Epistemonikos summaries
← vista completaPublished on February 23, 2017 | http://doi.org/10.5867/medwave.2017.6847
Should we add beta-blockers to band ligation for secondary prophylaxis of variceal bleeding?
¿Vale la pena agregar betabloqueadores a la ligadura endoscópica como profilaxis secundaria de hemorragia variceal en pacientes cirróticos?
Abstract
Cirrhotic patients who have had an episode of bleeding from gastroesophageal varices are at high risk of rebleeding, despite treatment with endoscopic variceal ligation. Adding beta-blockers could reduce this risk, but it is associated with adverse effects. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified seven systematic reviews including 21 randomized controlled trials addressing the question of this article. We extracted data, combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded the addition of beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal bleeding reduces the risk of rebleeding, but probably does not lead to any difference in terms of mortality. Even though it is associated to frequent adverse effects, these would be mild and generally do not lead to discontinuation of treatment.
Problem
Variceal bleeding in cirrhosis has a mortality risk between 20-50% per episode, as a consequence of hypovolemic shock or decompensation of underlying chronic liver damage [1]. Variceal rebleeding occurs in 60 to 70% of patients within the first two years after the first episode [2],[3],[4]. The standard strategy as secondary prophylaxis is eradication of varices with multiple sessions of endoscopic ligation. On the other hand, beta-blockers have proved to be better than placebo and randomized trials have shown there might be no difference in effectiveness when compared with endoscopic therapy [5],[6],[7],[8],[9],[10].
Endoscopic band ligation eradicates varices with high bleeding risk and beta-blockers reduce portal pressure, the main risk factor for variceal bleeding. However, it is not clear whether the combination of both therapies translates into a relevant clinical benefit when compared to endoscopic ligation alone.
Methods
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found seven [1],[2],[3],[4],[5],[11],[12] systematic reviews including three randomized controlled trials reported in four references addressing the question of interest [13], [14],[15],[16]. |
|
What types of patients were included |
All reviewed trials included patients who had already had a previous episode of variceal bleeding. |
|
What types of interventions were included |
The interval between ligation sessions was less than three weeks in two trials [14],[15]. One trial [16] did not report this data. |
|
What types of outcomes |
The main outcomes were overall mortality and rebleeding in all of the systematic reviews identified. Four reviews [1], [2],[3],[12] included adverse effects in their analysis, but none of them reported the data of adverse effects of the trials included in this summary. |
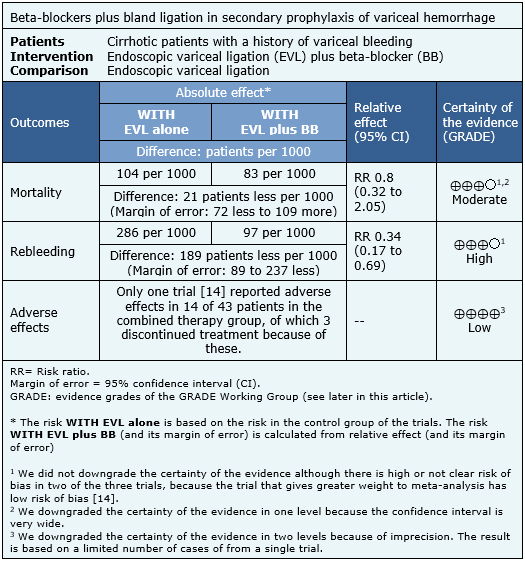
Summary of findings
The information on the effects of adding beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal bleeding is based on three randomized trials involving 161 patients [14],[15],[16]. All of the trials reported mortality and rebleeding and only one reported adverse effects [14]. The summary of findings is as follows:
- The addition of beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal hemorrhage leads to a substantial reduction in the risk of rebleeding. The certainty of the evidence is high.
- The addition of beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal hemorrhage might not reduce mortality, although the certainty of this evidence is low.
- The addition of beta-blockers would be associated to frequent but mild adverse effects, which generally do not lead to discontinuation of therapy, although the certainty of this evidence is low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
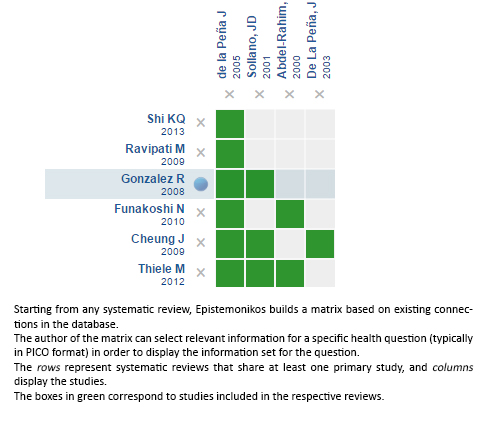
Follow the link to access the interactive version: Banding ligation versus beta-blockers for primary prevention of variceal bleeding
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

