Epistemonikos summaries
← vista completaPublished on July 9, 2018 | http://doi.org/10.5867/medwave.2018.04.7160
Prophylactic mastectomy versus surveillance for the prevention of breast cancer in women's BRCA carriers
Mastectomía profiláctica versus vigilancia en la prevención de cáncer de mama en mujeres BRCA positivo
Abstract
INTRODUCTION Women who have mutations in BRCA genes have a high risk of developing breast cancer. Therefore, multiple preventive strategies have been proposed, within which is prophylactic mastectomy. Considering physical and psychological effects of surgery, the controversy is established as to whether the preventive effect exceeds that of active vigilance.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified 13 systematic reviews including 50 studies overall. We concluded prophylactic mastectomy is associated with frequent adverse effects, but probably reduces the incidence of breast cancer and decreases mortality, in addition to being associated with high levels of satisfaction.
Problem
Breast cancer has become a relevant public health problem, being one of the leading causes of cancer in women in some countries, and a leading cause of mortality. Mutations in BRCA1 and 2 genes are present in 1 of 300-500 people in the general population and confer 80% lifetime risk of developing breast cancer. Hereditary breast cancer is associated with mutations in the BRCA1 and BRCA2 genes in 40-50% of cases.
With the advancement of technology for genetic diagnosis, the detection of these genes has become more common, opening questions related to which interventions could reduce the incidence of this disease.
Several interventions have been considered, including active surveillance (periodic clinical examination plus imaging tests such as mammography, echotomography or magnetic resonance) and chemoprophylaxis. Prophylactic mastectomy has gained popularity in the last years, but there is a high level of controversy.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found 13 systematic reviews [1],[2],[3],[4],[5],[6],[7], |
|
What types of patients were included* |
The 32 studies [14],[15],[16],[17],[18],[19],[20],[21], |
|
What types of interventions were included* |
Only seven studies [14],[15],[16],[17],[18],[19],[20] compared prophylactic mastectomy versus surveillance. |
|
What types of outcomes |
The outcomes, according to how they were grouped in the identified systematic reviews, were: Incidence of breast cancer, mortality (any cause), physical impact after the intervention, satisfaction with the decision of prophylactic mastectomy, satisfaction with cosmetic results, psychosocial well-being, body image, sexuality, impact of mastectomy on relationship, incidence of other cancers, etc. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
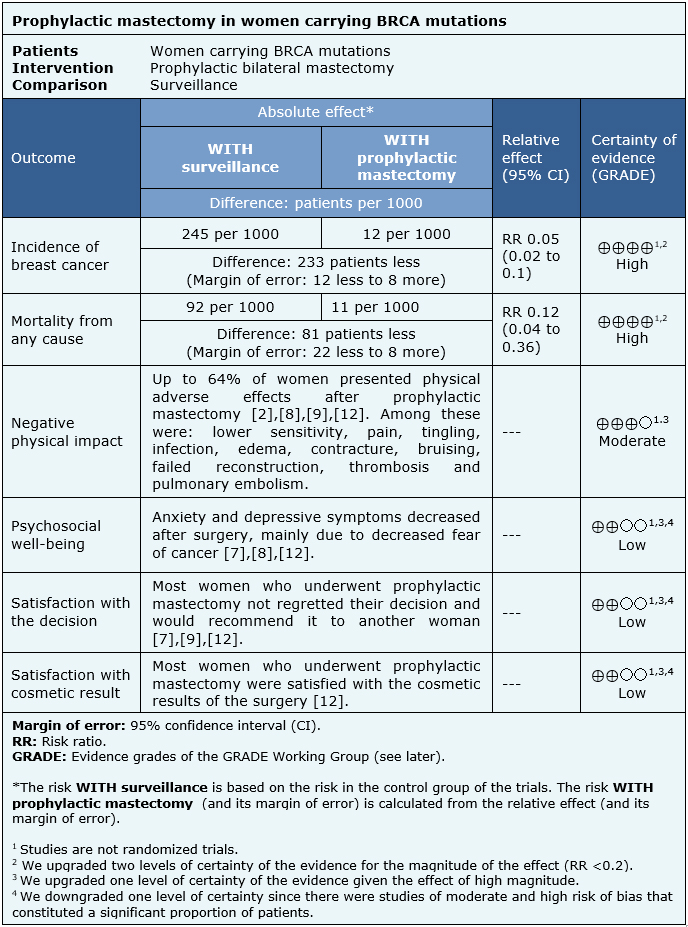
The information on the effects of prophylactic mastectomy compared to surveillance in women carrying a BRCA mutation is based on observational studies that included 6,328 patients [14],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45].
Only seven studies reported the incidence of breast cancer after prophylactic mastectomy or surveillance (2791 patients) [14],[15],[16],[17],[18],[19],[20]) and three studies measured mortality from any cause (1292 patients) [14],[18],[19]. Ten studies reported information on negative physical impact (2287 patients) [17],[21],[22],[23],[24],[25],[26],[27],[28],[29], 12 on satisfaction regarding the decision to have a prophylactic mastectomy (1464 patients) [23],[27],[28],[30],[31],[32],[33],[34],[35],[36],[37],[38], six on satisfaction regarding the cosmetic aspect of the surgery (1025 patients) [27],[30],[31],[33],[39],[40] and 13 on psychological well-being of patients undergoing prophylactic mastectomy (1307 patients) [23],[26],[29],[31],[32],[33],[34],[37],[41],[42],[43],[44],[45]). It was not possible to reanalyze the data from the primary studies on these last four outcomes, so the information was used as presented by the systematic reviews.
The summary of findings is the following:
- Prophylactic mastectomy prevents breast cancer in women carrying BRCA mutations. The certainty of the evidence is high.
- Prophylactic mastectomy decreases mortality in women carrying BRCA mutations. The certainty of the evidence is high.
- Prophylactic mastectomy probably has a negative physical impact in women carrying BRCA mutations. The certainty of the evidence is moderate.
- Prophylactic mastectomy might decrease depressive symptoms and anxiety in women carrying BRCA mutations, but the certainty of the evidence is low.
- Prophylactic mastectomy might be associated with a high level of satisfaction with the decision in women carrying BRCA mutations, but the certainty of the evidence is low.
- Prophylactic mastectomy might be associated with a high level of satisfaction with the cosmetic outcome in women carrying BRCA mutations, but the certainty of the evidence is low.
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
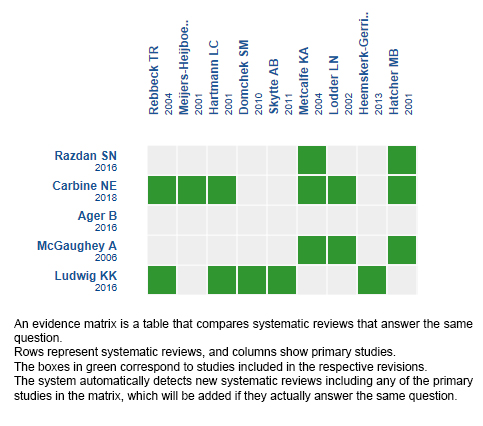
Follow the link to access the interactive version: Prophylactic mastectomy for the prevention of breast cancer in women who carry BRCA mutations
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

