Epistemonikos summaries
← vista completaPublished on April 24, 2015 | http://doi.org/10.5867/medwave.2015.03.6125
Is antibiotic prophylaxis beneficial in acute pancreatitis? - First update
¿Es beneficiosa la profilaxis antibiótica en la pancreatitis aguda? - Primera actualización
Abstract
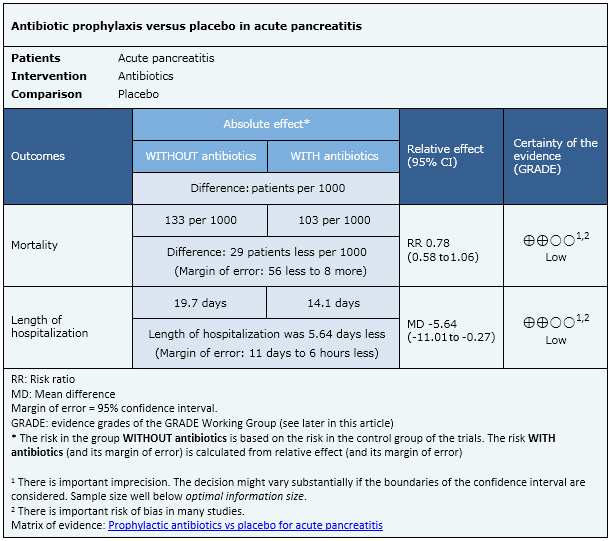
This Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) is an update of the summary published in August 2014, based on two systematic reviews appeared in January and February 2015. There is controversy about the effects of prophylactic antibiotics in acute pancreatitis. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified 18 systematic reviews including 19 randomised studies overall. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded that prophylactic antibiotics may reduce mortality and length of hospitalization in patients with acute pancreatitis, but the certainty of the evidence is low. The probability that future evidence change what we know is high.
About the update
The article updates the August 2014 Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) (doi: 10.5867/medwave.2014.07.6004) by including two new systematic reviews that appeared after publication of the original article [1],[2].
The new evidence incorporated in this summary does not lead to a modification on the certainty of the evidence, the key messages or other considerations for decision-making.
Notwithstanding, it is important to mention that our summary (consistent with the new reviews) is discordant with the results of the majority of previous systematic reviews and guidelines.
|
Key messages
|
Problem
Most cases of acute pancreatitis are mild but some patients develop a severe form of this condition characterized by organ dysfunction and/or local complications, such as pancreatic necrosis.
The initial stage is characterized by complications derived from the inflammatory systemic response, and in the second stage infectious complications might ensue with associated morbidity and mortality. Antibiotic prophylaxis has been proposed as an alternative to avoid the latter, but its use is controversial since it is also associated with adverse effects and antibiotic resistance.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
About the body of evidence for this question
|
What is the evidence.(See evidence matrix in Epistemonikos later).
|
We found 18 systematic reviews [1],[2],[3],[4],[5],[6],[7], |
| What types of patients were included. |
Most studies included patients with necrotizing pancreatitis [19],[29],[32],[35], severe pancreatitis [27],[33],[34],[38], any of these [24],[28],[31],[37], ], or severe necrotizing pancreatitis [22],[26],[30]. One study included patients with alcoholic pancreatitis plus two or more collections [21] and three old studies included patients based only on clinical and biochemical criteria [20],[23],[25]. |
|
What types of interventions were included. |
All studies except one [27] used intravenous antibiotics. Two studies used ampicillin [20],[23], one ampicillin or lincomycin [25], six imipenem [19],[28],[29],[30],[37],[38], two meropenem [22],[36], one ciprofloxacin [24] and three used a combination of ciprofloxacin and metronidazole [26],[34],[35]. Five studies allowed different antibiotic options [21],[22],[27],[31],[32]. |
|
What types of outcomes were measured. |
All studies measured mortality, but only three reported length of hospitalization. Other outcomes reported were pancreatic or peripancreatic infection, fungal infection, surgical intervention need, non-pancreatic infection, sepsis. |
Summary of findings
This information is based on 19 studies including 1178 patients. All studies evaluated mortality but only three (153 patients) measured length of hospitalization.
- Antibiotic prophylaxis may reduce mortality and length of hospitalization in patients with acute pancreatitis, but the certainty of the evidence is low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
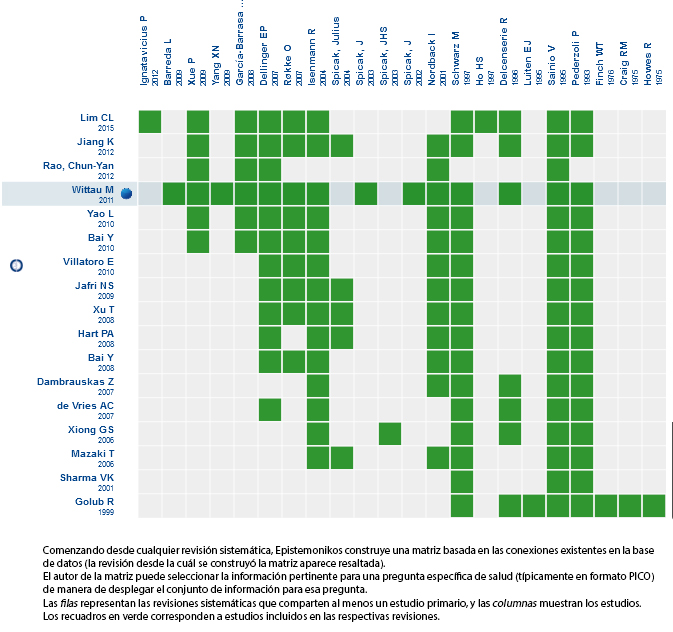 Full size
Full size Follow the link to access the interactive version Prophylactic antibiotics vs placebo for acute pancreatitis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here: http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Potential conflicts of interest
The authors do not have relevant interests to declare.

