Epistemonikos summaries
← vista completaPublished on June 27, 2015 | http://doi.org/10.5867/medwave.2015.6168
Is carvedilol better than other beta-blockers for heart failure?
¿Es el carvedilol superior a otros betabloqueadores en pacientes con insuficiencia cardiaca?
Abstract
There is wide consensus about the benefits of beta-blockers in systolic heart failure. However, it is not clear if one specific beta-blocker is superior to the others. Some guidelines favor three “evidence-based” beta-blockers (carvedilol, bisoprolol and metoprolol) that have proved to decrease mortality. Carvedilol might have different physiological properties, commonly referred as pleiotropic effects, but the clinical meaning of them is not clear.
Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified four systematic reviews including eight pertinent randomized controlled trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded there is little or no difference in hospitalization risk between carvedilol and bisoprolol or metoprolol, but carvedilol might decrease mortality compared to metoprolol or bisoprolol. It is uncertain whether nebivolol can be an alternative because the certainty of the evidence is very low.
Problem
Beta-blockers constitute standard treatment in heart failure with systolic dysfunction given their proven effect in morbidity and mortality. Some guidelines have recommended three “evidence-based beta-blockers” (carvedilol, bisoprolol and metoprolol) that have proved to decrease mortality in large trials. It has been postulated that carvedilol, a non-selective beta-blocker, would exhibit pleiotropic effects, such as increasing insulin-sensitivity, and vasodilator, antioxidant and antiarrhytmic effects, which might confer it superiority against the other beta-blockers. In the last years, nebivolol, a new beta-blocker with alleged pleiotropic effects has also been suggested as an option.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1-4] including 14 primary studies, reported in 15 articles [5-19], from which eight (reported in nine articles) correspond to randomized controlled trials pertinent to the question [5],[7],[9],[11-13],[15],[16],[19]. This table and the summary in general are based on the latter. |
|
What types of patients were included |
Average age between the studies ranged from 57 to 73 years. All studies considered heart failure of any etiology, except one [15] that restricted inclusion to ischemic heart failure. All studies except one [5] only included patients with low ejection fraction, defined as < 45% in one [7], < 40% in two [11],[12] and < 35% in four [9],[13],[15],[16],[19]. |
|
What types of interventions were included |
All studies evaluated carvedilol, compared to metoprolol in four studies [9],[13],[15],[16],[19], bisoprolol in two [5], [7] and nebivolol in two [11],[12]. |
|
What types of outcomes were measured |
All-Cause mortality, cardiovascular or sudden death, All-cause hospitalization, cardiovascular- or heart failure-cause hospitalization, non-fatal cardiovascular events, vital signs, quality of life, exercise tolerance, echocardiographic parameters, NYHA classification. |
Summary of findings
The information on the effects of carvedilol is based on eight randomized trials [5],[7],[9],[11],[12],[13],[15],[16],[19]. All of them reported total mortality, three reported All-cause hospitalization [7],[12],[16],[19] and only one reported heart failure-related hospitalization [11].
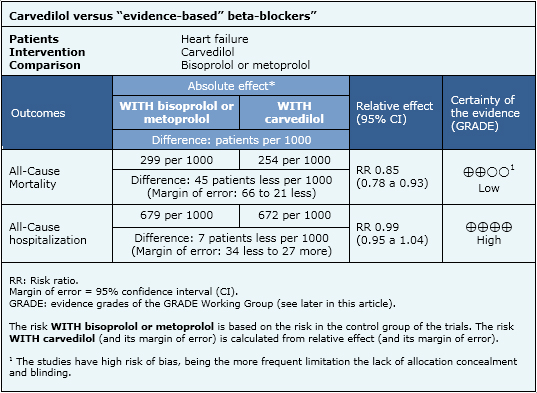
1) Carvedilol versus other “evidence-based” beta-blockers (bisoprolol, metoprolol)
Six studies evaluated this comparison, including 4333 patients [5],[7],[9],[13],[15],[16],[19].
- There is little or no difference between carvedilol and bisoprolol or metoprolol in hospitalization risk. The certainty of the evidence is high.
- Carvedilol might decrease mortality compared to metoprolol or bisoprolol in patients with heart failure. The certainty of the evidence is low.
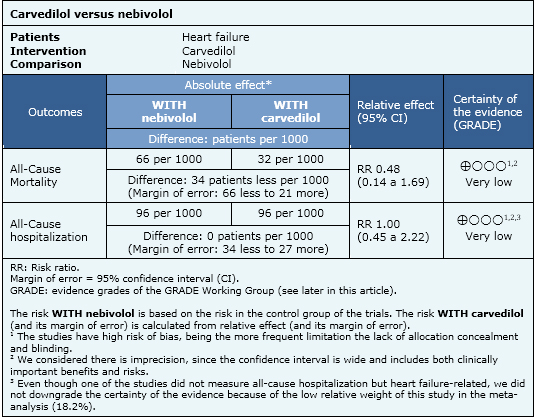
2) Carvedilol versus nebivolol
Two studies evaluated this comparison, including 191 patients [11],[12].
- It is uncertain whether nebivolol increases or decreases mortality in comparison to carvedilol. The certainty of the evidence is very low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
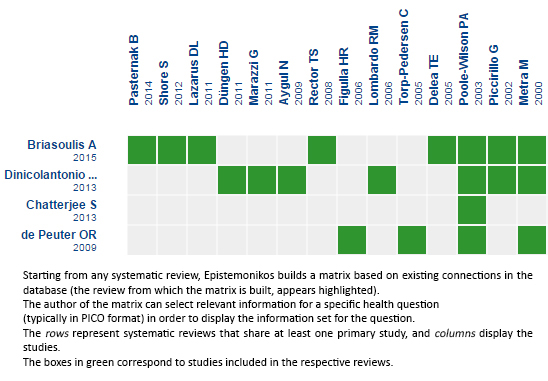 Full size
Full size Follow the link to access the interactive version Carvedilol versus cardioselective betablockers or nebivolol for heart failure

Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

