Analysis
← vista completaPublished on January 3, 2024 | http://doi.org/10.5867/medwave.2024.01.2762
Healthcare payment mechanism: Execution results of bundled payment program for bariatric surgery diagnosis in its first year of implementation in Chile
Mecanismos de pago en salud: resultados de ejecución del pago asociado a diagnóstico en cirugía bariátrica en su primer año de implementación en Chile
Abstract
Introduction More than 600 thousand people in Chile live with morbid obesity. Effective, safe, cost-effective therapeutic interventions are critical for healthcare systems and insurance schemes. In 2022, two bundled payment codes for bariatric surgery (gastric bypass and gastric sleeve) were incorporated into the National Health Fund's free-choice modality fee scheme. The objective was to characterize the execution of this payment mechanism program associated with bariatric surgery diagnosis in its first year of implementation.More than six hundred thousand people in Chile are estimated to live with morbid obesity. Effective, safe, cost-effective therapeutic interventions are critical for health systems and insurance schemes. In 2022, FONASA incorporated two Bariatric Surgery codes into the Free Choice Modality: Gastric Bypass and Sleeve Gastrectomy. Our objective was to characterize the execution of the Bariatric Surgery Bundled Payment Program in its first year of implementation.
Methods Descriptive and observational study of the pragmatic approach of the national execution of the payment associated with diagnosis in bariatric surgery. We examined sociodemographic variables (sex, age brackets, and National Health Fund tranches) and characterization of surgeries by code broken down by public or private provider, period of issue, unit cost, co-payment, and medical loans between March and December 2022.
Results We recorded n = 13 118 surgeries (45.81% bypass versus 54.19% sleeve), of which n = 2424 (18.48%) used medical loans. A total of 85.01% (p = 0.01) of the procedures were in women, in people between 35 and 39 years of age (20.15%), and 45.12% in beneficiaries of tranche B. Private providers performed a total of 99.21% of the surgeries. Ten accounted for 50% of the activity (range n = 1200 to 426 surgeries per year; n = 4.8 to 1.7 surgeries per working day). Total program expenditure was $71 626 948 350 CLP, accounting for 5.04% of the total activity of the national Diagnosis Associated Payment Program.
Conclusions The implementation of this bariatric surgery voucher benefited more than 13 thousand people living with obesity, mostly women of productive ages and with purchasing capacity. As an equity strategy, regardless of the access route through the voucher, it will be important to safeguard the activity in the public network.
Main messages
- According to the National Health Survey in Chile, 34.4% of the population lives with obesity, and 600 thousand people have a nutritional diagnosis of morbid obesity.
- Incorporating effective and safe therapeutic interventions for obesity is critical for healthcare systems and insurance schemes.
- This work presents an overview of the first year of executing the bariatric surgery payment mechanism program.
- The limitations of this analysis are the impossibility of ensuring that the month of issuance of the voucher corresponds to the same month of the surgical intervention; the data do not allow differentiating the purchase of vouchers or granting of loans by contributors and charges, and it was not possible to map the recovery of loans through the open data site.
Introduction
According to the National Health Survey in Chile, 34.4% of the population lives with obesity, and 3.2% has a nutritional diagnosis of morbid obesity, that is, more than 600 thousand people [1]. A study of the economic burden of obesity in the country indicated that an average expenditure of 455 billion Chilean pesos is attributable to direct costs of obesity annually, half of which are related to negative effects on cardiovascular health. Furthermore, the effect of obesity on indirect costs would be in the order of 1.92% of the national Gross Domestic Product (GDP) by the year 2030 [2]. Despite the impact of obesity on GDP, only 0.34% would be devoted to allocating budgets for expenditure on obesity treatment. In contrast, 1.87% addresses its complications [2]. The incorporation of effective and safe therapeutic interventions for the treatment of this disease becomes critical for healthcare systems and insurance schemes.
A cost-benefit study of bariatric surgery in Chile concluded that 30% of the intervention cost is recovered due to savings in complications associated with obesity in private insurance, whereas, in public insurance, the National Health Fund, 23% of the cost would be recovered [3]. Several international studies support the economic value of these surgeries in populations with type 2 diabetes [4,5,6,7,8], non-alcoholic liver cirrhosis [9], sleep apnea, dyslipidemia, and hypertension [10], among others. Bariatric surgery is a cost-effective alternative [7,8,9,10,11] that adds quality-adjusted life years [4], and its results are robust compared to conventional medical management of obesity [5,6].
Since 2010, the Bariatric Surgery Program of the National Health Fund has been operating in the public network through the institutional care modality and previously financed through payment for valued benefits, in which more than three thousand patients were intervened up to 2018 (according to official reports 1E N°8829/2019). At the same time, in 2022, two payment codes associated with diagnosis for bariatric surgery were incorporated into the National Health Fund’s free-choice modality tariff. Payments associated with diagnosis correspond to a bundled payment mechanism based on baskets aimed at the comprehensive resolution of a health problem or condition [12,13]. Only contributors in tranches B, C, and D of the National Health Fund and their dependents are eligible to purchase this voucher.
Payments associated with diagnosis define the classic variables of payment mechanisms: payment basis, risks, and price. Payments associated with bariatric diagnosis define the payment basis as access to surgery and associated resources for its performance: hospitalization days, laboratory and imaging tests during the inpatient stay, medications and medical devices, physician fees, and even follow-up. Additionally, as a tool to control risks, for example, asymptotic costs, it regulates the clinical eligibility criteria. For this case, a body mass index over 40 with or without associated morbidity was defined, as well as combinations of body mass indexes with major (e.g., type-2 diabetes mellitus, arterial hypertension) or minor (e.g., fatty liver, hypothyroidism) comorbidities. Payments associated with a diagnosis for this surgery demand a psychological evaluation and that the patient is free of contraindications. Each payment associated with bariatric surgery diagnosis defined the prices, being for the gastric sleeve (code 2501059) $5 224 530 Chilean pesos with a co-payment of $2 612 270, and for the gastric bypass technique a price of $5 737 280 defined with a co-payment of $2 868 640.
Given the prevalence of obesity in Chile, particularly morbid obesity, and given the implementation of payments associated with diagnosis for bariatric surgery as an alternative for the treatment of obesity in its most critical state, the purpose of this article is to characterize the execution of the payment bundled program for bariatric surgery diagnosis in its first year of implementation.
Methods
Descriptive and observational study with a pragmatic approach. Based on transparency request N° AO004T0005455 Oficio Ordinario 1K N°920/2023, access to secondary sources of data from the National Health Fund database on the complete record of payment executions associated with diagnosis for the period 2022 was obtained. This information was obtained within the framework of information access provided by public insurance through the Law of Transparency of the Public Function and Access to Information of the State Administration (Law No. 20 285).
The requested variables were the following: sociodemographic characterization of beneficiaries who register the payment of a diagnosis-associated payment voucher according to sex, age group, and National Health Fund tranche (operationalized in tranches B, C, and D based on their income and family charges defined by public health insurance), number of surgeries according to diagnosis-associated payment code broken down by public or private provider, month of voucher issuance, unit contribution or expenditure of the National Health Fund and patient co-payment in Chilean pesos, and number of authorized National Health Fund medical loans. Specifically, the National Health Fund loans correspond to the right of contributors and their dependents to receive support for financing a medical program authorized in the free-choice modality to contribute 42.5% of the total value of the procedure. In the case of bariatric surgery, a maximum loan of 85% of the co-payment was determined. This loan then fixes a debt with public insurance that cannot exceed 10% of the monthly income of the contributor [14].
The data were received electronically, in editable Excel format, without sensitive, traceable, or personal patient data. Data were processed using Microsoft Excel. The aforementioned variables were analyzed descriptively using central tendency statistics and parametric statistical tests according to the nature of each variable at an α of 0.01 to determine statistical significance.
Results
A total of n = 13 118 bariatric surgeries were performed in providers enrolled for diagnosis-associated payment program within the free-choice modality. Between March and December 2022, n = 6009 (45.81%) gastric bypass bariatric surgeries and n = 7109 (54.19%) gastric sleeve bariatric surgeries were performed. The month with the lowest issuance of payment vouchers associated with diagnosis was March (n = 302), consistent with the introduction of the payment voucher associated with diagnosis for this surgery. On the other hand, the month with the highest emissions was November (n = 1789) (Figure 1).
Total PAD voucher issuance by type of bariatric surgery.
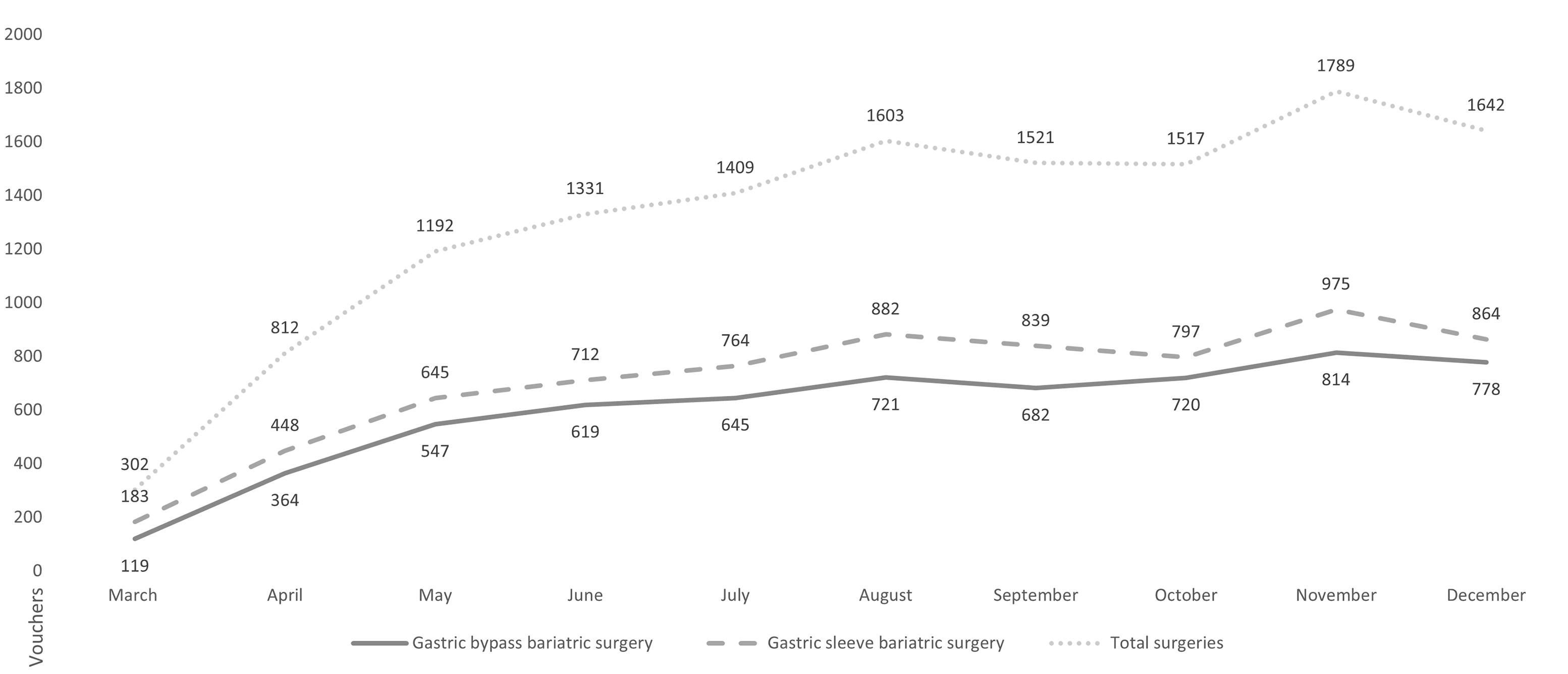
Source: Prepared by the authors based on Oficio Ordinario 1K N°920/2023.
The issuance of payment vouchers associated with diagnosis was more frequent in women than in men (Chi-square, p-value < 0.01), with a frequency of 85.01% versus 14.99%. The National Health Fund tranche with the highest issuance of diagnosis-associated payment vouchers for this surgery was tranche B with 45.12% (n = 5920), followed by tranche D with 37.07% (n = 4863), and in third place tranche C with 16.46% (n = 2159) of the activity. Some 1.35% (n = 178) of the emissions were registered in tranches A and X.
The procedures are mostly concentrated in people between 35 and 39 years of age (20.15%). In the case of gastric bypass, the highest concentration of procedures is observed between 25 and 29, up to the range of 45 to 49 years (81.49%). Meanwhile, gastric sleeve procedures are concentrated in people between 25 and 29, up to the range of 40 to 44 years of age (70.43%). People between 15 and 19 years old and those between 65 and 69 years old represent only 1.07% of the issued vouchers. Differences between the type of surgery by age group were statistically significant (p-value < 0.01). Additionally, in people between 15 and 39 years of age, gastric sleeve was more frequent (34.59%) versus gastric bypass (25.25%). However, the stat was inverted in people between 40 and 64 years of age, in whom gastric bypass was more frequent (20.40%) versus gastric sleeve (19.41%). These differences were significant (p-value < 0.01) (Figure 2).
Distribution of PAD voucher issuance by age group and type of bariatric surgery for the observation period.
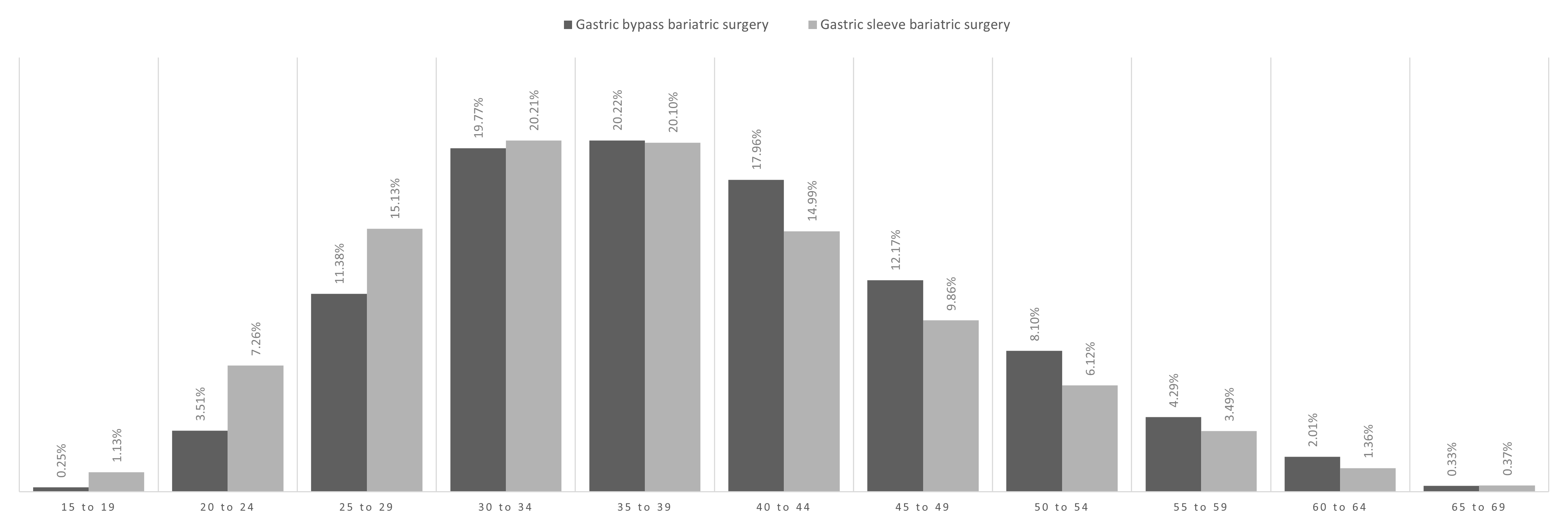
Source: Prepared by the authors based on Oficio Ordinario 1K N°920/2023.
A total of n = 13 014 (99.21%) surgeries were performed by private providers and n = 114 (0.79%) by public providers. Such differences in performance are statistically significant (Chi-square, p-value < 0.01). Fifty percent (n = 6559) of the total national activity in private providers was concentrated in ten facilities, performing a range of n = 426 (3.25%) and n = 1200 (9.15%) cases each per year, with gastric sleeve surgery (n = 3862) being the most frequent, accounting for 58.88% of the activity. Differences in performance of both surgeries when comparing total national providers versus reported activity at these ten providers were significant (Chi-square, p-value < 0.01). Within 251 working days in 2022, the highest-performing private provider performed an average of 4.8 surgeries daily. Within this group, the provider with the lowest number of daily surgeries performed 1.7 procedures. This subset of providers performed an average of 2.6 bariatric surgeries per day (Figure 3). The Metropolitan Region accounted for 48.33% (n = 29) of the providers that registered surgeries performed in 2022. In second place was the Valparaíso region, with 10.00% (n = 6) of the total number of providers, and in third place was the Los Lagos region with 6.67% (n = 4) of the facilities. Both the Bío-bío and Maule regions account for 5% (n = 3) of the providers performing surgeries. All the remaining regions have only one or two providers that have performed surgeries through payment associated with a diagnosis. Furthermore, 85.90% (n = 11 269) of patients who benefited from diagnosis-associated payment vouchers had access to the procedure in the Metropolitan region, while the Valparaíso region, despite having 10% of the national providers who performed these procedures, only attended 2.57% (n = 337) of the total demand under this modality. Finally, Los Lagos region managed 2.20% (n = 289) of the demand.
Annual PAD voucher issuance by the ten private providers with the highest issuance and estimated average number of bariatric surgeries per day.
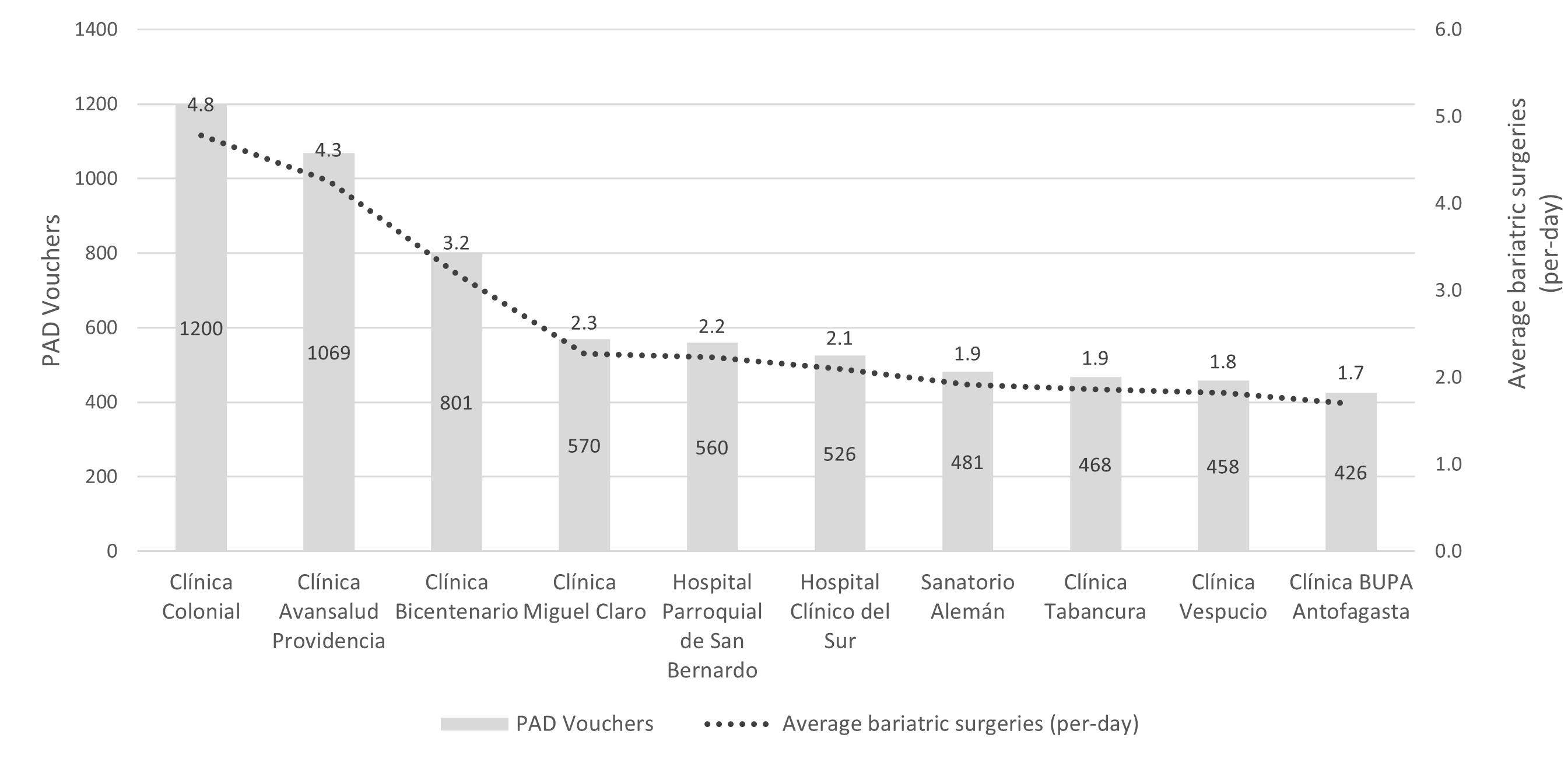
Source: Prepared by the authors based on data from Oficio Ordinario 1K N°920/2023.
The total expenditure observed for bariatric surgery in payment associated with diagnosis reached $71 626 948 350 Chilean pesos, distributed between the insurance contribution and patient expenditure. The insurance expenditure, i.e., the benefit bonus, is estimated at $35 813 438 620 for the entire bariatric surgery diagnosis-associated payment voucher program. On the other hand, the payment associated with the diagnosis of bariatric surgery with gastric sleeve issued by private providers accounted for an expenditure of $18 544 433 740 (51.78%), while gastric bypass surgery involved $16 973 742 880 (47.39% of the total). The insurance contribution for public providers was $263 914 880 (0.74%) for gastric bypass and $31 347 120 (0.09%) for gastric sleeve surgery. In parallel, patients made a total co-payment of $35 813 509 730 pesos.
A total of n = 2424 loans from the National Health Fund were granted for bariatric surgery, equivalent to 18.48% of the activity. This financing modality was mostly used by beneficiaries in tranche B (n = 955 loans; 39.40%) and D (n = 924 loans; 38.12%). The granting was more frequent in women than in men (89.19% versus 10.81%, respectively). Individuals between 30 and 39 years of age accounted for 45.54% of medical loans (n = 1104) for this diagnosis-associated payment.
In March, the proportion of loans to bonds issued was 1.99%. At the end of the period, 27.65% of the vouchers were issued with a medical loan. In other words, almost three out of ten surgeries required taking on debt to finance the co-payment (Figure 4).
Relationship between PAD bond issuance and granted FONASA medical loan.
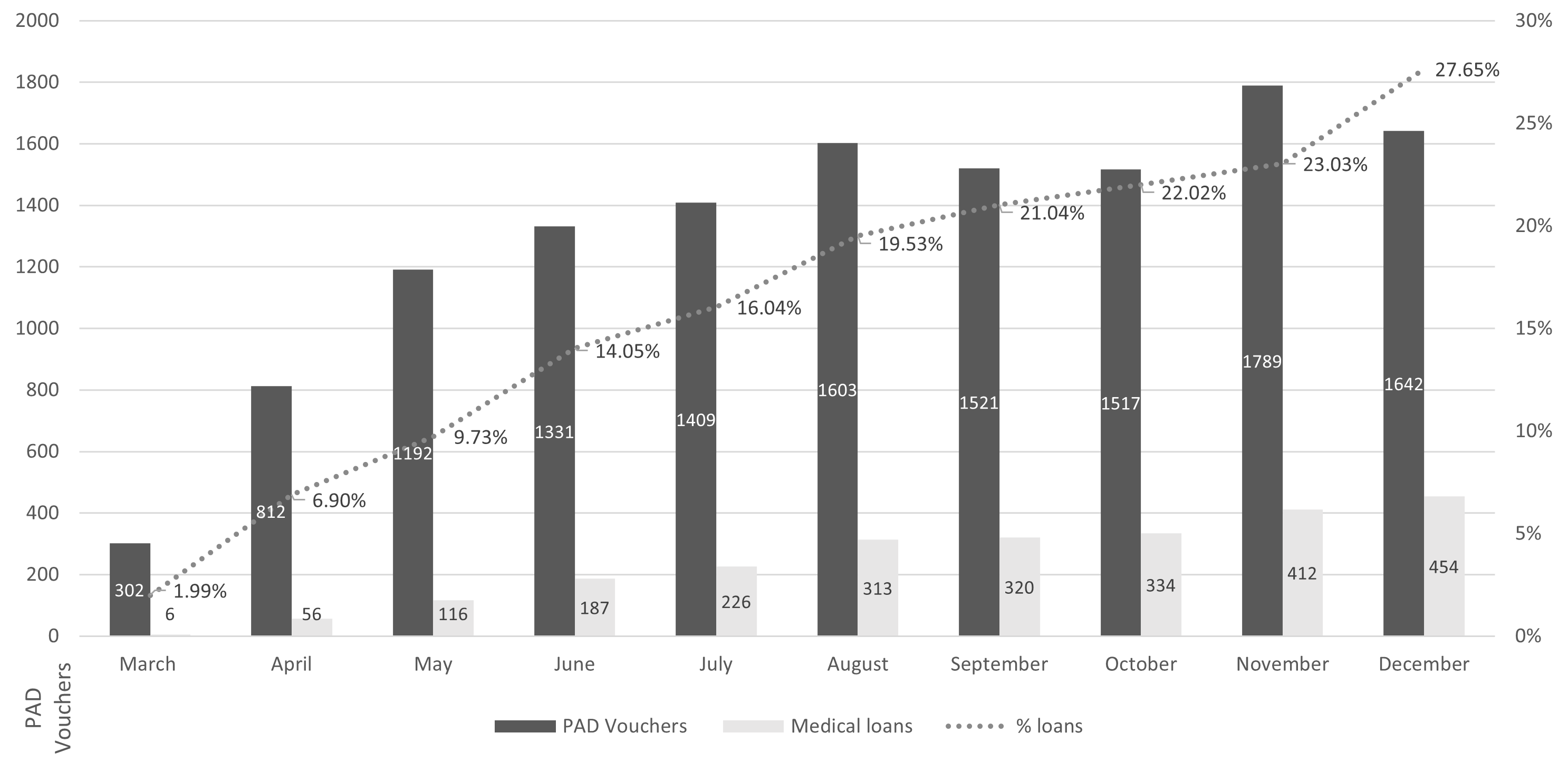
FONASA: National Health Fund.
Source: Prepared by the authors based on data from Oficio Ordinario 1K N°920/2023.
Discussion
The bundle payment program during the year 2022 registered a total of 262 thousand issued vouchers for the total number of resolutions included in the program. The main payment resolution associated with diagnosis was childbirth (code 2501009) with a total of n = 45 853 vouchers (17.46%), followed by cataracts (code 2501021) with n = 40 882 vouchers (15.56%) and cholelithiasis (code 2501001). Of the total payment activity associated with diagnosis, the issuance of vouchers for bariatric surgery accounted for 5.04%, ranking among the ten most issued payments associated with diagnosis, with gastric sleeve bariatric surgery in seventh place and gastric bypass in ninth place [15].
The number of diagnosis-associated payment vouchers issued for bariatric surgery during 2022 was similar to local projections that expected an annual total of n = 14 829 surgeries in tranche B, C, and D beneficiaries, based on current supply capacity and excess demand [16].
Productivity levels observed in the analyzed providers would be above the daily average in elective surgeries compared to those observed in the public sector. The latter presents a daily average of 3.3 surgeries for the entire portfolio (utilization rate of 53%, equivalent to 4.8 working hours out of a total of nine working hours [17]). The average private providers with the highest execution presented an average of 2.6 bariatric surgeries per day, reaching 4.8 surgical procedures.
The economic impact of incorporating the payment associated with the diagnosis of bariatric surgery was 5.09% of the total expenditure in the free-choice modality for 2022 (including payment activity associated with diagnosis, diagnostic tests, professional care, etc.). Comparatively, the expenditure of the bariatric surgery bundled payment program was lower than the insurance expenditure on bundled payment for diagnosis for childbirth ($42 058 909 110, i.e., 17.43% less expense). However, it was higher than all diagnosis-associated payments in the ranking of the ten most issued vouchers. That is, the expenditure on this new payment form in its first year of implementation exceeded the expenditure observed for cholelithiasis ($21 602 083 800, i.e., 1.7 times), cataracts ($19 569 072 220 or 1.8 times), photorefractive keratectomy or keratomileusis ($10 238 832 970 or 3.5 times), complicated abdominal hernia ($6 034 454 360 or 5.9 times), menisectomy ($6 016 876 110 or 6 times), phimosis ($1 458 401 200 or 24.6 times), and dental filling ($232 283 180 or 154.2 times).
The resulting local economic cost-benefit evaluation of the procedure showed a saving of 23%, considering weight regain and complications; this was in a scenario where the National Health Fund fully assumed the procedure costs and complications [3]. Such estimates could be improved given the financing system through the diagnosis-associated payment program. This is because the private provider assumes the cost of eventual complications, and the patient contributes with a 50% co-payment, reducing the cost for the public insurance by distributing the financial risk and costs, between the provider and the patient. This financing strategy would offset components of the expenditure in the free-choice modality and could improve the cost-benefit profile for the medium and long term. In fact, in an international evaluation of the economic impact of this surgery, at an investment between $17 000 and $26 000 US dollars (2008 currency), it was estimated that all costs were recovered within two years after surgery [18].
Bariatric surgery has shown benefits in mitigating patient comorbidities. It is necessary to obtain more in-depth estimates to relate the benefits of the intervention in the context of the diagnosis-associated payment program, in terms of savings in other programs such as Explicit Health Guarantees (coverage) Regime (GES) and Cardiovascular Health Program, among others. All of them address, in part, costs derived from obesity. In terms of magnitude, according to information provided by the open data site of the National Health Fund, it is indicated that the expenditure of the set of healthcare for cardiovascular diseases (disease codes I00 to I99) carried out in 65 hospitals financed through diagnosis-related groups, accounts for 12% of the total budget. This is equivalent to $205 492 million [19]. Incorporating techniques that reduce part of this expenditure and prevent the exacerbation of comorbidities will be strategic from a healthcare budget sustainability perspective.
A systematic review determined in more than 22 000 patients that bariatric surgery completely cured 76.8% of diabetes diagnoses and 61.7% of hypertension cases [20]. The International Federation for The Surgery of Obesity and Metabolic Disorders (IFSO) registry collected results for n = 68 374 gastric bypass procedures over seven years. In the case of type-2 diabetes mellitus, the prevalence dropped from 21.6% before surgery to 7.7% at 12 months after surgery. Hypertension experienced a drop from 33.5% to 19.6%, as well as musculoskeletal pain, going from 31.0% to 17.8%, and dyslipidemia, going from 27.5% to 13.8%. For the n = 47 334 records associated with gastric sleeve, the drop in type-2 diabetes mellitus went from 24.0% to 9.3%. In the case of hypertension, the prevalence dropped from 41.7% to 22.3%. In musculoskeletal pain and dyslipidemia, declines ranged from 26.3% to 15.7% and 27.2% to 14.6%, respectively [21]. A systematic review confirmed the benefits in people with diabetes, showing improvements of 0.9 to 1.43 points in the glycosylated hemoglobin marker compared to patients without surgery [22]. Likewise, another systematic review demonstrated an average drop of -88.2 milligrams per deciliter of blood glucose and -1.7% of glycosylated hemoglobin A1c after surgery [23]. Thus, bariatric surgery is positioned as a successful strategy in the management of cardiovascular risk factors of metabolic syndrome [24]. Similar benefits could be expected in the Explicit Health Guarantees programs for hip or knee replacement and in severe osteoarthritis diagnoses. Similarly, publications from the 2000s in Chile show reductions in comorbidities. Local data confirm the benefits in the reduction of insulin resistance, diabetes mellitus, and dyslipidemia in 100% of patients [25,26], the resolution of dyslipidemia in 92.5% of cases, arterial hypertension (63.6%), and osteoarticular problems (73.3%) [26]. Even in the Swedish population, over 16 years, the intervention reduced overall mortality with a favorable Hazard Ratio of 0.76 compared to the population that did not undergo surgery [27], which could expand an aspect of the analysis on the return on human capital.
From the point of view of insurance failure, the formulation of some payments associated with diagnosis has not controlled the practice of patient skimming by providers. In other words, the selection of less complex patients or those with a lower disease burden will optimize the reimbursement ratio versus the cost of care. In this context, there is room to deny the purchase of the voucher, for example, vouchers for payments associated with a childbirth diagnosis [28]. In contrast, the payment associated with bariatric surgery diagnosis controls this failure by explicitly incorporating comorbidity inclusion criteria, which precisely allows capturing the benefits associated with the reduction of comorbidities.
Although bariatric surgery began to be performed in Chilean public hospitals in 1986, it was not until the 2000s that the number of associated publications and patients who benefited from these studies increased [29]. By 2009, it was estimated that a total of n = 1500 surgeries were performed annually in Chile [30]. In the Bariatric Surgery Program of the National Health Fund between 2010 and 2018, n = 3011 surgeries were performed through payment for valued benefits (Oficio Ordinario 1E N°8829/2019). For example, the Salvador Hospital performed n = 256 procedures for that same period, and during the last year, n = 45. For its part, the Sótero del Río Hospital, between 2010 and 2018, performed a total of n = 200 procedures, and specifically during 2018, performed n = 61 procedures. Las Higueras Hospital performed a total of n = 83 between 2012 and 2018; in the latter year, a total of n = 13. On the contrary, simultaneously to introducing the diagnosis-associated payment voucher for this surgery in 2022, there was a decrease in the number of bariatric surgeries performed under institutional care modality in the public network. For example, the Salvador Hospital records only two of these surgeries associated with a main diagnosis of obesity in patients of the National Health Fund tranche C, and n = 66 discharges associated with tumors, sepsis, ulcers, acute abdomen, etc., which are presumably not indicated (Oficio Ordinario N°0159). The Sótero del Río Hospital performed a total of n = 38 surgeries under the institutional care modality with a main diagnosis of obesity, of which only five were beneficiaries of the National Health Fund, tranche A (Procedure AO081T0000943). In other words, patients who could not afford to purchase a diagnosis-associated voucher. Finally, Hospital Las Higueras reported zero cases of bariatric surgery performed during 2022 (Oficio Ordinario N°001306). The execution data of these providers could illustrate the fall of procedures in the public network financed through the institutional care modality. In sum, with the general decrease experienced by elective surgeries during the pandemic, it is presumed that the situation observed for public network bariatric interventions during 2022, along with the diagnosis-associated payment, would be similar to what was observed during the pandemic. Or even worse, given that this surgery is not prioritized in the regime of Explicit Health Guarantees and is added to waiting list.
The latter data may reflect the limitations in surgically prioritizing these procedures over other digestive surgeries, the pressure to recover surgeries on the waiting list that are part of the Explicit Guarantees Regime, which offset the surgical waiting list not included in this regime, or the migration of supply to the private sector. In other words, migration of surgical hours.
From this background, it is important to note that patients who are beneficiaries of tranche A of the National Health Fund are not eligible for the diagnosis-associated payment voucher. Likewise, it should be pointed out that the decreases in execution in the public network through the institutional care modality can potentially extend waiting lists for this surgery in this segment of beneficiaries. In addition to these local difficulties, the French experience has explored how social deprivation or extreme poverty can also become barriers to access, even though insurance systems guarantee full coverage of medical expenses [31]. This highlights the need to improve the communication of insurance and coverage models and the role of medical and administrative education in healthcare.
From a supply-side approach, the decline of bariatric surgeries in the public sector could account for incentives associated with the payment mechanism for the clinical segment. On the demand side, the displacement of procedures to the private sector could be in response to the desire to avoid the associated waiting lists, to a greater capacity of indebtedness, and to an elastic response to the co-payment of surgery in comparison with the previous alternatives to payment associated with diagnosis. Both, demand and supply, showed an elastic response to the studied diagnosis-associated payment.
From a service supply and geographic equity perspective, although all regions have at least one provider that performed bariatric surgeries through diagnosis-associated payment in the first year of implementation, the Metropolitan Region accounted for 85.90% of the procedures. Therefore, it will be important to review the geographic concentration of the available supply for bariatric surgery and the resolution capacity of each region. In Chile, the distribution of obesity is not homogeneous among regions. According to the last National Health Survey, in Aysén, the prevalence of obesity is 42.8%, in Bío-bío 35.5%, and in La Araucanía 34.9%; all above the national average of 31.4% [31]. Based on the data collected in this work, it was estimated that in Aysén, 0.02% (n = 2) of the total demand was met; in Bío-bío, 1.78% (n = 234), and in La Araucanía, 0.79% (n = 103) of the total number of national patients in 2022. Based on this background, we argue that it is valid to begin evaluating the region’s supply capacity of expansion.
A higher number of issued diagnosis-associated payment vouchers for women is to be expected, given the higher prevalence of this pathology among women; however, it was at higher rates than those reported by the National Health Survey. In the mentioned survey, the prevalence of obesity in women was 33.7% versus 28.6% in men, and 4.7% of morbid obesity among women and 1.7% in men [1]. In contrast, similar figures to those reported in this analysis were observed in the 10-year implementation of the National Health Fund Bariatric Surgery Program financed using payment for valued benefits, with 85.4% of women benefiting between 2010 and 2018 [32]. In the documented experience of more than 18 years of the Bariatric Surgery Program of the Pontificia Universidad Católica de Chile, the proportion of women who benefited from the program reached 79% [33]. The same trend is observed in international evidence of a decade of follow-up in the United States, where out of a total of more than 810 thousand surgical patients, 80.7% were women [34]. A similar proportion was reported in Brazil, with 85% of women [35].
According to data provided by the National Health Fund in the open data system, it is reported that in 2021 (the last year available and with complete information), a total of n = 11 949 medical loans were issued, totaling 14 billion Chilean pesos. The above is to finance institutional and elective activity, including emergency and elective treatments. Suppose we subtract the loans granted to finance emergency care and loans granted in the free-choice modality for the whole period. In that case, we record n = 2267 loans under the free-choice modality, including diagnosis-associated payments and payments unrelated to this system, equivalent to 1.7 billion Chilean pesos. In other words, in its first year of implementation, the loan activity of diagnosis-associated payments linked to bariatric surgery would have doubled the number of non-emergency free-choice loans. For this same type of activity (non-emergency free-choice), medical loans are also more frequent among beneficiaries in tranche B (56.27%) and tranche D (24.11%), although in bariatric surgery, the distribution of loans between tranche B and D was similar. Also, for the same type of activity, the same trend of a higher proportion of women accessing medical loans was observed. According to aggregate data from the National Health Fund, a total of n = 1288 women received loans in contrast to n = 802 men [36]. The differences in the proportion of women’s loans compared to men for the payment associated with bariatric surgery diagnosis versus national activity for the non-emergency free-choice modality activity set were statistically significant (Chi-square, p-value < 0.01). The association between gender, obesity, and low socioeconomic level could explain the greater use of medical loans by women. A Chilean study based on the last National Health Survey found that 82% of women with low socioeconomic status, in terms of income or education, were overweight; this association was not observed in men [37].
Access to bariatric surgery is complex and heterogeneous at the international level. In Canada, the number of facilities performing the surgery remained stagnant at 33 national centers between 2012 and 2019, even reporting that the surgery was available to only 0.58% of eligible adults [38]. In the United States, the restrictions of health insurance policy systems have been examined as a barrier to access, determining that 95% of insurers with the largest market share define pre-authorization policies [39]. It has also been analyzed that in the United States, payment mechanisms associated with insurance plans influence the performance of surgery [40]. Even in the NHS (National Health Service) of the United Kingdom, surgical indication biases that influence the distributive justice of the procedure have been studied [41]. In the Australian program in Canberra, geographical and psychosocial barriers that complicate adherence stand out [42]. Despite having a public funding program for surgery in Australia, interstate discordance is reported in determining surgical eligibility and guiding post-surgical care [43]. In Brazil, even though between 2010 and 2014, an increase of 60% in surgeries in public facilities was reported, there is geographic dispersion in terms of access, and there is still a high unsatisfied demand for this procedure since the providers do not meet the minimum number of surgeries required by the government, set at 96 per year. Some of the possible causes would be the high rate of open surgery instead of laparoscopy [35].
Among the limitations of this analysis is that it is impossible to ensure that the month of issuance of the voucher corresponds to the same month of the surgical intervention. On the other hand, the data did not allow us to differentiate the purchase of vouchers or granting loans according to contributors and charges. Nor was it possible to map loan recovery through the open data site.
Conclusions
Implementing the diagnosis-associated payment voucher for bariatric surgery benefited more than 13 000 people living with obesity in Chile, most of them women of productive age. The execution of this voucher went hand in hand with financial support instruments, such as medical loans from the National Health Fund, which more than one-fifth of the people used as an access tool.
As an equity strategy, regardless of the access to the diagnosis-associated payment voucher under the free-choice modality, it will be important to keep the Bariatric Surgery Program active under the public network for the institutional care modality since there are beneficiaries without debt capacity nor possibilities of purchasing a diagnosis-associated payment voucher, even though the diagnosis-associated payment voucher is a good tool. The latter occurs, for example, in tranche A of the National Health Fund, to which 19,61% of the beneficiaries belong, whose alternative is to remain on surgical waiting lists not included in the regime of Explicit Health Guarantees and subject to a historical de-prioritization of the procedure.
The diagnosis-associated payment voucher has been an excellent tool for improving access. However, in its first year of implementation, it only provided treatment to approximately 2% of the population living with morbid obesity. This surgery has demonstrated a good safety, effectiveness, and cost-effectiveness profile worldwide, with a good profile in the Chilean experience. This is mainly due to its effects in reducing the comorbidities that usually accompany morbid obesity.
Although the Chilean strategy has addressed several of the barriers and difficulties reported in the international evidence, there are still tasks to be undertaken to improve access and equity. For example, although several national centers are distributed among all regions and at least one provider in each region performs the procedures, supply concentrates in the capital. On the other hand, there is a low level of assisted demand in regions where the prevalence of obesity exceeds the national average. This opens a line of sectorial work to strengthen regional supply, recognizing that the distribution of obesity in Chile is heterogeneous.
The strategy of payment associated with diagnosis is useful. Still, not all beneficiaries of the National Health Fund can access the voucher, either because they cannot meet the co-payment, are not eligible for a medical loan, or belong to tranche A. This, in addition to the decrease in surgeries performed under the institutional care modality, shows that it will be necessary to prioritize bariatric surgery under this modality in the public sector. This is by virtue of its health outcomes and benefits for patients, as well as exploring new ways to ensure the sustainability of diagnosis-associated payment for bariatric surgery under free choice modality. This will enable the opening of a comprehensive portfolio to address obesity in Chile.

