measures are required against an epidemic.
Due to the fragile characteristics of this population, the implementation of timely and continuous morbidity and mortality monitoring systems are required, which consider new risk situations in the short, medium, and long term – even among the vaccinated population.
Notes
Contributor roles
PR, MH, IM y JB: conceptualization, methodology, software, validation, formal analysis, research, resources, data curation, writing-draft, writing-review and editing, visualization, supervision, project administration. CL and GR: conceptualization, methodology, software, validation, research, data curation, writing-draft, writing-review and editing, visualization, project administration. XA and PV: conceptualization, methodology, formal analysis, research, data curation, writing-draft, writing-review and editing, visualization. CA and TG: conceptualization, methodology, validation, research, resources, writing-draft, writing-review and editing, visualization, supervision, project administration.
Acknowledgments
We thank SENAMA, particularly the LTCF delegates, who collaborated with the fieldwork and the directors of the institutions that agreed to participate in this collaborative study: Fundación Chile, Ministry of Science and Innovation, Universidad Adolfo Ibáñez, and Universidad del Desarrollo. We would also like to thank the participants in this study.
Competing interests
The authors declare no conflict of interest.
Funding
This project received no funding.
Ethics
The Scientific Ethics Committee of the Universidad del Desarrollo approved the study, file number 2020-97.
Language of submission
English. No Spanish version is available.

