Epistemonikos summaries
← vista completaPublished on September 12, 2018 | http://doi.org/10.5867/medwave.2018.05.7241
Is treatment with stem cells effective in Parkinson's disease?
¿Es efectivo el tratamiento con células madre en la enfermedad de Parkinson?
Abstract
INTRODUCTION There are many patients with Parkinson's disease who have a limited response to conventional pharmacological treatment. The use of stem cells has been postulated as an alternative, although its effectiveness remains a matter of controversy.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified two systematic reviews including 21 studies overall, of which three were randomized trials. We concluded it is not clear whether stem cells have any effect on the symptoms of Parkinson's disease because the certainty of the available evidence is very low.
Problem
Parkinson’s disease is a progressive and degenerative condition characterized by the destruction of dopaminergic neurons located in the substantia nigra, specifically in the nigrostriatal pathway, which leads to a progressive decrease in dopamine levels. As the disease advances there is also a loss in other neuronal groups (e.g. serotonergic, noradrenergic), which leads to a decrease in the number of functional dopaminergic and non-dopaminergic neurons, and the subsequent loss in the capacity to respond to treatment [1].
Despite improvements in pharmacological treatment which makes possible to control symptoms in a large proportion of patients, many patients remain symptomatic, or experience treatment-related complications, such as dyskinesias, akinesia and end-of-dose wearing off. In addition, Parkinson’s disease also leads to non-motor manifestations such as cognitive impairment, which limits the therapeutic alternatives [2].
Consequently, new alternatives are actively investigated, such as the implantation of stem cells. Stem cells are precursor cells with the ability to self-renew and generate multiple mature cell types. Embryonic stem cells result from the isolation and culture of blastocyst cells, which are formed 5 days after fertilization, and are pluripotent, which means they can grow into any type of adult cellular lineage. Adult or somatic stem cells remain quiescent with limited self-renewal and differentiation capacity. Numerous types of precursor cells have been isolated from adult tissues, leading to the concept that all tissues have their own compartment of stem cells, responsible for replenishing cells that die within human organs. Mesenchymal cells, for instance, are stromal in origin and can be isolated virtually from any tissue in the body. The most obvious therapeutic potential of adult stem cells is to restore or replace tissues that have been damaged by disease or injury and to avoid the ethical problem of using embryonic derived cells. However, the actual efficacy of stem cells derived from non-hematological tissue remains a matter of debate [3].
Stem cell transplantation is a novel alternative in Parkinson’s disease. Through implantation in the affected regions, it seeks to develop new synapses and restore the levels of dopamine in the nigrostriatal pathway. This technique requires stereotactic neurosurgery to graft them directly into required areas, which is not exempt of risks, generating controversy about the role of this intervention in Parkinson’s disease.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found two systematic reviews [1], [4], including 21 primary studies [5],[6],[7],[8],[9],[10],[11],[12],[13], |
|
What types of patients were included* |
Both trials included participants with Parkinson's disease with at least two of the following symptoms: bradykinesia, rigidity, tremor at rest and stability in their medication.The age range was 34 to 75 years. One trial included patients with Parkinson's disease for more than 7 years (average duration of 14 years) [5], while the other trial included patients with advanced Parkinson's disease, but did not mention the duration of the disease [7]. Both trials excluded patients with previous neurosurgery or a history of psychiatric illness. |
|
What types of interventions were included* |
All trials compared grafting of mesencephalic tissue cells of embryonic origin by stereotactic surgery. No trial reported the dose of levodopa that was administered if necessary. |
|
What types of outcomes |
All trials evaluated:
One trial [5] reported outcomes at the first year after surgery, while the second [7] reported them at two years after the procedure. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
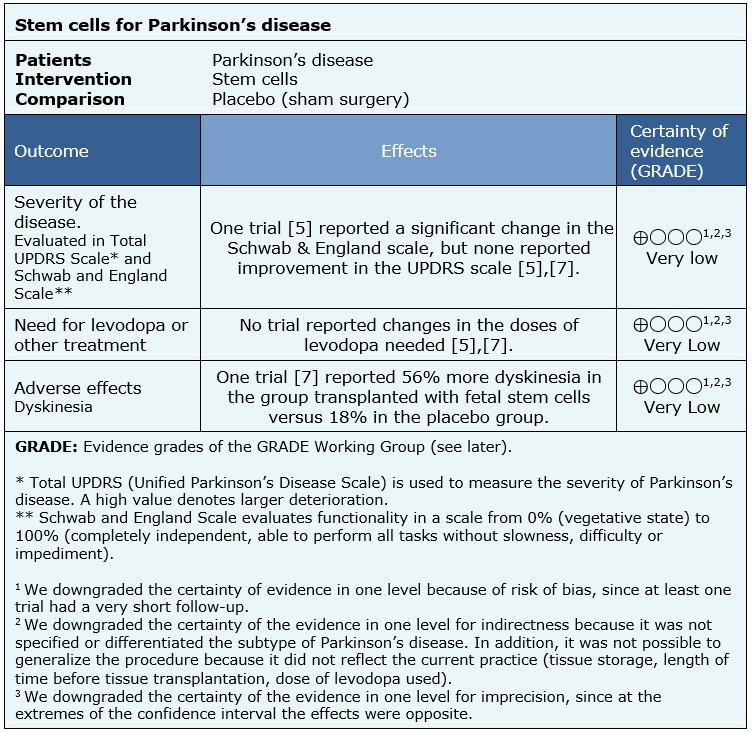
Summary of Findings
The information about the effects of stem cells for patients with Parkinson’s disease is based on two randomized trials [5],[7], including 74 participants.
None of the systematic reviews presented a meta-analysis, or information that allows to reanalyse the trials, so the information presented below corresponds to a narrative synthesis of the information as reported by the reviews.
The summary of findings is as follows:
- It is not clear whether stem cells have any effect on the symptoms of Parkinson's disease because the certainty of the evidence is very low.
- It is not clear whether stem cells reduce the need for levodopa or other treatments because the certainty of the evidence is very low.
- It is not clear whether stem cells have adverse effects because the certainty of the evidence is very low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
| Feasibility |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
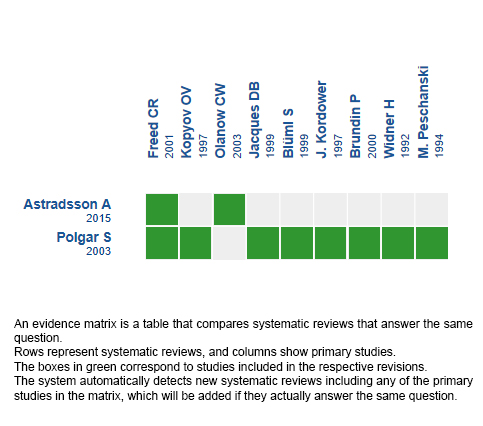
Follow the link to access the interactive version: Stem cells for Parkinson’s disease
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

