Health economics
← vista completaPublished on September 2, 2024 | http://doi.org/10.5867/medwave.2024.08.2918
Electrophysiology lab efficiency using cryoballoon for pulmonary vein isolation in Latin America: A sub-analysis of the Cryo Global Registry Study
Eficiencia del laboratorio de electrofisiología que utiliza criobalón para el aislamiento de venas pulmonares en Latinoamérica: Un subanálisis del Cryo Global Registry Study
Abstract
Objective Cryoballoon ablation for pulmonary vein isolation is a time-efficient procedure that can alleviate stress on electrophysiology lab resources. This analysis modeled the impact of cryoballoon ablation on electrophysiology lab operation using data from Latin America.
Methods Data from centers in Argentina, Mexico, Colombia, and Chile of the Cryo Global Registry were used as inputs for an electrophysiology lab efficiency simulation model. The model used the assumption that either two (today’s electrophysiology lab operations) or three (including electrophysiology lab operational changes) cryoballoon ablation procedures could be performed per day. The endpoints were the percentage of days that resulted in 1) overtime and 2) time left for an extra non-ablation electrophysiology procedure.
Results Data from a total of 232 procedures from six Latin American centers were included in the analysis. The average electrophysiology lab occupancy time for all procedures in Latin America was 132 ± 62 minutes. In the Current Scenario (two procedures per day), 7.4% of simulated days resulted in overtime, and 81.4% had enough time for an extra electrophysiology procedure. In the Enhanced Productivity Scenario (three procedures per day), 16.4% of days used overtime, while 67.4% allowed time for an extra non-ablation electrophysiology procedure.
Conclusions Using real-world, Latin American-specific data, we found that with operational changes, three ablation procedures could feasibly be performed daily, leaving time for an extra electrophysiology procedure on more than half of days. Thus, use of cryoballoon ablation is an effective tool to enhance electrophysiology lab efficiency in resource-constrained regions such as Latin America.
Main messages
- This manuscript explores the potential for operational optimization through a discrete event simulation approach in the field of cardiovascular conditions frequently treated in hospitals.
- Real-world Latin American-specific data shows that with operational changes, three ablation procedures could feasibly be performed daily, leaving time for an extra electrophysiology procedure on more than half of days.
- The cryoballoon ablation is an effective tool to enhance electrophysiology lab efficiency in resource constrained regions such as Latin America.
Introduction
Atrial fibrillation is a progressive disease; after some time, patients can experience longer and more frequent episodes despite using antiarrhythmic medication. The incidence and prevalence of atrial fibrillation is rising with an aging population [1,2]. In the Latin American country of Colombia, cases doubled from 41 to 87 per 100 000 people from 2013 to 2017 [3]. The growing drug-refractory atrial fibrillation population has increased the quantity of catheter ablation procedures [4]. Conventional treatment for patients with drug-refractory, symptomatic atrial fibrillation is catheter ablation for pulmonary vein isolation [5,6,7,8]. Cryoballoon ablation was developed specifically for achieving pulmonary vein isolation and has proven safe and effective in the treatment of patients with paroxysmal or persistent atrial fibrillation [9,10,11,12]
The increasing burden of catheter ablation procedures requires deliberate management of limited hospital resources. Procedure times, specialized equipment, dedicated electrophysiology lab usage, and expert personnel are all factors considered when performing catheter ablations. Single-shot techniques like cryoballoon ablation have shorter and more consistent procedure times, allowing for a shorter learning curve [13,14]. Decreased procedure time with cryoballoon catheter ablation has proven beneficial in improving electrophysiology lab efficiencies compared to traditional radiofrequency catheter ablation [15,16,17]. Cryoballoon ablation can be most impactful on electrophysiology lab efficiency in regions such as Latin America that fall behind higher-income regions in electrophysiology lab resources to help accommodate the increased burden of atrial fibrillation [18]. However, more data is needed to assess the impact of cryoballoon ablation on electrophysiology lab efficiency due to operator experience, technological innovations, and the increasing paroxysmal indication in Latin America. This study was designed to assess the current efficiency of electrophysiology labs in Latin America, given the use of the cryoballoon catheter. This analysis also proposes operational changes that could meaningfully improve productivity and resource utilization.
Methods
Procedural measurements within the Cryo Global Registry
The Cryo Global Registry (NCT02752737) is a prospective, global, multi-center, observational post-market registry. The registry aimed to evaluate and describe the clinical performance and safety data in patients with drug-refractory (to class I or III antiarrhythmic drugs) paroxysmal atrial fibrillation (episode duration < six months) treated with the commercially available Arctic Front™ Cardiac Cryoablation Catheter System, according to routine clinical practice [19,20,21]. The registry was conducted at 93 sites in 36 countries, including South America [11]. The present analysis includes procedures performed in public and private facilities in Argentina (Hospital Universitario Fundación Favaloro and Instituto Cardiovascular de Buenos Aires, which provided n = 71 and n = 93 cases, respectively), México (Hospital San Ángel Inn and Centro Médico Nacional Siglo XXI, n = 20 and n= 27 cases, respectively), Colombia (Fundación Clinica Shaio, n = 16 cases), and Chile (Clínica Dávila, n= 5 cases).
Cryoballoon ablation procedures were done according to the standard set at each site. This procedure has been extensively described [6,7,8,10,12,22,23]. In brief, the 23- or 28-mm cryoballoon catheter (Arctic Front Advance, Medtronic, Inc.) was inserted into the left atrium using a steerable sheath (FlexCath Advance Steerable Sheath; Medtronic, Inc.) through a transseptal puncture. Utilizing either a J-tip guidewire or a dedicated mapping catheter (Achieve; Medtronic, Inc.) the cyroballoon catheter was delivered to the pulmonary vein. Once the vein ablation was initiated, the operator determined dosing and duration. Pulmonary vein isolation was exhibited by electrical isolation of the pulmonary veins from the left atrium after cryoablation. Post-procedure testing was done, and patients were discharged according to local hospital standard policies.
Time measurements from the Cryo Global Registry were retrieved to assess the electrophysiology lab usage, including total procedural time and total lab occupancy time. The time from initial venous access to final sheath removal was measured and defined as the total procedural time. While the total electrophysiology lab occupancy time was defined as the time elapsed between the patient entering and leaving the electrophysiology lab. Lab occupancy time is an independent variable unaffected by external operational events such as administrative delays or management of the operating lab and its physical or human resources. Time estimations presented herein represent the observations from the sample of sites in Latin America and will be applied as input parameters for the two tested scenarios in combination with proposed operational improvements using a discrete event simulation model.
Discrete event simulation model operation
The electrophysiology lab utilization was modeled using a discrete event simulation. The simulation aims to evaluate how operational changes in the electrophysiology laboratory can lead to enhanced productivity.
Discrete event simulation is a modeling method designed to represent a wide range of interactions within the healthcare system co-occurring in a real-world environment [24,25]. Discrete event simulation models are based on stochastic time series of individual, granular events representative of realistic interactions of its core elements: Entities, attributes, events, resources, queues, and time [26]. Entities trigger events (e.g., people or critical resources). A pathway is traced for them based on a probabilistic characterization derived from real-world data and experience, in which they consume resources and enter queues over time. This method is advantageous for modeling the efficient use of resources in provider settings. The model aims to explore how earlier start times, later end times, and more efficient management of supply and operating room turnover between patients could increase productivity from two cryoablation procedures to three per day.
The model used for this analysis has been previously described [27,28]. In brief, entities – represented by patients, physicians, and support staff – and the electrophysiology lab can affect lab occupancy times for procedures by incurring delays and contributing to distortions in the expected start times. These estimations are drawn from defined distributions (Table 1).
The Lab occupancy time utilized in both scenarios is derived from actual measurements from the Cryo Global Registry. As displayed in Table 1, lab occupancy time remains unaffected by operational events external to the surgical procedure, behaving as an independent variable to environmental changes. No technological or physician technique changes are being modeled; thus, lab occupancy time remains the same for both scenarios.
The differences between both scenarios lie in the modifications of operational activities accompanying surgical work. Administrative or operational tasks include the operating room schedules' start and end times, the time required to prepare, clean, and equip the operating room for a new patient, and delays dependent on the professional or related to the patient.
A pulmonary vein isolation procedure began in the discrete event simulation after patient and physician delays were accounted for (i.e., all entities were simultaneously available), and its total duration was selected randomly from the probability distribution of lab occupancy times reported in the STOP Persistent atrial fibrillation trial. After the lab occupancy completion time, all entities were released back into the model, and the process was repeated for all procedures pre-planned for a given day according to either block or as-available room scheduling practices retrieved in local explorations for the sample of countries (Figure 1).
Discrete event simulation model operation.
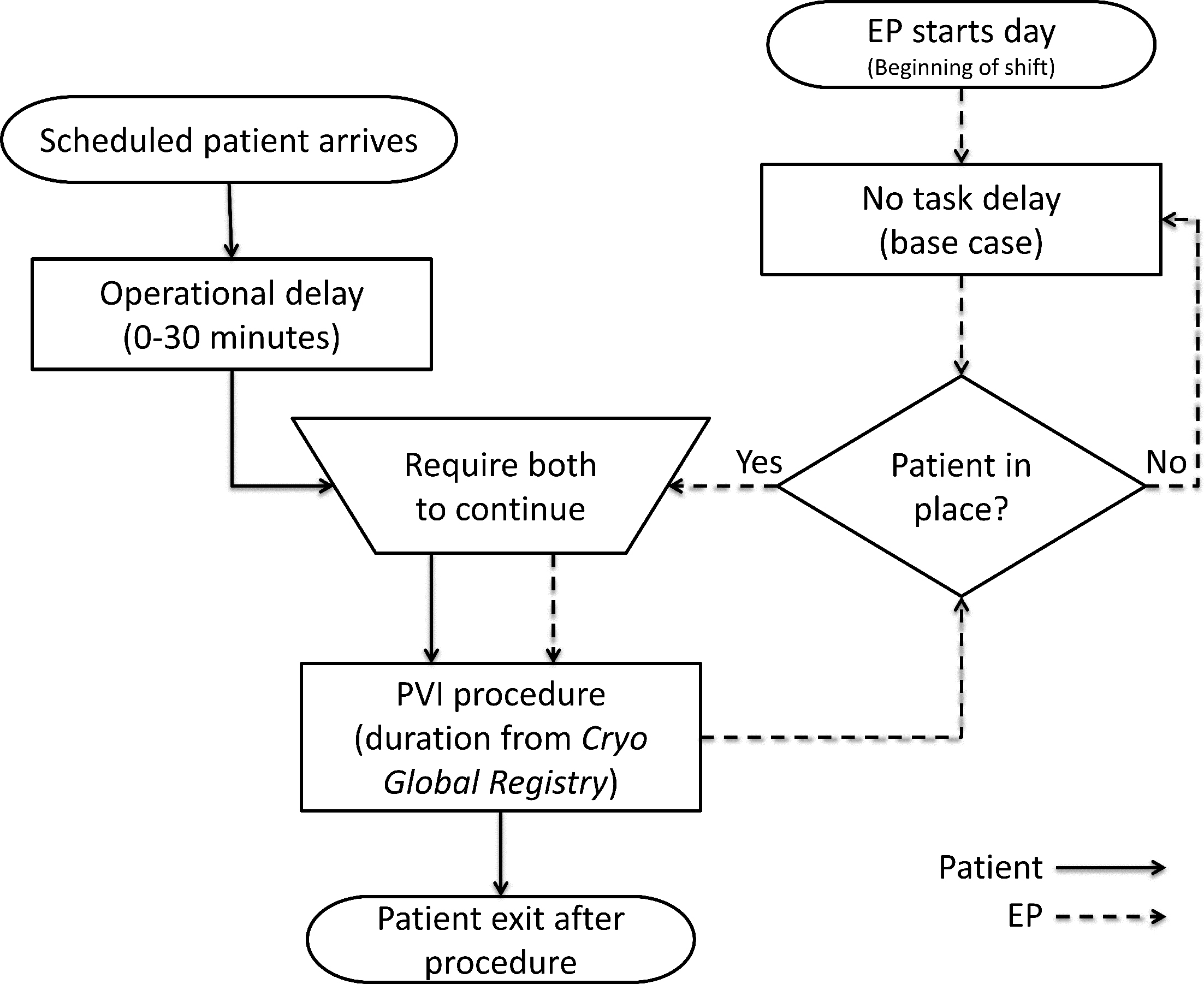
Source: Prepared by the authors for this study.
The simulation was conducted for 1000 days accounting for variations in all model parameters simultaneously. The current practice and enhanced productivity scenario were modeled, considering moving from two pulmonary vein isolation cases per day to three, changing the first case start time and overtime begin time, and reducing room turnover time.
The metrics collected from the discrete event simulation included the percent of days in which the pre-planned pulmonary vein isolation procedures led to overtime or resulted in excess time for one or two additional non-ablation cases in the electrophysiology lab (e.g., pacemaker implants, implantable cardioverter defibrillator replacements, etc.). This analysis used SIMUL8 professional version 26.0 (SIMUL8 Corporation) for discrete event simulation.
Model inputs
The lab occupancy times from all Latin American patients in the Cryo Global Registry were included and represented all ablations performed for pulmonary vein isolation and any non-pulmonary vein isolation ablations. For the current scenario, it was assumed that only two pulmonary vein isolation cases could be completed in one lab day, and operational parameters were changed to demonstrate what would have to be true to accomplish three pulmonary vein isolation cases per day to represent an enhanced productivity scenario. For both scenarios, it was assumed that the electrophysiology lab operated on dedicated pulmonary vein isolation days (i.e., no other procedures were performed other than pulmonary vein isolation). The assumptions and parameters for the number of daily procedures, first case start, overtime begin, time for add-on case, room turnover time, and delays, have been referenced from Kowalski, M. et al. (2021). Furthermore, these parameters were validated by a panel of eight electrophysiology experts from countries involved in the Cryo Global Registry: Chile, Argentina, Colombia, and Mexico. These data were combined as inputs to the model for the simulation of each scenario.
Current scenario
For the current scenario, the first procedure was scheduled to begin at 8:30 am, and the second procedure was scheduled to begin as soon as possible after the first case plus electrophysiology lab turnover time. Operational delays based on qualitative research were assumed in the model, including: 1) room turnover time of 45 minutes, and 2) patient delays between 0 to 30 minutes. No physician delay was modeled. Physicians were assumed to be focused on the pulmonary vein isolation procedures and immediately available for each case. Overtime was assumed to begin at 4:00 am.
Enhanced productivity scenario
A hypothetical enhanced productivity scenario was designed to show what would have to be true for an electrophysiology lab in Latin America to accomplish three pulmonary vein isolation cases in a day without an unreasonable overtime burden. In this scenario, the shifts for staff would be extended with the first case scheduled for 7:30 am and overtime to begin at 5:00 pm. The electrophysiology lab turnover assumption was reduced to 30 minutes, with all other inputs remaining the same as the current scenario. The model inputs for both scenarios are summarized in Table 1.
Model validation and sensitivity analysis
A sensitivity analysis is a technique used to understand how changes in study parameters affect the outcomes of a model. A deterministic sensitivity analysis was performed to evaluate the effect of parametric uncertainty or variations on the nominal and high-efficiency use cases by independently changing each of the individual time components, such as the mean lab occupancy time, operating room turnover time, and lab shift end. All other assumptions and inputs were maintained constant. Table 1 displays the values of the variables considered in this sensitivity analysis. For this sensitivity analysis, for each parameter above, a number labeled as "High" represents the high end of the range for the variables. At the same time, "Low" is numerically lower than the value corresponding to the base case. A probabilistic sensitivity analysis was not deemed necessary due to the inherent stochastic nature of Discrete Event Simulation (DES).
Statistics
Pearson 5 distributions were used to characterize the variability in lab occupancy time. After 1000 lab days of base simulation, mean simulated lab occupancy times were, with a 95% confidence level, within 3% of the expected mean generated from the clinical trial. The percentage of days resulting in overtime, or the amount of time left for adding operations were the key model outputs. The mean, 10th percentile, and 90th percentile are presented for all descriptive raw lab occupancy time data.
Results
Electrophysiology lab occupancy time distributions
The lab occupancy time distribution for all use cases in this manuscript were derived from the subset of sites in the Cryo Global Registry dataset in Latin America, including 232 procedures from six study sites. These patients' clinical characteristics, treatment details, and clinical outcomes were previously published [10].
Site-specific average lab occupancy times ranged from 91 to 279 minutes across the trial sites (Figure 2A). The average lab occupancy time was 132 ± 62 minutes, with a 10th percentile of 75 minutes and a 90th percentile of 230 minutes (Figure 2B). Detailed procedure time distributions were fit to a Pearson five distribution (online supplementary figure 1) as input to the simulation model. These time estimations are applied to both scenarios.
Lab occupancy times derived from the
Source: Prepared by the authors of this study
Electrophysiology lab efficiency outcomes
A simulation of 1000 electrophysiology lab days was performed for each scenario. The current scenario simulation represented 2000 total pulmonary vein isolation procedures and resulted in cases that required overtime work in 74 (7.4%) of the simulated days, while 814 (81.4%) of the simulated days finished pulmonary vein isolation cases early enough to allow time for an extra non- pulmonary vein isolation procedure without overtime. The enhanced productivity scenario simulation represented 3000 total pulmonary vein isolation procedures and resulted in cases that required overtime work in 164 (16.4%) of the simulated days, while 674 (67.4%) of the simulated days finished pulmonary vein isolation cases early enough to allow time for an extra non- pulmonary vein isolation procedure without overtime (Table 2).
Influence of operations on lab efficiency
A representative simulated case regarding time distribution for the current scenario is included in Figure 3A, while Figure 3B is representative of the enhanced productivity scenario.
Duration of pulmonary vein isolation cases per day.
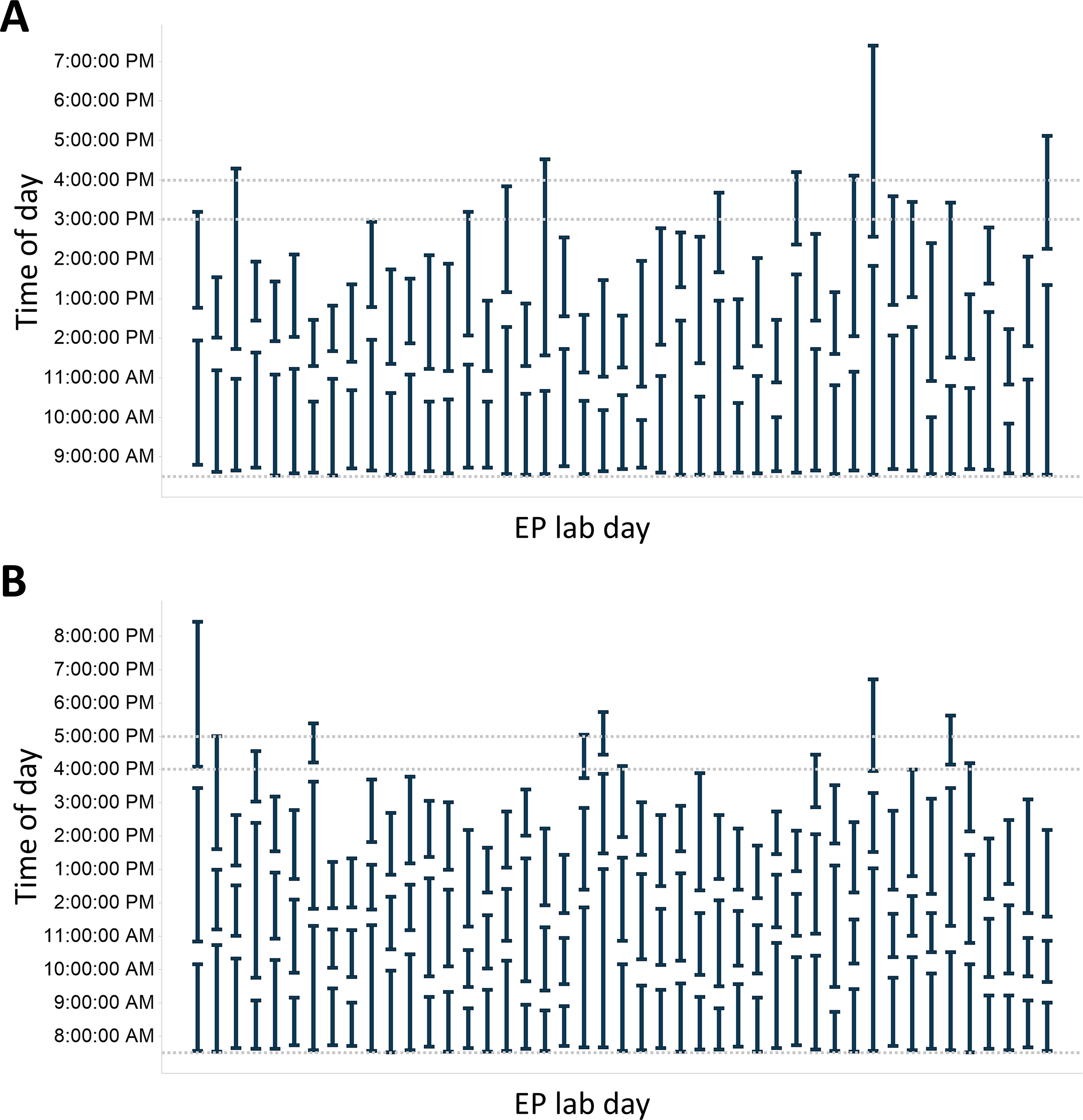
Abbreviation: EP, electrophysiology.
Source: Prepared by the authors of this study.
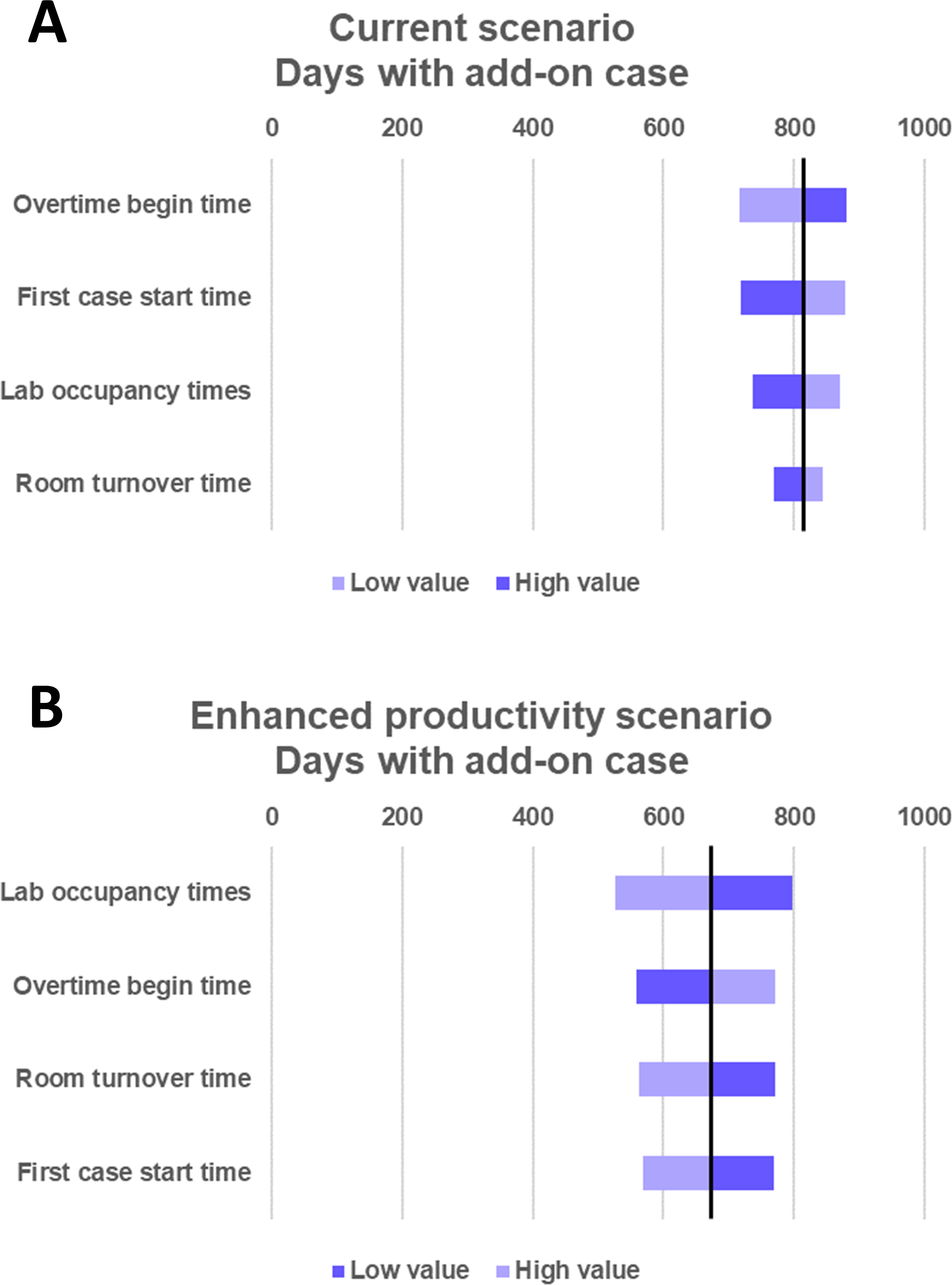
The sensitivity analysis results for the overtime days metrics are shown in Figure 4 and the results for add-on case metrics are shown in online supplementary figure 2. The simulation model was most sensitive to changes in overtime begin time for the current scenario, and lab occupancy times for the enhanced productivity scenario; however, the overall results remained directionally consistent for all simulations in the sensitivity analysis.
Sensitivity analyses.
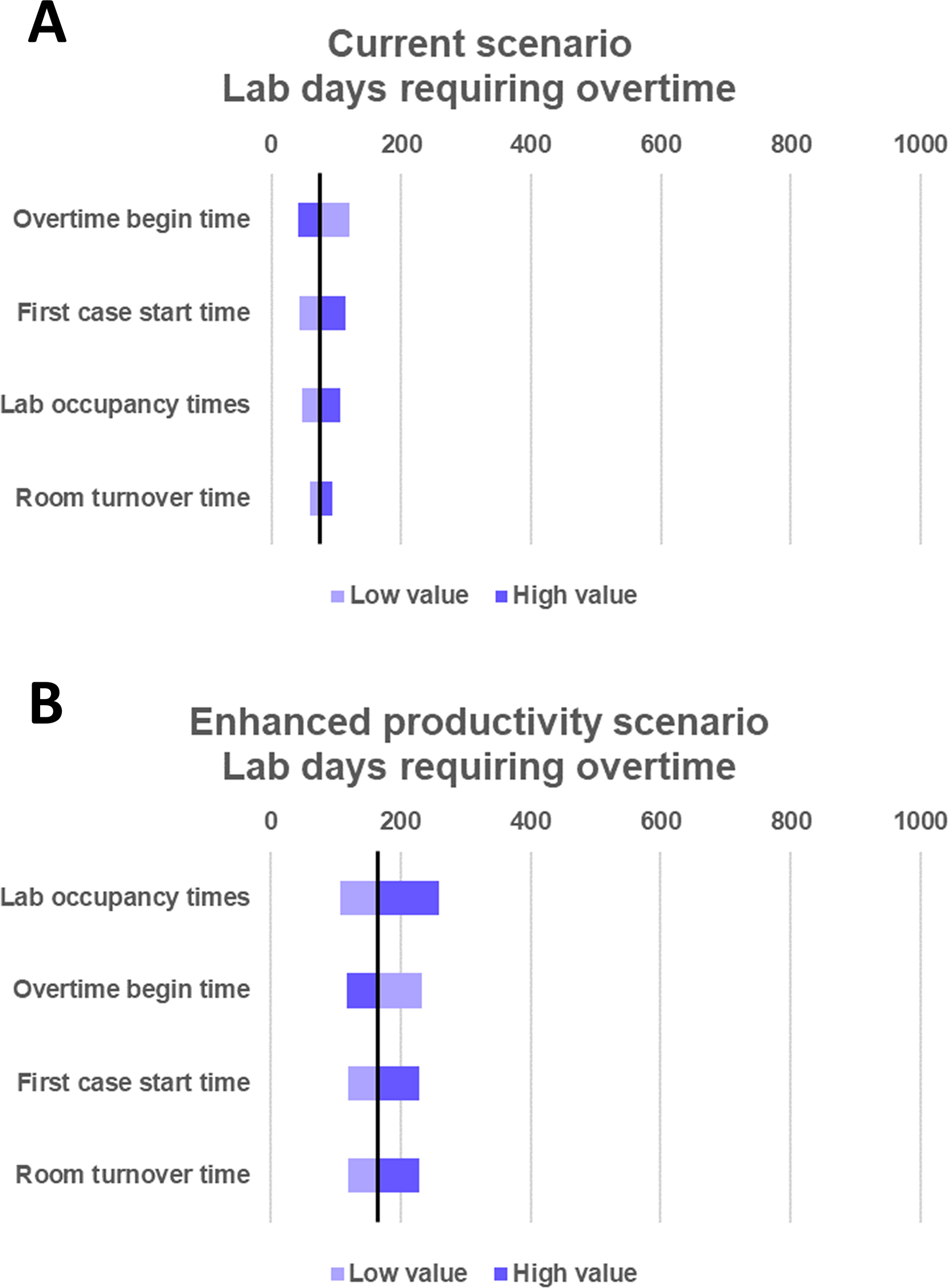
Source: Prepared by the authors of this study.
Discussion
This analysis explored current and potentially achievable electrophysiology lab efficiencies when using cryoballoon technology to perform pulmonary vein isolation ablation procedures, specifically in the Latinamerican region, based on data from the Global Cryo Registry. Currently, with an average lab occupancy time of 132 minutes and a lab day that runs from 8:30 am to 4:00 pm, cryoballoon enables two pulmonary vein isolation cases per lab day with minimal intrusion of overtime for staff (7.4% of days) and consistent opportunity to do extra non- pulmonary vein isolation cases with the same resources (81.4% of days). By extending the lab day incrementally from 7:30 am to 5 pm, an increase in productivity of 50% (from two to three cases per day) is feasible with low overtime and good capacity for extra non-pulmonary vein isolation cases.
There was notable variability among the average procedure times by site (average lab occupancy times by site ranged from 91 to 279 minutes). The highest and lowest measures per site came from sites with relatively few procedures, which may limit the accuracy of interpreting the data at the site-specific level. Nonetheless, lab occupancy times can be affected by different variables, such as previous operator experience, the procedure learning curve, and each center’s internal dynamics. The sensitivity analysis found that the main results of the analysis were not overly sensitive to changes in the lab occupancy time within reason.
Pulmonary vein isolations using catheter ablation can be unpredictable since many variables interact: creation of geometries, voltages and maps, and cartography, among others. This volatility can lead to a wide range of procedure times depending on the case’s complexity. With the advent of "one shot" device, including cryoablation, these variables and the time they take are much more predictable due to the simplicity of the technique. For example, Velagic and colleagues showed that point-by-point radiofrequency ablation had an average procedure time of nearly 192 minutes with substantial variation (± 101.1 minutes), while cryoballoon ablation was significantly shorter with much less variation (116.6 ± 39.8 minutes) [14].
The efficiency advantages of an anatomical approach enabled by current cryoballoon technology as opposed to a point-by-point approach significantly reduce lab occupancy time for pulmonary vein isolation procedures [15,16]. Direct comparisons of anatomical vs point-by-point demonstrate improvements in overtime avoidance and increased use of fixed lab resources in the United States for paroxysmal atrial fibrillation using first-generation catheter technologies [27], and in Europe for paroxysmal and persistent atrial fibrillation procedures using newer generation technologies [29]. Analyses looking specifically at the anatomical approach estimate that overall lab throughput can reasonably be increased by 50% (from two to three pulmonary vein isolation procedures per day) both in the United States [28] and in Europe [29]. The current analysis uses similar methodology with Latin America-specific procedure data from the global cryo registry to demonstrate that the efficiency gains previously seen can be extended to the region.
While the measures of this analysis, overtime days and days with time for non-pulmonary vein isolations, have meaning for hospital administrators, the specific impact may vary between institutions and countries. When considering overtime in private institutions, this is likely to be a direct measure regarding extra staff costs and the inconvenience of unplanned extra work hours for the staff themselves. Public institutions typically cannot afford overtime, leading to canceled cases to avoid additional costs. This results in fewer procedures on that day and scheduling difficulties, ultimately causing longer patient wait times. When considering days with time for a non-pulmonary vein isolation case, having a consistent resource available for additional procedures enables advance planning to use that resource, first serving more patients with appropriate indications for these treatments and benefitting the hospital by creating more value from a fixed resource cost.
In Chile, a recent analysis of elective surgeries has demonstrated that public providers perform 3.3 general elective surgeries per day (utilization rate of 53%, equivalent to 4.8 hours out of nine working hours), with an average delay of 40 minutes for the first case. Also, operating rooms finish shifts two hours early [30]. These results have driven a sectorial agenda towards efficient surgical resolution models, emphasizing ambulatory surgical models.
There are numerous challenges to the efficient operation of an electrophysiology lab in Latin America. In many South American countries, the electrophysiology laboratory is not exclusive to electrophysiology procedures and is shared with other cardiology and medical specialties. Shared operating rooms also impact their equipment, specifically polygraphs or cryo-consoles. In some models, these are supplied by the service provider, depending on the availability and scheduling. Although high-volume hospitals satisfy the demand by stable contracts with distributors, that is only the case for some. Especially in low-volume providers, due to the cost of the therapy, the cost-benefit balance is not fully understood by decision-makers, despite studies published in this regard. Nursing and radiology support staff change between departments and are randomly assigned to procedures, complicating training and impacting efficiency. A deficit of qualified personnel for the room’s workflow also affects efficiency, especially during evening shifts and weekends. Because of these challenges, the ideal scenario is far from being achieved.
Reductions in lab occupancy time can create incremental improvements toward the ideal, even given other challenges, and there are good reasons to improve using available pulmonary vein isolation technologies in conjunction with reasonable changes to operating parameters. The conditions explored for modeling the enhanced productivity scenario align with the Chilean national commission for productivity recommendations, which suggested the extension of operating room availability from 7:30 am until 5:00 pm, an increase in physicians' supply for surgeries from 17% to 33% or more of their hired time and increase anesthesiologists supply from 53% to 60% of their hired time also [30]. As suggested by the enhanced productivity scenario, improvements in lab occupancies can enable more procedures. The same Chilean report has estimated that reducing surgical times from 1.5 to 1.2 hours would allow one additional daily surgery [30].
There are limitations in this analysis that should be acknowledged. The results are based on simulations rather than observations. However, the inputs to the simulation are based on real observations from the Cryo Global Registry. These findings are consistent with those from other publications on this topic, and have been supported by a robust sensitivity analysis.
The analysis includes only cryoballoon procedures and is not directly comparable to other technologies; however, there is a strong existing evidence base on the efficiency advantages of cryoballoon. Operator experience was not accounted for, but the distribution of lab occupancy times represented a wide variability, and the registry represented a real-world experience sample. The analysis assumed an electrophysiology lab day dedicated to isolation procedures as the priority, even though some are shared with interventional cardiology, pacemaker implantation, or other electrophysiology procedures.
The analysis includes private and public providers, which might differ in payment systems involved in reimbursing procedures. Payment mechanisms are well recognized for their role in setting incentives for productivity and efficiency. Further lines of investigation could delve deeper into outstanding results and protocols of specific countries, such as Argentina which recorded an average time of 102.1 minutes, that is 29.4 minutes below the region. Finally, this analysis used data and assumptions specific to the region, and the results cannot be generalized to other geographies.
Conclusions
Modeling electrophysiology lab efficiency using Latin America-specific data, cryoballoon ablation easily allowed for two ablation procedures to be performed in one simulated day given currently accepted operational parameters. With reasonable changes to operational parameters, three procedures could be performed without using overtime on most simulated days and even allow time for an extra non-ablation on over two-thirds of simulated days. Increased adoption of the cryoballoon ablation procedure along with efficiency modifications in resource-constrained regions can improve electrophysiology lab efficiency by maximizing the number of procedures performed in one day, which will help accommodate for the rise in atrial fibrillation patients who require the procedure.

