Epistemonikos summaries
← vista completaPublished on March 29, 2017 | http://doi.org/10.5867/medwave.2017.6892
Should we administer oxygen during an acute coronary syndrome?
¿Debemos administrar oxígeno durante un síndrome coronario agudo?
Abstract
Oxygen therapy is used for the treatment of acute coronary syndrome without further discussion. However, the support of this practice in clinical research is scarce, ignoring the true effects of its implementation. To answer this question, we searched in Epistemonikos database, which is maintained by screening multiple information sources. We identified five systematic reviews including 12 studies overall, five of which were randomized trials. We extracted data, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded that using oxygen probably does not decrease pain, and might not make any difference in mortality during an acute coronary syndrome.
Problem
Oxygen therapy has a wide clinical use mainly in patients with cardiac and pulmonary disease. In this context, the use of oxygen in patients with an acute coronary syndrome is considered part of the usual treatment. This practice is supported by pathophysiology, as an increased arterial coronary oxygen concentration reduces myocardial hypoperfusion, the pain caused by this condition, and probably the associated morbimortality. However, other theories suggest that hyperoxia could lead to reduction in coronary flow and an increase in free radicals associated with oxygen, increasing the damage caused by the ischemia. However, the clinical effects of this intervention are not clear.
Methods
We used Epistemonikos database, which is maintained by screening multiple sources of information, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including 12 primary studies reported in 20 references [6], [7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18], [19],[20],[21],[22],[23],[24],[25]. Of these, five studies correspond to randomized controlled trials, reported in 13 references [11],[12],[13],[15],[16],[17],[18],[19],[20], [21],[23],[24],[25]. This table and the summary in general are based on the latter, since the observational studies did not increase the certainty of the existing evidence, nor did they provide relevant additional information. |
|
What types of patients were included |
Two trials included patients with confirmed acute myocardial infarction [23],[25] and three with suspected infarction [11],[12],[13]. Regarding the use of thrombolysis and angioplasty (PCI), two trials used PCI as first line therapy [11],[23]; another trial used PCI as first option in one of the centers while in the other thrombolysis was performed [12]; another trial mentions that it was conducted after the implementation of thrombolysis [25], but does not specify whether it was used as their primary intervention; one trial was conducted in pre-thrombolysis era [13]. The mean age was reported in three of the trials [11], [12],[13] ranging from 56 to 63 years. The same three trials report the average male proportion varied between 74% and 79%. The main reasons for exclusion reported by the trials were heart failure [13],[23],[25]; chronic obstructive pulmonary disease [12],[13]; other pulmonary conditions [13],[23], [25]; cyanosis [12],[25]; and complications of infarction [12],[23]. None of the five trials reported comorbidities of the patients included. |
|
What types of interventions were included |
All of the trials in this summary used facial oxygen mask for oxygen delivery as the intervention. Four of the trials used 100% oxygen [11],[12],[13],[25] but with different oxygen flow; two at 6 L/min [12],[13]; one at 8 L/min [11]; another at 4 L/min [25]. One trial used 45% oxygen with a flow between 3 and 6 L/min [23]. Three trials used ambient air as comparison [11],[23], [25]; one used oxygen to maintain arterial saturation between 93 and 96% [12]; another used oxygen at 21% with a 6 L/min flow [13]. The follow-up time considered by two of the trials [13], [25] was up to the patient's discharge. Another trial followed-up for 30 days [12], another for 10 days [23] and one trial for 6 months [11]. |
|
What types of outcomes |
Outcomes reported in the trials were grouped by the systematic reviews as follows:
|
Summary of findings
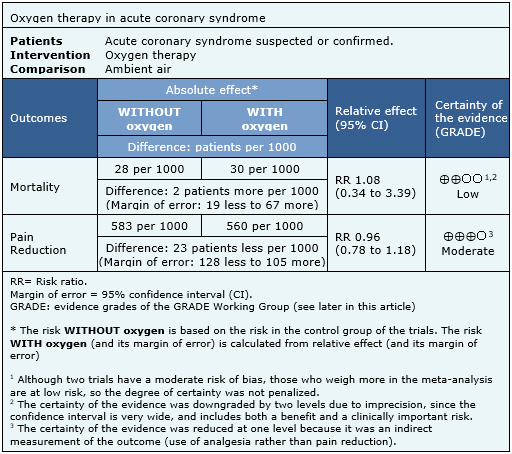
The information on the effects of oxygen on acute coronary syndrome is based on five randomized trials involving 1,123 patients. Four of the trials reported mortality [11],[12],[13],[23] and two trials (250 patients) reported pain estimated as analgesics requirement [13],[25]. The summary of findings is as follows:
- Oxygen therapy probably does not decrease pain during an acute coronary syndrome. The certainty of the evidence is moderate.
- Oxygen therapy might make no difference in mortality during an acute coronary syndrome. The certainty of the evidence is low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
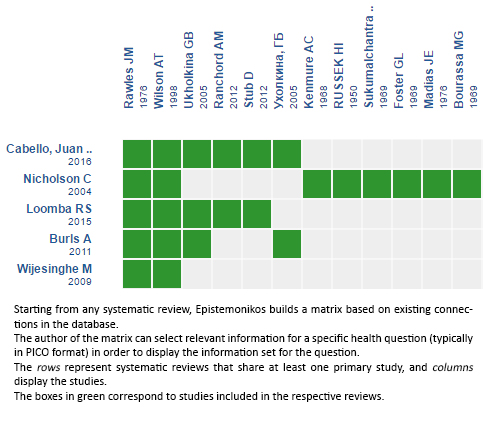
Follow the link to access the interactive version: Oxygen therapy for acute myocardial ischemia
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

