Epistemonikos summaries
← vista completaPublished on October 18, 2017 | http://doi.org/10.5867/medwave.2017.08.7063
Is duloxetine an alternative in the treatment of osteoarthritis?
¿Es la duloxetina una alternativa en el tratamiento de la artrosis?
Abstract
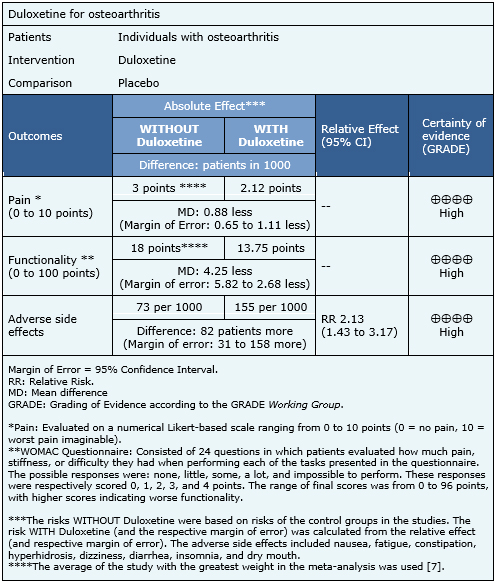
INTRODUCTION: Many osteoarthritis patients continue to present symptoms despite nonsurgical treatment. Duloxetine might be a viable alternative for such cases, but real clinical relevance remains unclear. METHODS: A literature review was conducted in Epistemonikos, the largest database for systematic reviews in health that compiles multiple sources, including MEDLINE, EMBASE, and Cochrane, among others. Relevant data were extracted, and information from the primary studies was reanalyzed. A subsequent meta-analysis was conducted, and summary of findings tables were constructed using the GRADE methodology. RESULTS AND CONCLUSIONS: Four systematic reviews including four randomized trials, were identified. In conclusion, while duloxetine slightly improves pain and functionality in osteoarthritis patients, its use is associated with frequent adverse side effects. Therefore, the benefit/risk balance appears unfavorable.
Problem
Osteoarthritis is a highly prevalent disease worldwide and a frequent cause for visits to both primary care and specialists. The persistence of pain despite nonsurgical treatment is one reason for such consults, and no clearly established alternatives exist for pain management.
Duloxetine has been used to treat various conditions with chronic pain, since it exerts central inhibitory effects, so it might be a therapeutic alternative for osteoarthritis with persistent pain after regular treatment. However, duloxetine is associated with adverse side effects, including fatigue, drowsiness, constipation, and high blood pressure.
Methods
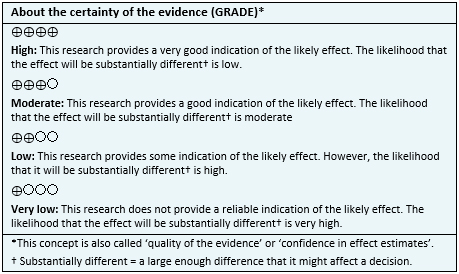
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] including four primary studies, reported in six references [5],[6],[7],[8],[9],[10]. All correspond to randomized controlled trials. |
|
What types of patients were included* |
Three trials focused on osteoarthritis of the knee [5],[6],[8] and one did not specify it [7]. Average WOMAC (The Western Ontario and McMaster Universities Osteoarthritis Index) ranged between 50 and 57 in three trials [5],[6],[8] and one did not report it [7]. Average age of the participants ranged between 61 and 69 years in the different trials. The proportion of women was between 16 and 77% in the different trials. |
|
What types of interventions were included* |
All of the trials used duloxetine in oral presentation. One trial used 60 mg/day as starting dose, which was increased to 120 mg/day at the seventh week in patients that reported a reduction in pain less than 30% [5]. One trial used 60 mg [6]. One trial used a flexible dosage between 60 and 120 mg per day, keeping a baseline treatment with NSAIDs at therapeutical dose [7]. One trial had two active arms, with 60 mg and 120 mg per day [8].** All trials allowed the use of concomitant analgesia. All trials compared against placebo. |
|
What types of outcomes |
The outcomes, as classified in the identified systematic reviews, were as follows: effect on the intensity of pain (analyzed as a decrease or improvement); overall impression of the patient-reported improvement; sub-scale of physical functionality established by the Western Ontario and McMaster Universities Arthritis Index (WOMAC); and adverse side effects. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
** This information was directly obtained from the primary studies.
Summary of Findings
The information on the effects of duloxetine was based on three randomized trials that included 1011 patients [5],[7],[8]. The remaining trials were not included in the meta-analysis as none of the identified systematic reviews extracted sufficient trial data. The three evaluated trials reported improvements in pain and functionality, and adverse side effects. The summary of findings is as follows:
- Duloxetine slightly decreases pain. The certainty of the evidence is high.
- Duloxetine slightly improves functionality in osteoarthritis. The certainty of the evidence is high.
- Duloxetine is associated with frequent side effects. The certainty of the evidence is high.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
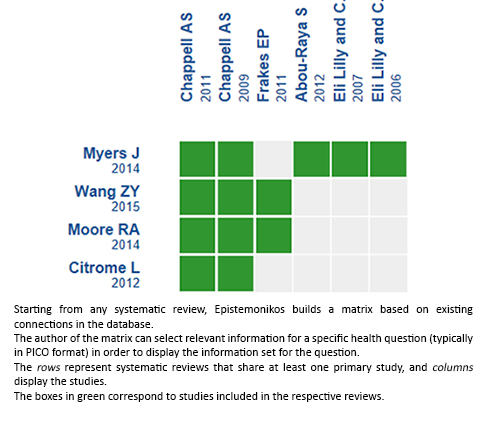
Follow the link to access the interactive version: Duloxetine for osteoarthritis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

