Epistemonikos summaries
← vista completaPublished on December 20, 2017 | http://doi.org/10.5867/medwave.2017.09.7101
Is secukinumab effective for psoriatic arthritis with insufficient response to initial treatment?
¿Es efectivo el secukinumab para la artritis psoriática que no responde a tratamiento inicial?
Abstract
INTRODUCTION Psoriatic arthritis is an inflammatory arthritis without a clear etiology. Biological therapy has become key for its treatment, especially in more severe cases. There are several alternatives for biological treatment, including secukinumab. However, it is not clear how effective and safe it is, which is particularly relevant considering its high cost.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified eight systematic reviews including three randomized trials overall. We concluded secukinumab in psoriatic arthritis leads to an improvement of disease activity and symptoms, and it is probably not associated to severe adverse events.
Problem
Psoriatic arthritis is an inflammatory arthritis without a clear etiology. It is associated with psoriasis, and the majority of patients are seronegative for rheumatoid factor. Currently, there are some alternatives for its treatment, mainly based on drugs proven for rheumatoid arthritis. In recent years, the efficacy of new alternatives for psoriatic arthritis has been studied in greater depth, especially for those who are resistant to initial treatment, either with non-steroidal anti-inflammatories, disease modifying drugs (e.g. methotrexate) or biological drugs (e.g. TNF-inhibitors). Due to its high cost, it is important to evaluate their real effectiveness to achieve a good outcome. Among these new alternatives is secukinumab, an IL-17a inhibitor.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found eight systematic reviews [1],[2],[3],[4],[5],[6],[7],[8], that include three primary studies, reported in five references [9],[10],[11],[12],[13]. All of them correspond to randomized controlled trials. |
|
What types of patients were included* |
All of the trials included adult patients with clinical psoriatic arthritis diagnosed according to CASPAR criteria, with active disease and inadequate response with non-steroidal anti-inflammatories, disease modifying drugs or anti-TNF biological medication. |
|
What types of interventions were included* |
One trial [10] included subcutaneous secukinumab 75 mg, 150 mg or 300 mg once a week for four weeks. Then, the same dosage was repeated every four weeks. |
|
What types of outcomes |
The outcomes were pooled by the different systematic reviews as follows:
|
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
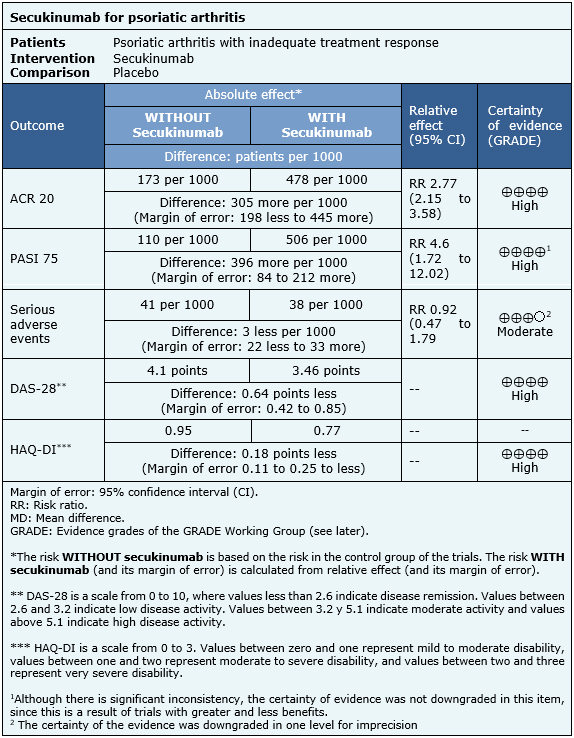
The information on the effects of secukinumab is based on three randomized trials that included 1045 patients overall [9],[10],[11]. All of these trials reported ACR 20, HAQ-DI and serious adverse events. Two trials reported PASI 75 and DAS-28. The summary of findings is the following:
- Secukinumab improves ACR 20 scale in psoriatic arthritis. The certainty of the evidence is high.
- Secukinumab improves PASI 75 scale in psoriatic arthritis. The certainty of the evidence is high.
- Secukinumab probably leads to little or no difference in serious adverse events against placebo in psoriatic arthritis. The certainty of the evidence is moderate.
- Secukinumab leads to an improvement of doubtful clinical relevance in DAS-28 scale in psoriatic arthritis. The certainty of the evidence is high.
- Secukinumab leads to an improvement of doubtful clinical relevance in HAQ-DI scale in psoriatic arthritis. The certainty of the evidence is high.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
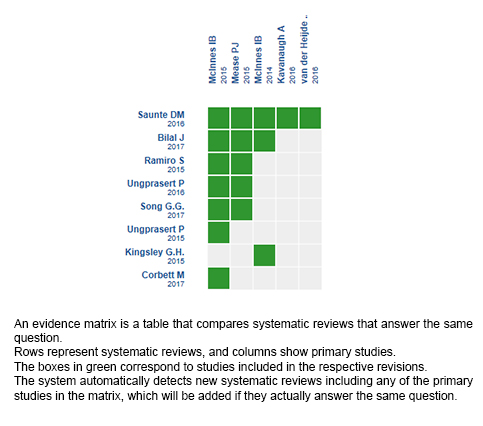
Follow the link to access the interactive version: Secukinumab for psoriatic arthritis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

