Epistemonikos summaries
← vista completaPublished on June 14, 2017 | http://doi.org/10.5867/medwave.2017.6972
Are cannabinoids an effective treatment for chronic non-cancer pain?
¿Son los cannabinoides un tratamiento efectivo para el dolor crónico no asociado a cáncer?
Abstract
The use of cannabinoids has been proposed as an analgesic for different painful conditions, especially for chronic pain refractory to usual treatment. However, its real efficacy and safety remains controversial. We sought to determine whether cannabinoids are an effective treatment for chronic non-cancer pain. To answer this question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We identified 37 systematic reviews including 41 studies overall, of which 32 were randomized trials relevant for the question of interest. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded it is not clear whether cannabinoids decrease pain in patients with chronic non-cancer pain because the certainty of available evidence is very low. On the other hand, they are associated with significant adverse effects.
Problem
Cannabis has been used for centuries for recreational and therapeutic purposes for various conditions, including pain. However, since the United Nations 1961 Single Convention on Narcotic Drugs, Cannabis has seen a worldwide ban and its use has been limited. Despite this, research on its therapeutic use led to the discovery of the endocannabinoid receptors CB1 and CB2, which through a mechanism associated with G protein would have an effect on pain reduction. Since many patients with different causes of chronic pain remain symptomatic despite standard therapy, it has been proposed that the use of Cannabis sativa plant extracts with its active ingredients delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), or its analogues, could be of use. Several studies have delved into this premise with different results and have revealed several associated adverse effects, ranging from gastrointestinal and neurological to psychiatric symptoms, with cannabinoids’ clinical utility still unproven. Given this scenario, we sought to determine whether cannabinoids constitute an effective treatment for chronic non-cancer pain.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found 37 systematic reviews reported in 38 references [1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14], |
|
What types of patients were included* |
Of the 32 trials comparing cannabinoids versus placebo, nine included patients with central neuropathic pain [43],[58],[76],[78],[79],[87],[108],[113],[115], nine included patients with multiple sclerosis [42],[54],[77],[93],[102],[104],[106],[119],[122], four included patients with diabetic neuropathy [61],[97],[103],[110], two included patients with HIV neuropathy [39],[56], two included patients with undifferentiated peripheral neuropathic pain [99],[114], one included patients with fibromyalgia [100], one included patients with musculoskeletal pain [90], one included patients with undifferentiated chronic non-cancer pain [85], one included patients with neurological pain of undifferentiated origin [86], one included patients with rheumatoid arthritis [46] and one included patients with pain associated with spasticity [117]. |
|
What types of interventions were included* |
Cannabinoids extracted from Cannabis sativa (THC, CBD and combinations) and synthetic cannabinoids (nabilone and ajulemic acid) were used as interventions via different routes of administration. Twelve used nabiximol (Sativex®, THC and CBD) in oromucosal spray [42],[43],[46],[61],[77],[79],[86],[87],[93],[97],[99],[106], six used oral nabilone [58],[90],[100],[103],[104],[117], five used smoked THC [39],[54],[56],[113],[115], three used dronabinol (oral THC) [85],[102],[119], three used oral THC combined with CBD [108],[119],[122], two used oromucosal THC spray [43],[110], one used oral ajulemic acid [76], one used oral CBD [78] and one used vaporized THC [114]. |
|
What types of outcomes |
The main outcome was significant pain reduction (≥ 30%) assessed on visual-analogue scale, 11 points numerical scale or neuropathic pain scale. Other outcomes evaluated were pain reduction ≥ 50%, quality of life and presence of gastrointestinal, central nervous system and psychiatric adverse effects, among others. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
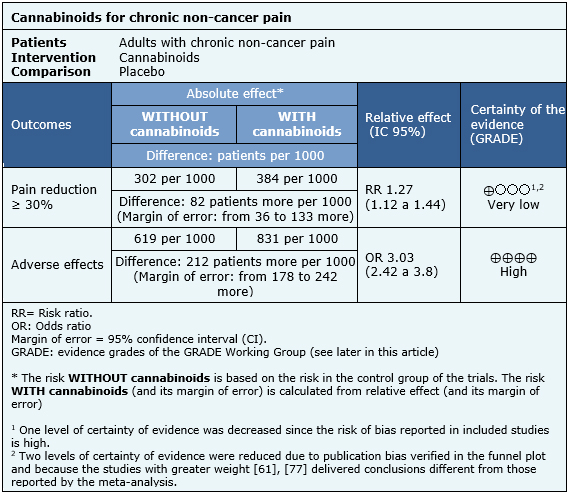
Summary of findings
Information on the effects of cannabinoids for pain reduction ≥ 30% is based on 15 randomized trials involving 1,788 patients [39],[43],[56],[76],[77],[79],[86],[87],[93],[97],[99],[101],[113],[114],[115]. The other trials did not report any outcome of interest, or did not present the information in a way it could be incorporated in a meta-analysis. Information on adverse effects is based on a systematic review [37] assessing the adverse effects of cannabinoids in different populations, and includes 3,489 patients in 29 trials reporting this outcome. The summary of findings is as follows:
- It is not clear whether cannabinoids decrease pain in patients with chronic non-cancer pain because the certainty of available evidence is very low.
- The use of cannabinoids is associated with a high rate of adverse events. The certainty of the evidence is high.
|
Follow the link to access the interactive version of the Summary of Findings (iSoF) table |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
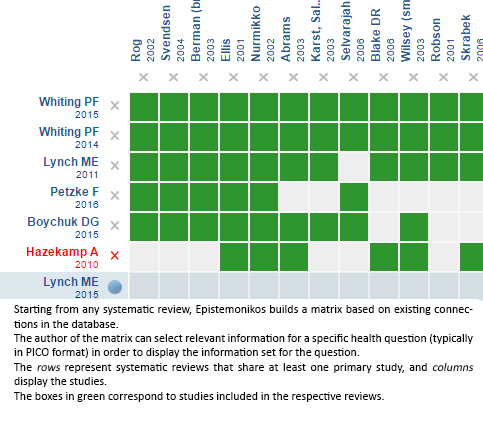
Follow the link to access the interactive version: Cannabinoids for chronic non-cancer pain
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrices and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

