Epistemonikos summaries
← vista completaPublished on August 20, 2015 | http://doi.org/10.5867/medwave.2015.6224
High-dose inhaled corticosteroids or addition of theophylline in patients with poorly controlled asthma?
¿Uso de dosis altas de corticoides inhalados o adicionar teofilina en pacientes con asma no controlada?
Abstract
There are several management strategies for patients with poorly controlled asthma despite usual treatment. Increasing doses of inhaled corticosteroids or adding theophylline are among the therapeutic alternatives. However, the latter is associated with important adverse effects. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified only one systematic review including four pertinent randomized controlled trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded it is not clear whether theophylline or high-dose inhaled corticosteroids constitute a better alternative for symptomatic control or reduction in exacerbations in poorly controlled asthmatic patients because the certainty of the evidence is very low.
Problem
There are several management strategies for patients with poorly controlled asthma. Within the therapeutic alternatives are xanthines such as theophylline, or high-dose inhaled corticosteroids. Theophylline exerts its action on the bronchial smooth muscle relaxation, and through its anti-inflammatory and vasodilatory activity. Since theophylline is associated with important adverse effects, it is necessary to assess its potential benefits in symptomatic patients with initial therapy.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found one systematic review [1] including four randomised controlled trials [2],[3],[4],[5]. |
|
What types of patients were included |
All of the studies included patients older than 18 years who had symptomatic asthma. Two studies included patients with forced expiratory volume in 1 second (FEV1)> 50% [2],[4], one study with peak expiratory flow (PEF)> 50%, [3] and one study did not limit for lung function. Two of the studies specified there was no use of oral corticosteroids in the three weeks prior to intervention [2],[5]. The baseline therapy in all the studies was low-dose inhaled corticosteroids and short-acting inhaled beta agonists. |
|
What types of interventions were included |
All of the studies consisted of one arm receiving low-dose inhaled corticosteroids associated with theophylline and another arm receiving double dose of corticosteroids without theophylline. The dose of theophylline varied between 200 and 375 mg twice daily (depending on body weight). Two studies reported median plasma levels of theophylline (8.7 to 10.1) [2],[4]. High-dose of inhaled corticosteroids corresponded to twice the standard dose in all studies. In three studies the corticosteroid was beclomethasone (400-500 ug/day) [3],[4],[5] and in one study budesonide 400 ug/day [2]. |
|
What types of outcomes |
The systematic review meta-analyzed the following outcomes: change in morning PEF, change in evening PEF and predicted FEV1. Although symptomatic scores were reported in all studies, these results were not considered in the systematic review. Neither mortality, exacerbations nor hospitalizations were reported. |
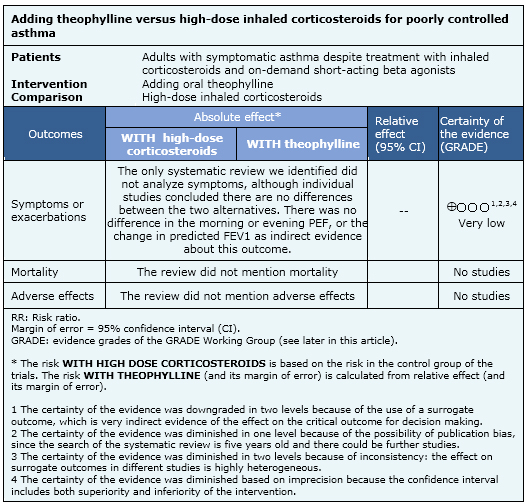
Summary of findings
The information on the effects of adding oral theophylline compared to the use of high-dose inhaled corticosteroids is based on four randomised controlled trials including 318 patients. All studies measured symptoms, and change in morning and evening PEF as outcomes. Three studies measured change in predicted FEV1 [1],[2],[4]. No study measured exacerbations, hospitalizations or mortality.
- It is not clear whether theophylline or high-dose inhaled corticosteroids achieve better symptomatic control or reduction of exacerbations in poorly controlled asthmatic patients because the certainty of the evidence is very low.
- No studies were found that evaluated the impact of theophylline compared with high-dose inhaled corticosteroids on mortality.
- The studies identified did not report adverse effects.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| Feasibility |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
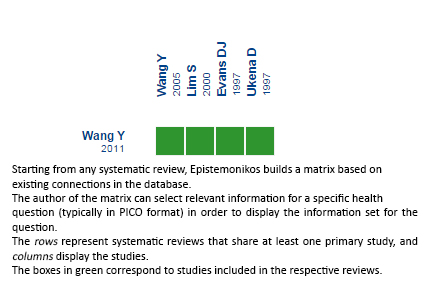 Full size
Full size Follow the link to access the interactive version: Increasing dose of inhaled corticosteroids or adding theophylline for unresponsive asthma
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

