Systematic reviews
← vista completaPublished on September 28, 2018 | http://doi.org/10.5867/medwave.2018.05.7265
The effectiveness of joint mobilization techniques for range of motion in adult patients with primary adhesive capsulitis of the shoulder: a systematic review and meta-analysis
Efectividad de las técnicas de movilización articular sobre el rango de movimiento de pacientes adultos con capsulitis adhesiva primaria de hombro: revisión sistemática y metanálisis
Abstract
OBJECTIVE To determine the effectiveness of joint mobilization techniques in the range of motion in adult patients with primary adhesive shoulder capsulitis.
METHODS Systematic review with meta-analysis. The search was performed in the MEDLINE/PubMed, PEDro, CENTRAL, LILACS, EMBASE, CINAHL, Scopus and Web of Science databases. The eligibility criteria were studies that used an oscillatory and/or maintained joint mobilization technique applied alone or added-on to a treatment program in patients with primary adhesive capsulitis at any stage. Two authors carried out the selection of studies and the extraction of data, independently. Risk of bias was evaluated according to the tool proposed by Cochrane.
RESULTS We included 14 studies with variable risk of bias. Posterior mobilization compared to any other technique was not significantly different (0.95 degrees; 95% CI: - 5.93 to 4.02), whereas compared to a control group, the difference is 26.80 degrees (CI 95%: 22.71 to 30.89). When applying a set of joint techniques versus a control group, for abduction the difference is 20.14 degrees (95% CI: 10.22 to 30.05). In both cases, the results are statistically significant, and the effect size is moderate.
CONCLUSIONS The evidence is not conclusive about the effectiveness of joint mobilization. When compared with treatments that do not include manual therapy, joint mobilization seems to have a favorable effect on the range of motion and pain reduction in patients with primary adhesive shoulder capsulitis.
|
Main messages
|
Introduction
Adhesive Capsulitis is a common musculoskeletal condition characterized by spontaneous onset pain associated with a progressive loss of glenohumeral movement of unknown etiology[1]. Neviaser was the first to use the term adhesive capsulitis, describing it as a chronic inflammation of the synovial membrane with fibrosis of the joint capsule and intraarticular adhesions in the shoulder[2]. Years later, it would be defined by the Consensus of the American Society of Shoulder and Elbow Surgeons as "a condition of unknown etiology, characterized by a significant restriction of the passive and active range of motion of the shoulder that occurs in the absence of an intrinsic pathology known"[3]. Zuckerman proposed a classification system where primary or idiopathic adhesive capsulitis is not associated with a systemic condition or history of damage, that is, there is no preceding event to which the case can be attributed, and from the point of view of diagnosis, it is considered in all cases that the etiology associated or underlying this condition can’t be identified[3],[4].
The knowledge of the natural history of the disease is relevant to evaluate the real effectiveness of the different therapeutic modalities used in the clinical management of this disease. In the case of primary adhesive capsulitis, its benign nature and self-limited course is controversial[5],[6],[7],[8],[9]; Codman and Gray, were the first to affirm that all patients with primary adhesive capsulitis have a complete recovery of pain and range of motion at 2 years after onset of symptoms[10],[11]. However, prospective and long-term studies have reported variable percentages of loss of range of motion, pain and disability in patients with primary adhesive capsulitis[6],[12],[13],[14],[15]. Regarding movement restrictions, the authors report a significant restriction in 90% of patients at 7 months of follow-up[7], and between 30% and 50% of patients present mild and / or moderate restriction in a follow-up of 3 to 10 years[6],[7],[8],[12],[13]. This is relevant, especially when evidence of moderate quality suggests that the theory of self-resolution is increasingly uncertain and that the best therapeutic results are obtained by intervening in early stages, and not late[16].
In this regard, it should be noted that rotational movements, specifically external rotation, have not shown significant changes before 4 weeks of physiotherapy treatment[17]. Some therapeutic interventions such as corticosteroid injection, different modalities of electrotherapy, arthrographic distension, treatment of muscle trigger points and manual therapy techniques have also been recommended for the improvement of range of motion and pain reduction[18],[19],[20],[21],[22]. In recent years, several studies have shown beneficial results using manual therapy techniques to correct the deficits of the glenohumeral rotational range of motion, especially external rotation[23],[24],[25],[26],[27],[28]. These techniques have been shown to be effective in the management of capsular restraints, specifically when provided by a physiotherapist[29].
The literature describes three types of joint mobilization techniques: oscillatory, maintained and manipulative. Oscillatory techniques are repetitive passive movements of varying amplitude and at low-velocity[30],[31],[32]. The maintained mobilizations are a type of traction of variable amplitude and low-velocity, that decrease the intra-articular compressive forces and remove the distention of the periarticular tissues[33]. These have been graded according to the amplitude of the movement and the degree of tension of the periarticular tissue[31],[34]. Finally, manipulation techniques are those that involve high-velocity, low-amplitude movements associated with a "thrust" at the end of the available articular range of motion[31].
From the above, our research questions are born: in patients with primary adhesive shoulder capsulitis, are the techniques of joint mobilization maintained more effective than the oscillatory ones for the improvement of range of motion, pain and function of the shoulder? Do adding articular mobilization techniques to a treatment program produce some improvement in the range of motion, pain and function of the shoulder? Trying to elucidate these questions was what motivated the realization of this systematic review whose main objective is to determine the effectiveness of joint mobilization techniques in the improvement of range of motion, whether applied alone or added to a program of treatment. Secondary objectives are to determine the effect of the techniques on the improvement of function and pain reduction, in addition to the dosage used.
Method
Protocol
The present systematic review will be reported according to the preferred standard for systematic reviews and meta-analysis[35]. It should be mentioned that the protocol prior to carrying out the present review was not registered.
Eligibility criteria
To carry out the systematic review, a search strategy was developed in which the following eligibility criteria were included: 1) Population: patients older than 18 years with a diagnosis of primary adhesive capsulitis at any stage, without distinction of gender or race; 2) Intervention: an oscillatory and / or maintained joint mobilization technique applied alone or added to a treatment program; 3) Comparison: with other techniques of manual therapy, use of physical agents, different modalities of therapeutic exercise or pharmacological treatments; 4) Outcome measures: articles that have evaluated clinical effectiveness through range of motion, function and shoulder pain; 5) Types of studies: randomized clinical trials published in English or Spanish until July 16, 2018.
Inclusion criteria
- Randomized clinical trials comparing the clinical effectiveness between two joint mobilization techniques applied in patients with primary adhesive capsulitis.
- Randomized clinical trials comparing the clinical effectiveness of one or more joint mobilization techniques applied as part of a treatment program in patients with primary adhesive capsulitis.
Exclusion criteria
- Randomized clinical trials that do not describe the type of joint mobilization technique or specify the dose used.
- Randomized clinical trials that study other joint mobilization techniques such as mobilization with movement and / or manipulation.
Information sources
An electronic search was conducted in the following databases: Medline (www.ncbi.nlm.nih.gov/pubmed), PEDro (www.pedro.org.au), Central (www.cochrane.org), LILACS (www.lilacs.bvsalud.org/en), Embase (www.elsevier.com/solutions/embase-biomedical-research echa), Cinahl (www.health.ebsco.com/products/the-cinahl-database echa), Scopus (www.scopus.com/home.uri?zone=header&origin=searchbasic) and Web of Science (www.fecyt.es/es/recurso/web-science), searching from the beginning of each database until July 16, 2018. We also reviewed the reference lists of the included trials and any relevant review articles retrieved in the electronic search, in order to identify any other potentially relevant trial, it should be mentioned that a gray literature search was not conducted in the present review.
Search strategies
To carry out the search in the Medline database, a sensitive search strategy proposed in the Cochrane Collaboration manual was used[36]. The search terms used in this review were obtained from MeSH: «Bursitis», «Physical Therapy Modalities» and «Musculoskeletal Manipulations». They were combined with free text terms: «Frozen Shoulder», «Adhesive Capsulitis» and «Manual Therapy».
The processes are described below:
- “Bursitis” [MeSH]
- Frozen Shoulder
- Adhesive Capsulitis
- #1 OR #2 OR #3
- “Physical Therapy Modalities” [MeSH]
- “Musculoskeletal Manipulations” [MeSH]
- Manual Therapy
- #5 OR #6 OR #7
- #4 AND #8
- Randomized Controlled Trial [pt]
- Controlled Clinical Trial [pt]
- Randomized [tiab]
- Randomly [tiab]
- Trial [tb]
- Groups [tiab]
- #10 OR #11 OR #12 OR #13 OR #14 OR #15
- Animals [mh] NOT Humans [mh]
- #16 NOT #17
- #9 AND #18
For the PEDro, Lilacs, Central, Cinahl, Web of Science, Scopus and Embase databases, the search strategy was carried out by combining the terms previously mentioned in the advanced search option.
Selection of studies
Two of the authors (JZ and FP) carried out the search chain independently, reviewing the title, abstract and complete text of the articles. Only studies that met the eligibility criteria were selected. The disagreements were resolved in a discussion between the authors, and in case of persisting in disagreement, a third independent reviewer (CO) was consulted.
Data extraction
Data extraction for the included trials was carried out as recommended by the Cochrane Collaboration Manual for systematic reviews[36], two reviewers (JZ and FP) independently completed a standardized data summary form, specially designed for this review. The data collected were entered in Rev-Man 5.3, and in case of disagreement or discrepancy, the article was evaluated by a third reviewer (HG) and by discussion of the authors, its final inclusion was decided.
Evaluation of the risk of bias of the included studies
Two reviewers (JZ and FP) independently assessed the risk of bias of included studies, using the Cochrane Collaboration tool for risk of bias, as described in the manual for systematic reviews36. The following domains were considered:
- Generation of random sequence
- Concealment of allocation (selection bias)
- Blinding of participants and staff (performance bias)
- Blinding of outcome assessment (detection bias)
- Incomplete outcome data (attrition bias)
- Selective report of results (report bias)
- Other sources of bias, each of these domains was evaluated as "low risk", "high risk" or " unclear risk".
A study classified as high risk would not be excluded from this review, but it could degrade our recommendation confidence. The information obtained was used through a presentation of multiple analyzes, from all the studies obtained and that allowed for their quantitative analysis.
Summary measures
For the present review only continuous variables (range of motion, pain and function scales) were identified, so the difference in means between the intervention groups with 95% confidence intervals was used as the main summary measure, in order to determine the effect size of the results. To carry out this process, the final value and the standard deviation of the result of interest were recorded, as well as the number of participants for each treatment group at the end of the follow-up.
Summary of results
The synthesis of results was performed through meta-analysis, which were carried out in the Rev-Man 5.3 program. In the case of clinically homogeneous studies, the heterogeneity was evaluated with the chi2 statistical test and the I2 heterogeneity test. We consider a low heterogeneity a chi2 value with a P > 0.1 and the I2 test with a value less than or equal to a 50%, in this case a fixed effect model was used for the analysis of the data, with inverse variance weighting. On the contrary, a random effect model was used when there was high heterogeneity.
Additional analysis
We performed the meta-analysis based on two comparisons. First, we grouped the Randomized clinical trials that included the subsequent mobilization grade III according to Kaltenborn and, secondly, the studies that included within their intervention a set of Joint mobilization. In both comparisons, analysis by subgroups was considered, based on the comparison with other joint mobilization techniques and with a conventional treatment that did not include joint mobilization techniques.
Results
Study selection
According to the defined search strategy, 563 records for terms and keywords were identified, of which 225 were duplicates. After analyzing the titles and abstracts of the remaining, only 25 articles met the eligibility criteria, which were reviewed in full text. After analysis of the selection criteria, 11 studies were excluded for various reasons, all presented in Figure 1, and the remaining 14 studies were included in the qualitative synthesis process[37],[38],[39],[40],[41],[42],[43],[44],[45],[46],[47],[48],[49],[50].
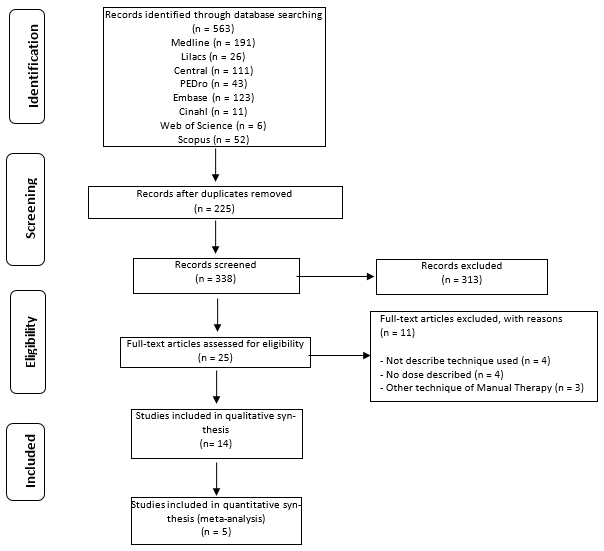 Full size
Full size Study characteristics
Considering the 14 selected randomized clinical trials, the total number of patients was 474, with an average of 24 patients per study and a range between 14 and 100 patients. The average age in the studies was 46.9 years, with a range between 35 and 70 years. After analyzing the included articles, the articular mobilization techniques studied could be grouped based on two comparisons. They are comparing the clinical effectiveness between two joint mobilization techniques[38],[39],[40],[41],[42],[44],[45],[50], and those comparing the clinical effectiveness of one or more joint mobilization techniques applied as part of a treatment program[37],[43],[46],[47],[48],[49], the schematic representation of these comparisons can be seen in figures 2 and 3.
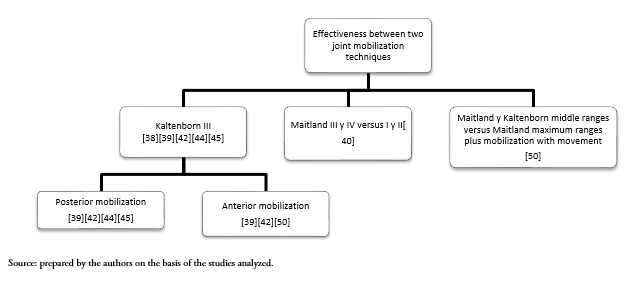 Full size
Full size 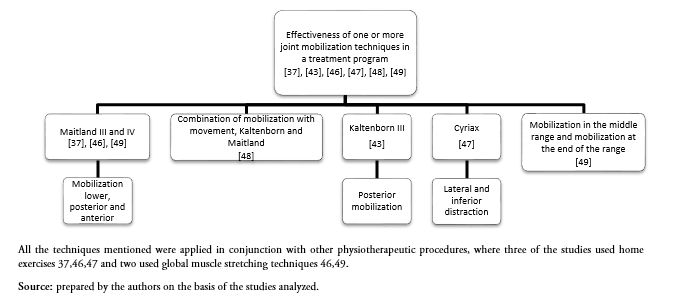 Full size
Full size Results of Individual Studies
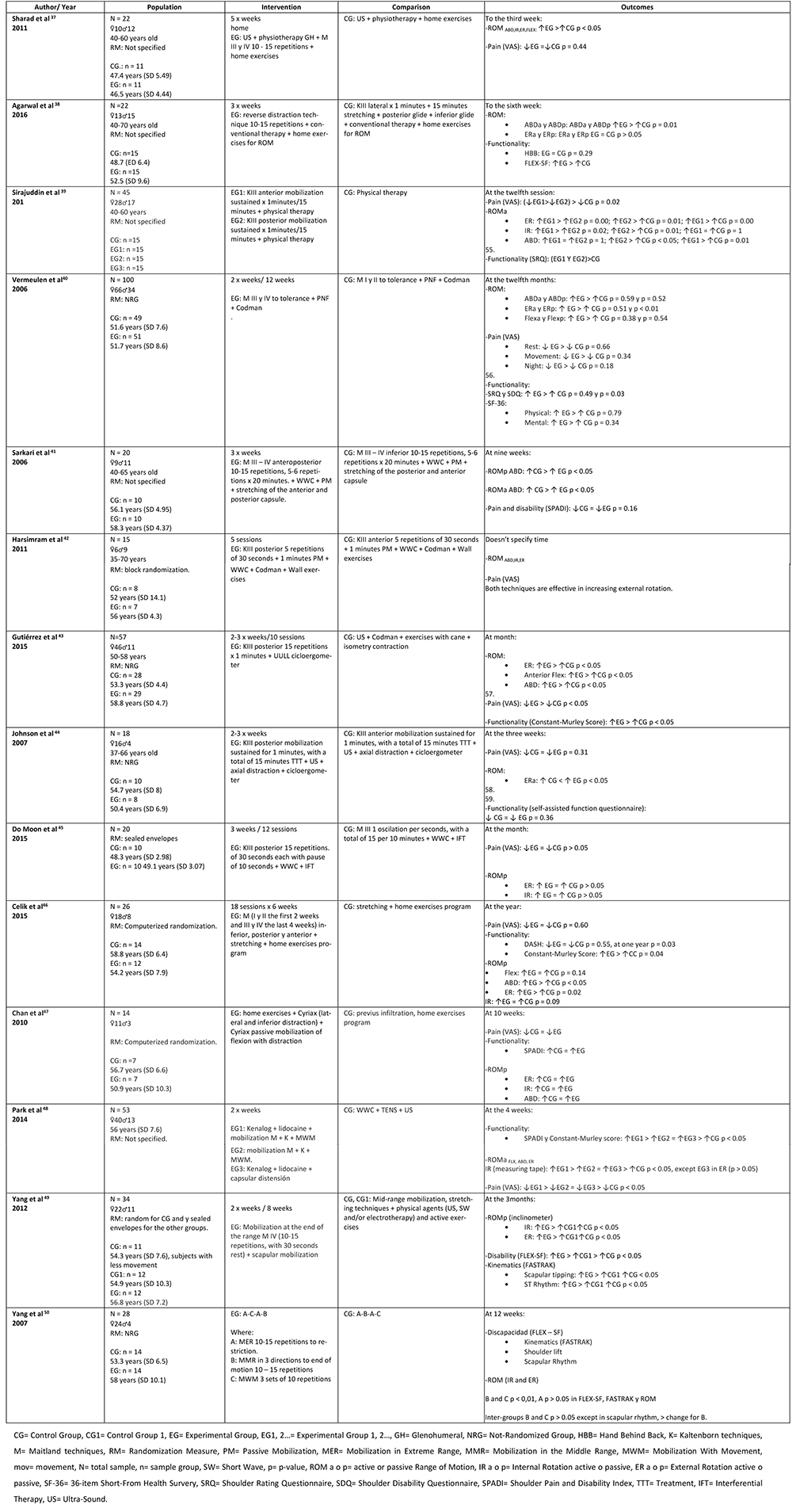
The results of each of the included studies are summarized in Table 1.
Risk of bias of the studies
The risk of bias of the studies included in this review is presented in Figure 4 and 5. Only eight of the selected studies reported details of random sequence generation[40],[42],[43],[44],[45],[46],[47],[50], and the allocation concealment in only six[41],[43],[44],[45],[46],[47]. Given the nature of the interventions studied, blinding of patients and the treating is complex, at this point three studies were rated high risk[37],[39],[43], and the remaining unclear risk.
 Full size
Full size 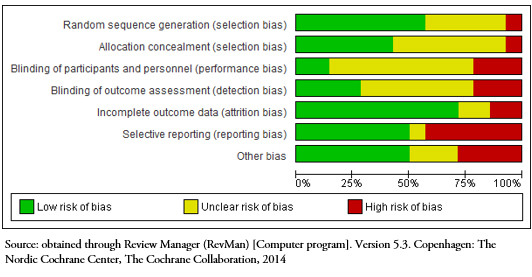 Full size
Full size 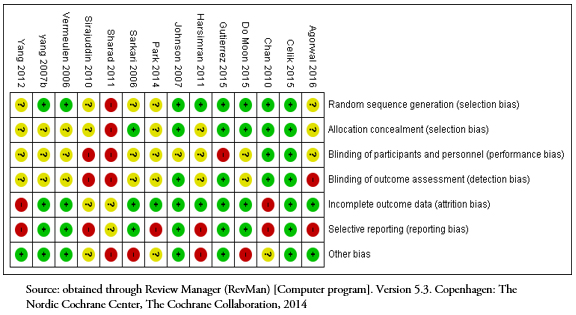 Full size
Full size Measures of results of the studies
Considering that the restriction of movement is a pathognomonic sign of primary adhesive capsulitis, the range of motion was considered as the primary outcome measure for the present systematic review. All included studies evaluated glenohumeral range of motion through goniometry, with special emphasis on osteokinematic movements of external rotation and shoulder abduction. Considering the maladaptive and pathophysiological changes of primary adhesive capsulitis on tasks involving the shoulder joint complex[38],[40],[41],[43],[44],[46],[50], shoulder function and pain are considered as secondary outcome measures. The first was assessed in 10 of the studies, through different questionnaires such as Constant-Murley[43],[46],[48], The Disabilities of the Arm, Shoulder and Hand[46], Hand behind back[38], Shoulder Pain and Disability Index[41],[46],[47],[48], among others. Pain was assessed through the visual analogue scale, in 10 of the 14 studies[37],[39],[40],[42],[43],[44],[45],[46],[47],[48].
Meta-analysis of the results
Range of movement glenohumeral
Three of the included articles evaluated glenohumeral external rotation[38],[43],[45]. Comparing posterior mobilization versus other joint techniques, the figure 6 shows that the results of the meta-analysis with a fixed effect model, there was no statistically significant difference in the range of motion of external rotation at the end of treatment mean difference – 0.95° (confidence interval 95 %: - 5.93 a 4.02; p = 0.71). When comparing posterior mobilization versus conventional treatment, there was a statistically significant difference in favor of the posterior mobilization, resulting an average difference of 26.8° (confidence interval 95 %: 22.71 a 30.89, p = < 0.05). In considering the overall effect with high heterogeneity (I2 = 97 %) could not make a significant difference (p = 0.43) in favor of external rotation posterior mobilization.
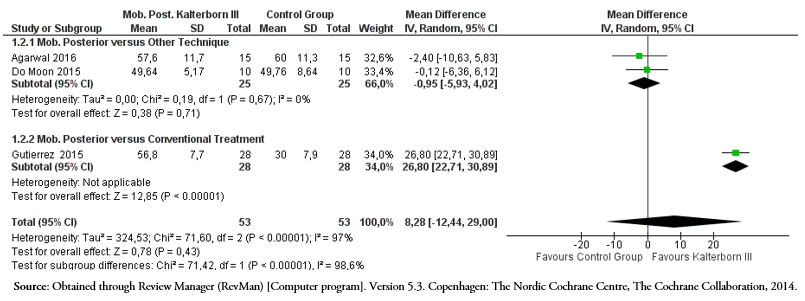 Full size
Full size Two of the included articles evaluated glenohumeral abduction[38],[43]. Comparing the posterior mobilization versus the reverse distraction, the figure 7 shows that there was a statistically significant difference in favor of the posterior mobilization with an mean difference of 25.5° (confidence interval 95 %: 32.97 a 18.03, p < 0.05). When compared with a conventional treatment, the mean difference is 21.9° (confidence interval 95 %: 17.59 a 26.21) in favor of the posterior mobilization (p < 0.05). When considering the total effect with a random effect model due to high heterogeneity (I2 = 99 %), a significant difference (p = 0.94) in abduction could not be established in favor of the posterior mobilization.
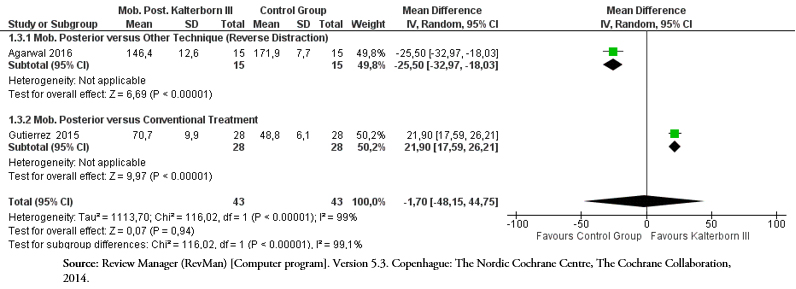 Full size
Full size When comparing a treatment program that included joint mobilization techniques versus a control group, the figure 8 shows that with a fixed effect model there was a statistically significant difference of 20.14° (confidence interval 95 %: 10.64 a 33.56) in the range of glenohumeral abduction in favor of studies that included a set of joint techniques within their intervention compared to a control intervention (p < 0.05).
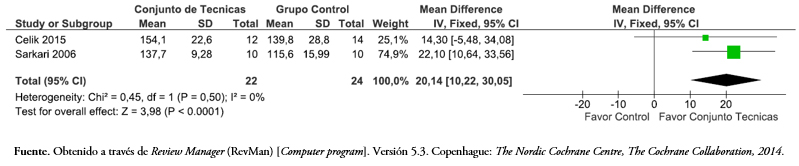 Full size
Full size Shoulder function
Two of the included articles evaluated the function of the shoulder with Constant-Murley[46],[48]. When comparing a treatment program that included joint mobilization techniques versus a control group, the figure 9 shows that with a fixed effect model there was a statistically significant difference of 13.86 points (confidence interval 95 %: 6.38 a 21.34) in the questionnaire Constant-Murley in favor of the joint use of joint techniques compared to a control intervention (p < 0.05).
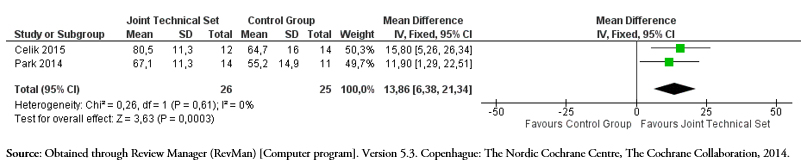 Full size
Full size Pain
Five of the included articles evaluated the pain intensity with the visual analogue scale[38],[39],[43],[44],[45]. When comparing subsequent mobilization versus other joint techniques, the figure 10 with a random effect model due to high heterogeneity, shows that there is an mean difference of 1.26 cm (confidence interval 95%: - 2.14 a 4.66), and versus anterior mobilization is -0.23 cm (confidence interval 95%: - 1.46 a 1), in both comparisons the difference was not statistically significant (p> 0.05). On the contrary, when compared to treatments that do not include joint mobilization techniques, there was a mean difference of - 1.21 cm (confidence interval 95%: - 1.74 to - 0.68) in favor of the posterior mobilization (p <0.05).
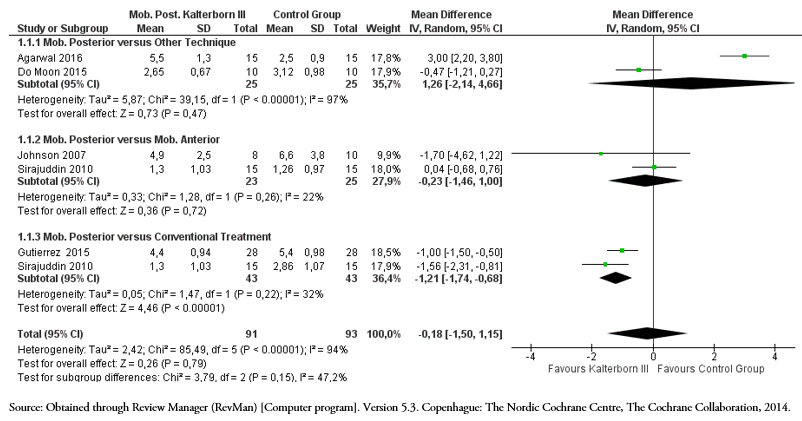 Full size
Full size Discussion
The present systematic review with meta-analysis was conducted on 14 randomized clinical trials, and aimed to determine the effectiveness of joint mobilization techniques applied alone or added to a treatment program, in the improvement of the range of movement, function and shoulder pain. The results showed that the evidence is not conclusive in the use of joint mobilization techniques, despite the high heterogeneity and risk of bias of the articles included, the Kaltenborn type III technique shows a tendency to increase the range of external rotation, abduction and pain reduction compared to a control group, although without statistically significant differences. The use of joint mobilization techniques added to a treatment program showed statistically and clinically significant results for abduction and shoulder function when compared to control groups in patients with primary adhesive capsulitis.
According to previous systematic reviews that have evaluated the effectiveness of joint mobilization techniques, the results have shown an increase in the range of motion and decrease in pain[22]. And when they are compared with conventional treatments they have shown moderate changes in the range of shoulder movement, especially in external rotation (p < 0.05), in favor of posterior glide, showed an average increase of 26.8° (95% confidence interval from 22.71 to 30.89). Although this difference does not occur when comparing two joint mobilization techniques (p = 0.71). Considering the high heterogeneity of the studies, it can not be assured that these changes depend only on the technique, given that it has not been possible to identify a single, minimum or necessary dosage to obtain these improvements. However, the most relevant clinical results were obtained in those experimental groups that were subjected to high-mobilization techniques and performed at the end of the available range of motion[37],[38],[39],[43],[45],[46],[49],[50].
Considering that the restriction of the rotational movement is one of the most common clinical characteristics, this deficit can be prolonged beyond the restrictive phase, and persist for a period of 2 years, affecting more external rotation than the other movements of the shoulder[51] The restrictions of the periarticular tissue[38],[39],[44], and the consequent dysfunction of the muscles that stabilize and mobilize the glenohumeral and scapulothoracic joint, has its origin in the increase of tension of the rotator interval and directly affects to the joint complex of the shoulder in all its planes of motion[52]. Changes in translation and rotational movement of the humeral head determine a pathomechanical movement characterized by an elevation and anteriorization of the humeral head with respect to the glenoid surface, affecting its arthro-osteokinematic. This could explain why humeral rotations end up being the most restricted movements in conjunction with abduction, which does not always show statistically significant changes[39],[40],[47].
Despite the knowledge and the large number of published trials, it has not been possible to identify or establish a dosage for the techniques found, either as a single treatment or as part of an intervention program. When analyzing the complementary treatments to the applied techniques, a study that added stretching techniques to the articular mobilization of Maitland grade IV[46], showed favorable results in both groups, with significant changes in favor of joint mobilization in the range of motion , a similar situation observed in another study that added Kaltenborn III and Maitland III techniques to the application of physical agents[45], which showed significant changes for the two groups but without statistically significant differences between them. In those studies that used Maitland techniques (in all grades) associated with an exercise program[46], and Maitland III and IV techniques associated with muscle stretches[41], statistically significant improvement in the range of motion of the muscles was shown abduction. Similar to a study that added scapula mobilization, and that in addition to improving the range of abduction movement, also showed improvement in glenohumeral external rotation[49].
The dosage of the techniques used in the different studies is varied, observing that the frequency of repetitions of the same technique to complete a treatment session, in the case of Kaltenborn techniques, range from 5 to 15 repetitions, with a time of maintenance from 30 seconds to 1 minute[38],[39],[43],[46], showed positive changes in the groups treated. The total time of application of the technique was 15 minutes, with the exception of one study that considered 20 minutes[48]. On the other hand, those who used the Maitland techniques describe 2 to 15 repetitions, whose frequency was mentioned in only two studies[45],[46], which range from 1 to 2 oscillations per second, with a total treatment time 20 minutes. Two of the included studies propose 10 to 15 repetitions for joint mobilization techniques, but it does not report the specific techniques[38],[50].
Regarding the direction, the authors who used Kaltenborn techniques studied it anteriorly, posteriorly and laterally[40],[42], demonstrating that in those studies where the technique was used in a posterior the improvement of the range of motion of external rotation was statistically significant[38],[39],[43],[44], this contrasts with the results of the study by Do Moon et al[45], where no statistically significant changes were reported when comparing Maitland grade III in different directions.
High-grade joint mobilization techniques, whether from Maitland III - IV or Kaltenborn grade III, aim to restore arthrokinetic movement through distention and elongation of the periarticular structures, increasing the tension of some capsular and ligamentous components, that passively stabilize the joint[53]. This concept alludes to the physical components of the length - tension curve, which studies the behavior of tissues when it is subjected to a load, demonstrating that its properties vary progressing from an elastic phase to a plastic phase, depending directly on the degree, time and dosage of the mobilization, as well as the relative position of the joint[54]. On this depends the remodeling of collagen fibers and the modulation of the properties of the affected connective tissue[50], when analyzing the studies that used techniques in the final range and high stress level in a posterior, all obtained improvement in the range of movement, especially external rotation, but not for abduction (p = 0.94).
This postulates that the magnitude of the technique and the direction in which it is performed, can determine a greater or lesser change, where the posterior sliding influences to a greater degree in the capsular restriction, positioned the joint and increasing the elongation of the joint capsule. which would not be sufficient to show a determinant effect in the movement of abduction, product of the elevation of the humeral head and the increase in the thickness of the inferior fibers of the joint capsule[39],[40],[47] Nevertheless, Articular mobilization techniques achieved significant improvements in the abduction range when compared with control groups, achieving an average increase of 20.14° (95% confidence interval 10.64 to 33.56).
One of the characteristics to consider and that only one study consigned in its inclusion criteria[43], was the degree of irritability of the subjects. Kelley et al[1], propose a classification system in this regard, where a low degree of irritability is one that presents pain less than or equal to 3 cm according to the visual analogue scale, without nocturnal pain or at rest, and with similar limitation of pain, range of active and passive movement. On the other hand, a high degree of irritability implies suffering from pain greater than or equal to 7 cm of visual analogue scale, mainly during passive mobility, with night and rest pain, associated with high levels of disability, with pain predominating over the restriction of range of movement.
This finding becomes relevant at the time of the assignment of a treatment, since some patients will not tolerate the degree of mobilization if their level of irritability is high, mainly because the tolerance to mechanical loads is low. Given that the techniques of high degree of mobilization are based on a micro-injury[37],[43], it is probable that when they are performed, the clinical manifestation is negatively influenced, reflected in an increase in pain. Its phase-dependent applicability could be a subject of study, endorsing its application in phases where rigidity predominates over pain[40],[43].
Limitations
The trials identified for this review studied a wide variety of joint mobilization techniques, this added to the risk of bias and the heterogeneity that limited the possibility of grouping a greater number of results. In addition, the great variability that the studies presented in the dosage of their interventions (type of technique, number and frequency of sessions), made it difficult to identify optimal doses for the application of some joint mobilization in patients with primary adhesive capsulitis of the shoulder. Within the methodological limitations, despite the use of eight electronic databases and the tracking of references of the relevant studies, it is possible that some studies have been overlooked. We did not consider searching for gray literature and we also selected only studies in English or Spanish. We also could not assess the risk of publication bias due to the limited number of trials.
Conclusion
In summary, after analyzing 14 randomized clinical trials that used joint mobilization techniques, with variable methodology in relation to potential sources of bias and statistically heterogeneous. When applied alone or as part of a treatment program, compared to treatments that do not include joint mobilization, they seem to improve range of motion, function and decrease pain. There was no evidence to support or refute a clinical difference of any type of technique over another, nor is there enough evidence to determine the ideal dose of the different techniques of joint mobilization occupied in the different randomized clinical trials in patients with primary adhesive capsulitis.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Authors’ contribution
JZG: Conceptualization, Methodology, Data Validation, Formal Analysis, Research, Materials, Data Management, Writing (Preparation of the original draft), Writing (Revision and editing), Revision and presentation, Supervision, Project Management.
FPB: Conceptualization, Writing (Preparation of the original draft), Writing (Revision and edition), Revision and presentation.
HGE: Conceptualization, Methodology, Formal analysis, Writing (Preparation of the original draft), Writing (Revision and edition), Revision and presentation.
COH: Software, Data validation, Formal analysis, Data management, Writing (Preparation of the original draft), Writing (Revision and editing).
Funding
The authors declare that there were no external sources of funding.
Declaration of conflicts of interest
The authors have completed the ICMJE conflict of interest declaration form, and declare that they have not received funding for the production of the report; have no financial relations with organizations that might have an interest in the published article in the last three years; and have no other relations or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.Referencias

