Analysis
← vista completaPublished on April 7, 2021 | http://doi.org/10.5867/medwave.2021.03.8147
Description and analysis of primary care-based COVID-19 interventions in Colombia
Descripción y análisis de las intervenciones fundamentadas en la atención primaria para responder al COVID-19 en Colombia
Abstract
Introduction The COVID-19 pandemic was declared in early 2020, requiring different prevention and intervention measures on a large scale. In the case of Colombia, a series of measures focused on isolation and remote services provision were introduced in a context marked by health inequities. This article reviews the theoretical and normative references on primary care interventions in the Colombian response to the COVID-19 pandemic.
Methods A literature review was conducted in PubMed, LILACS, MEDLINE, and official documents and regulations issued in Colombia, the World Health Organization, and the Pan American Health Organization. A narrative synthesis was done of 33 documents based on their contribution to the implementation of primary care in Colombia and their role in the pandemic.
Results The information was organized into two categories: Actions taken in Colombia in response to COVID-19 and Opportunities in primary care in response to COVID-19. Colombia’s actions were contrasted with world experience. Better pandemic control was found in countries that adopted primary care as a response. Primary care has strengthened the handling of the pandemic through community action, the provision of coordinated services, mental health inclusion, and the adoption of telemedicine processes.
Conclusions In Colombia, primary care is presented as an opportunity to respond to the COVID-19 pandemic and the problems and needs derived from this situation. However, despite the above, there is resistance in the country to adopt this type of approach and complement the hospital-centric model to face the pandemic.
Main messages
- Colombia, in March 2020, declared a health emergency and adopted different governmental measures to respond to COVID-19.
- The measures adopted in Colombia focused on social isolation and strengthening the hospital system.
- The focus of primary health care was recognized worldwide as the strategy that allows essential health care within reach of individuals and families in the community through self-responsibility and self-determination.
- Colombia has led efforts to include this approach in its health system, but this situation requires a review of strategies from primary health care to respond to current and future threats.
- Two limitations of this work are the rapid evolution and change of the scientific literature regarding primary health care and COVID-19, which will restrict the applicability of its findings over time, and the scarcity of available literature on the COVID-19 pandemic, particularly for the Colombian case.
Introduction
In late 2019, a new coronavirus with pandemic potential was identified as the etiologic agent of a cluster of pneumonia cases in China and rapidly spread worldwide. In February 2020, it was identified as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), and the World Health Organization (WHO) designated the disease as COVID-19[1]. Cases increased exponentially until March 11, 2020, when it was declared a pandemic by the WHO and prompted the global adoption of prevention measures on a previously unprecedented scale[2].
In Colombia, a state of health emergency was declared by the Ministry of Health and Social Protection in March 2020[3], giving way to implementing different governmental measures through official documents to control the spread of the virus. Despite these efforts, new problems arise, such as the decrease in health care opportunities, mental health problems arising from confinement, and subsequent economic difficulties, aggravated by the country’s socioeconomic and health inequity[4],[5],[6].
On the other hand, in the world, the Primary Health Care (PHC) approach was recognized as a strategy that allows essential health care to be available to individuals and families in the community through self-responsibility and self-determination[7]. Colombia has made efforts to include this approach in its health system; however, this situation requires reviewing PHC strategies to respond to current and future threats[8].
This article seeks to review the available literature on intervention opportunities based on primary care to respond to COVID-19 in Colombia, comparing them with what is found in the available literature and official documents to generate a reference framework for applying PHC for the pandemic in the country.
Methodology
A narrative review was conducted to answer the question: what is the role of primary health care in the control of the COVID-19 pandemic in Colombia?
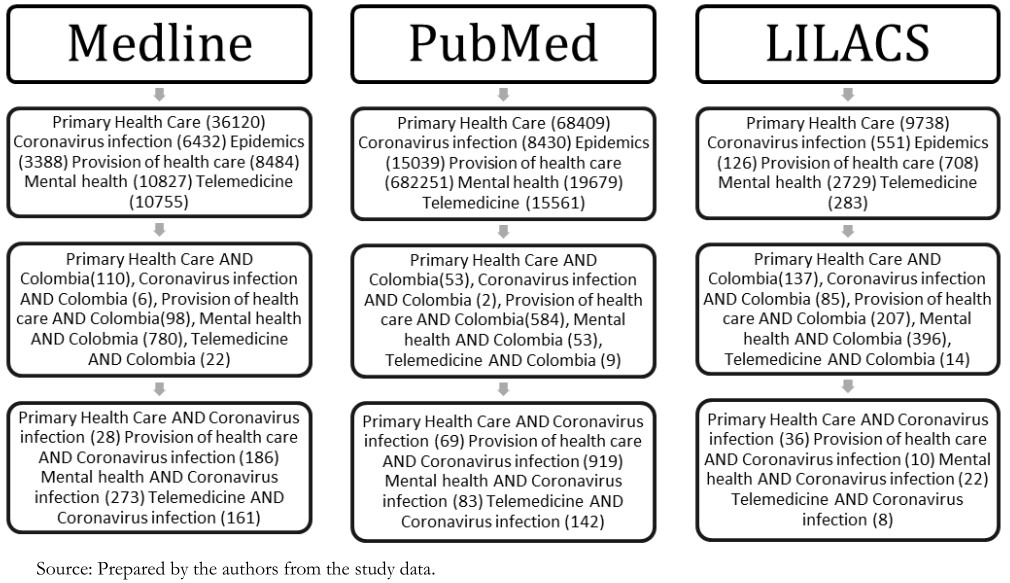
Using the DeCS/MeSH descriptors “Atención Primaria de Salud”, “Infecciones por Coronavirus”, “Epidemias” y “Prestación de servicios en salud” with their respective English terms, limited to the last 10 years, with a cut-off date of June 2020. The relevance of the terms “Mental Health” and “Telemedicine” was identified, so they were included in the search and associated with the terms “Colombia” and “Coronavirus Infections” to address the available literature in the Colombian context, as well as the relationships between PHC and these infections (Figure 1).
 Full size
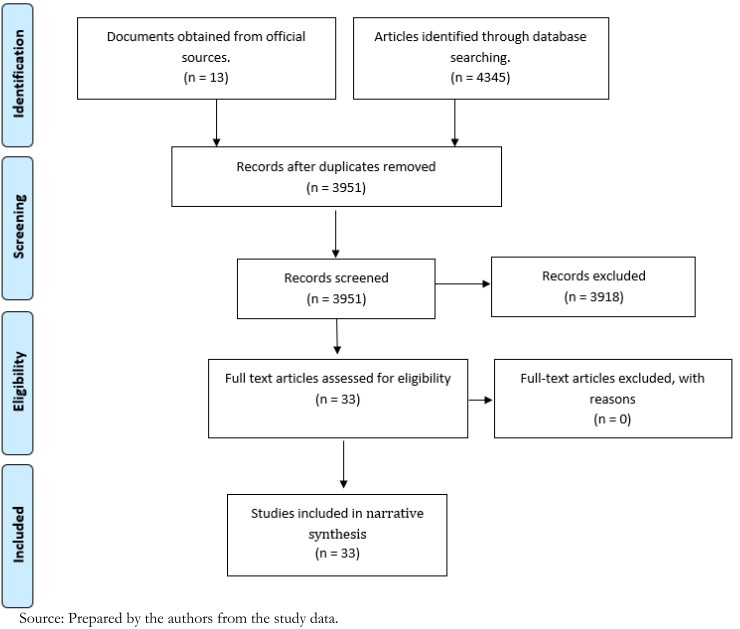
Full size Articles with full-text access, in Spanish and English, corresponding to research studies and reflection documents that include PHC elements and analyze their role in the pandemic were selected. Finally, official documents and regulations from Colombia, WHO, and the Pan American Health Organization (PAHO) were included (Figure 2).
 Full size
Full size Documents were then organized in a database with titles, abstracts, and dates of publication; subsequently, duplicates were eliminated, and the remaining documents were reviewed according to the previously mentioned criteria. A narrative synthesis was made of 33 documents according to their contribution to the implementation of primary health care in Colombia and their role in the pandemic, and the information was organized in the following categories: Actions taken in Colombia in the face of COVID-19 and Opportunities in PHC in the face of COVID-19.
Results
Actions are taken in Colombia in the face of COVID-19
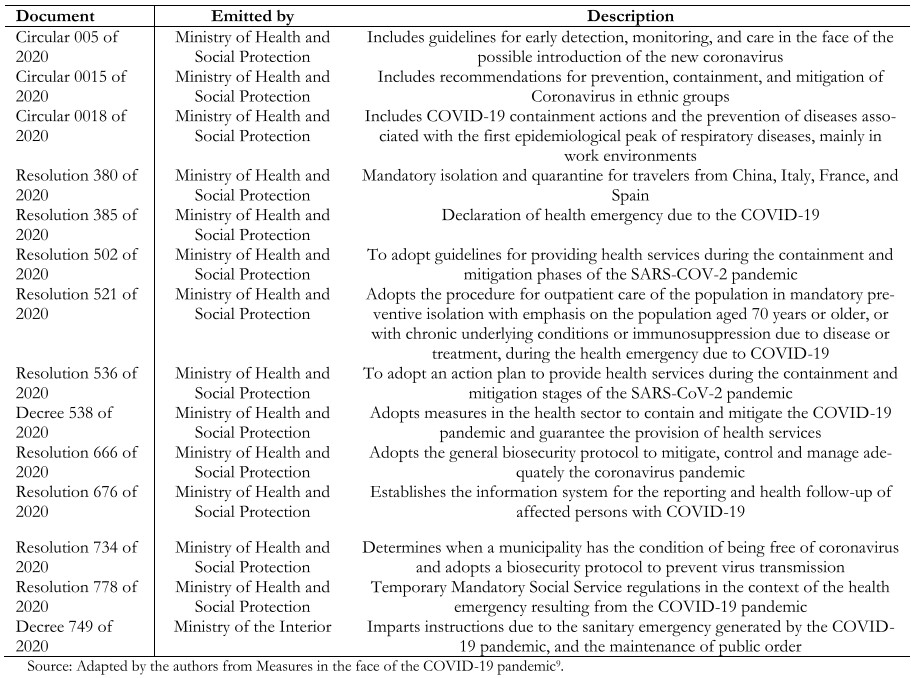
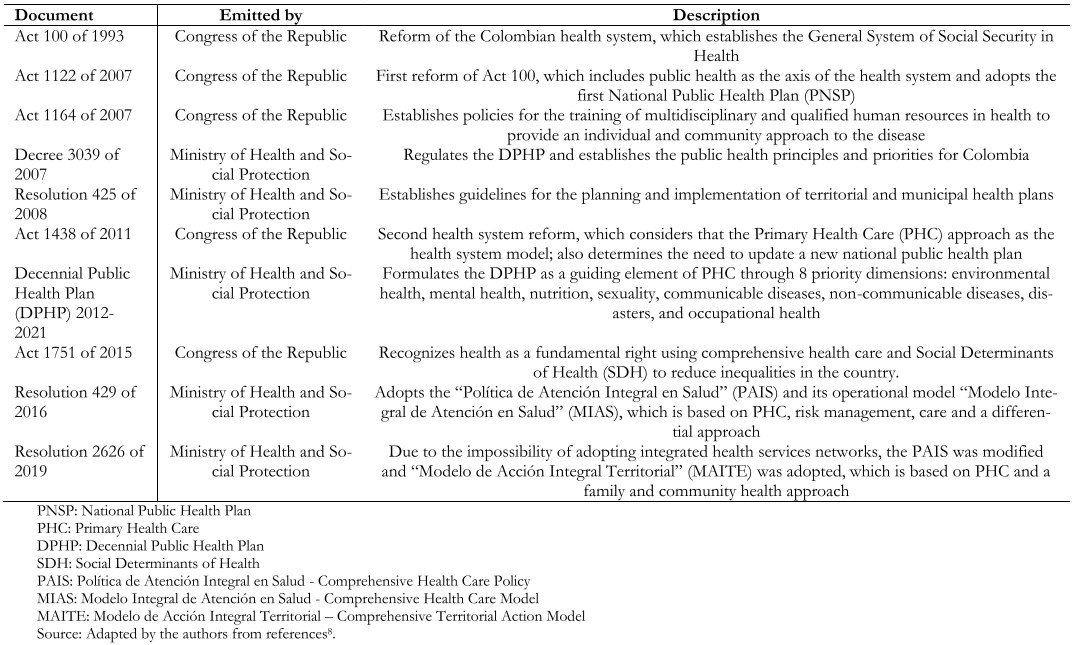
Colombia, like many countries, has integrated PHC strategies to improve the health conditions of the population, taking into account their social conditions[6]. However, regulations in response to COVID-19 have been limited to the formulation of resolutions classified as sanitary and sanitary emergency measures; social, economic, and ecological emergency measures; and public order measures, and others of an ordinary nature[9] (Table 1). These are not based on PHC strategies but include aspects of promotion and prevention.
 Full size
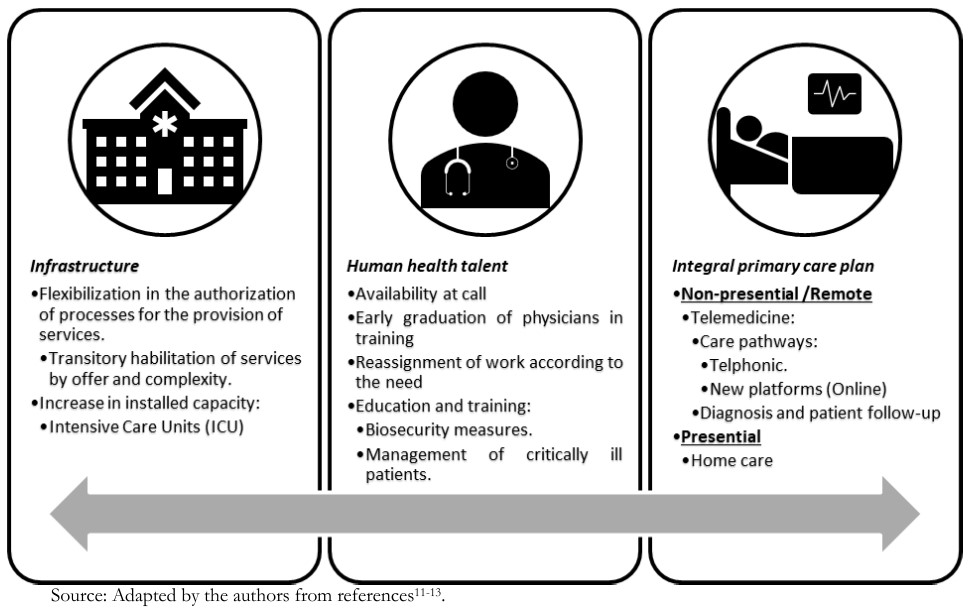
Full size Thus, the initial response included plans for early detection of the disease before the arrival of COVID-19[10]. After the declaration of the state of health emergency in Colombia, and one day after the WHO declared the pandemic, efforts were directed at preventing the spread of the virus and preparing health professionals and health care institutions for a possible increase in the demand for care[11]. In this regard, the regulations cover structural issues, human talent, and service provision (Figure 3), prioritizing three population groups in terms of home care:
a) people who make spontaneous demand for general morbidity (especially those over 70 years of age).
b) patients with controlled chronic pathology and low risk.
c) people with uncontrolled chronic pathology of medium or high risk and pregnant women[12].
 Full size
Full size Also, a notification system was implemented that details the information related to the health of the infected, integrating the reporting, care, and follow-up of patients; giving way to decision making based on the data collected by it in terms of speed of spread, identification of new and accumulated cases, follow-up, lethality, time of evolution of the epidemic, installed capacity of beds in Intensive Care Unit (ICU), laboratories and available human talent[13].
On the other hand, interventions vary worldwide, showing different outcomes ranging from the explosive growth of cases, as observed in Brazil, Chile, Peru, and Mexico[14],[15],[16]. In contrast, the flattening trend observed in China, Vietnam, Cuba, and Costa Rica is due to the implementation of PHC-based strategies that include the active search for cases and where governmental entities are responsible for institutionalized isolation, case follow-up, and epidemiological surveillance through the characterization of contacts by those infected in strategic locations[16],[17],[18]. Contrary to what occurs in Colombia, where PHC actions are not the central axis of the response to the pandemic[9].
Opportunities in Primary Health Care in the face of COVID-19
The pandemic represents an unprecedented crisis and tests the response of modern health systems[19]. Under the global scenario, PHC, as a transversal public health strategy, can respond to this situation through the integration of epidemiological surveillance, care processes, the Natural History of Disease (NHD), and clinical practice, which makes it possible to propose and classify preventive strategies at three levels: primary, secondary and tertiary, according to the moment at which they are applied. In this way, the importance of identifying the vulnerable population in the face of an entity from the Social Determinants in Health (SDH) and risk factors specific to individuals is highlighted to improve access, ensure continuity of services and promote self-care and solidarity of the community, unlike the hospital-centered model with a focus on disease and paternalism[20].
Therefore, there is an opportunity to reinforce key aspects of PHC and new strategies focused on primary prevention[21] that can be evidenced by community action policies for the care of the population, emphasizing self-care and empowerment in health. On the other hand, there is a need to renew the provision of health services, articulated with the implementation of telemedicine as an alternative to traditional means, and the search for solutions to mental health problems arising from the situation[22]. Besides, there is a need to improve the quality of health services, articulated with the implementation of telemedicine as an alternative to traditional means and the search for solutions to mental health problems arising from the situation[22].
1. Community actions
The characteristics of the microorganism give it a great capacity for contagion and, in the absence of vaccines and specific treatments, call for the need to employ public health strategies to reduce contact among the population and reduce the transmission of the disease. This is where measures such as hand washing, the use of masks, isolation, quarantine, and social distancing become important[23].
First, among the elements of promotion and prevention against the pandemic, hand washing and personal protective equipment (PPE) are included. The importance of these is that they are tools that are easily accessible to the entire population and involve them actively in the control of contagion, which stimulates solidarity to facilitate compliance with isolation measures[24].
At the same time, different authors agree that one of the main measures for pandemic control involves limiting the movement of people through quarantine, isolation, and social distancing[25]. In combination with cross-sectoral crowd control efforts, such as the closure of academic institutions, these measures have shown effectiveness in controlling the increase in COVID-19 cases and allow health systems to prepare for the increase in demand[25].
Also, PHC strategies explore the characteristics and needs of communities, including cultural safety, which is important given the unequal distribution of the pandemic with a predilection for vulnerable populations such as low-income communities and ethnic minorities. In this way, they allow the conjugation of traditional and current knowledge, achieving the articulation of the health system with these populations[26],[27].
Because of the above, the isolated use of community measures has a limited impact on disease control, while the combination of these measures has proven to be effective and has a high impact on the reduction of transmissibility, the collapse of health care services, and, consequently, mortality[25].
2. Provision of Health Services and Telemedicine
At the national level, certain conditions have been identified that hinder the provision of services. First, there is low availability of ICU beds[28]. Likewise, there is a decrease in the timeliness of outpatient care secondary to the measures adopted during the pandemic, which increases the risk of deterioration of chronic pathologies and loss of continuity and comprehensiveness of health services. Thus, there is a need to adapt intra- and extra-hospital services through non-face care, increasing the installed capacity and training health personnel[29],[30],[31].
Consequently, the provision of intrahospital services has focused on controlling the spread of the virus, so it is important to protect patients not infected by COVID-19 while ensuring care for those infected. This implies the adaptation of spaces for hospital wards and ICU functions, as well as the limitation of elective procedures to avoid situations such as the one in Italy, where the overflow of services resulted in the care provided in improvised spaces and a consequent increase in the risk of contagion[19],[32]. For this reason, territorial plans have been stipulated focused on the expansion of installed capacity that seeks to prepare Colombia in the event of not achieving adequate control of the pandemic[33].
Regarding outpatient services, given the isolation measures and to reduce infection rates, they were suspended, which made it difficult to follow up patients with chronic pathologies and those affected by COVID-19 without hospitalization criteria. In response to this, home visits have arisen to continue monitoring these patients, evaluating their environment and which in the future may be adopted for the care of non-urgent pathologies[34]. Likewise, home dispensing of medications and early delivery of up to three months of formulations to limit the movement of persons are also included[12].
Besides, a renewed interest is emerging worldwide in the use of digital platforms that allow remote care since they provide continuity to out-of-hospital services, allowing the control of the spread of the virus by limiting physical contact[31],[35]. Colombia has regulations on telemedicine, intending to facilitate access to health care services and reliable information on time, as well as decongesting hospital services[36].
However, in both cases, it is important to educate the patient, especially in confirmed cases of COVID-19 infection susceptible to outpatient management, emphasizing the importance of isolation and alarm signs, since there is no constant surveillance as there would be in hospital services, which leads to the risk of not effectively complying with the established quarantine periods.
It should be noted that the health system requires trained actors for its implementation who recognize the importance of comprehensive care from promotion and prevention, integrating the family as the foundation of society. For this reason, the specialty of family and community medicine, by meeting the needs of the community and the state, emerges as the main responsible for guaranteeing this approach. However, this should be present during the training of all health personnel and, in response to the immediate needs caused by the pandemic, the possibility of training other actors within the community outside the provision of services should be contemplated, strengthening it as the manager of its health[37].
Thus, the advantages of the change in the approach to providing health services have been identified. These include the decongestion of emergency departments by reducing unnecessary consultations, the opportunity for continuous access to reliable information, the provision of virtual consultations, and the follow-up of infected patients who do not require hospitalization[29].
3. Mental health
Public health emergencies lead to greater emotional distress and increased risk of psychiatric disorders, so the health system must intervene in emotional and mental health issues in response to the pandemic. Likewise, it is necessary to recognize the population at greater psychosocial risk, including those who contract COVID-19 or are at high risk of suffering it, previous use of psychoactive substances, and patients with pre-existing pathologies, mental or not. Specifically, in the previous epidemics for the severe acute respiratory syndrome (SARS) in 2003 and Ebola in 2014, fear-induced behavioral disturbances were observed in public coupled with increased levels of anxiety, depression, and post-traumatic stress disorder in survivors and health care workers that were evident even after the epidemic[38],[39].
On the other hand, excess information from unreliable sources, associated with a state of uncertainty faced by the population, can trigger psychiatric disorders and increase the risk of suicide. For example, in a study conducted after the closure of a U.S. university due to a gun attack, it was found that individuals exposed to misinformation through social networks reported higher levels of acute stress[20]. Also, when combined with isolation measures, there is an increased risk of feelings of anxiety and emotional tension[22],[38],[39].
At the same time, stress is inevitable in this type of situations, so it is recommended to take self-care measures in mental health; these include physical activity, performing social activities remotely via the internet or telephone, limiting the search for information about the crisis to official sources and no more than twice a day[22],[38],[39]. Similarly, the information provided must contain simple and understandable language for the entire population at the community level, avoiding the use of complex terms and using practical examples when informing[22].
Consequently, the need to implement community strategies through the Mental Health Gap Action Program (mhGAP) has been recognized worldwide by training non-specialized personnel for mental health care at the basic levels, allowing for a timely approach[40]. It is worth mentioning the program that emerged in China after SARS in 2003, which has been strengthened over time and is now available to respond to the COVID-19 pandemic[41]. In addition to the usual mental health care routes, telehealth was implemented in Colombia as a means of offering remote psychological assistance, mainly through the opening of telephone lines[42].
Discussion
We are currently in times of crisis, doubt, and uncertainty in the face of the COVID-19 pandemic. However, without undermining the victims and the economic, social, or political events that this has triggered, it can be stated that this event also represents an opportunity for improvement in health care processes, especially concerning primary care and the use of health technologies[43],[44].
Worldwide, inequity as one of the main challenges for health maintenance led to the proposal of the “health for all” program in the year 2000, giving importance to communities and using PHC strategies[45]. However, the region of the Americas needed to renew these concepts in 2005 to revitalize their adoption. Subsequently, in 2008, the need to include PHC in all the world’s health systems was recognized through the report “PHC more necessary than ever.”[46],[47],[48].
For Colombia, during the creation of its health policy, these aspects were not included until 2007, when interest in public health emerged. Four years later, in 2011, PHC strategies were implemented as the basis of its healthcare model. These include self-care elements, supervision, motivation of health personnel, and integration with the community, allowing for integrated, comprehensive, and continuous care. Additionally, these elements contribute to economic, political, and social development through the recognition of intersectionality as a key aspect for the health of its population[48],[49],[50].
Under this dynamic, the country has tried to advance new regulations, restructuring health care based on PHC strategies (Table 2). Consequently, favorable changes have been noted, mainly when comparing statistics such as life expectancy and mortality, added to the experiences from primary care for disease prevention, promotion, and health maintenance, focusing on the empowerment of people about their self-care[8].
 Full size
Full size However, although such strategies are conceptually adequate, since they revolve around the needs of a population in demographic transition such as the country’s, there is resistance to change. Colombia is a country with a hospital-centered, supra-specialized, and disease-centered tradition, which contributes to the fragmentation of services and makes it challenging to address SHD by overloading the provision of services in the hospital setting, in addition to other social factors such as inequity, special interests, and corruption[51],[52],[53]. Besides, the lack of recognition of the family physician as the main person in charge of fulfilling the integrating role of the different medical specialties hinders the comprehensive approach and the articulation of services with the community[37]. For this reason, despite the different efforts to include PHC in the regulatory framework of the country’s health system, its implementation has been patchy and marked by the selectivity of the plans related to this strategy to the detriment of comprehensiveness in the provision of health services.
The initial response to the pandemic in the country was based on isolation and self-care, without clarity in the regulations on the implementation of strategies from PHC and, at the same time, the strengthening of intrahospital services focused on intensive care units, given the experiences in other countries[19],[29]. Moreover, after three months, the isolation measures were made more flexible, establishing 43 exceptions to the national regulations despite the continuous increase in cases with a daily rate higher than that presented in previous months, showing how the importance of disease prevention measures is downplayed to avoid economic repercussions[54].
Similarly, this approach is evidenced in identifying cases by COVID-19 when testing only symptomatic patients, ignoring other vectors of infection such as the asymptomatic population and those who choose not to consult. On the contrary, from PHC and through the implementation of new technologies, countries that carried out an active search for cases and contact tracing with them achieved better control of the pandemic[18],[55].
In Latin America, the response of the different governmental entities is due to fragmented and hospital-centered health systems whose integration of PHC strategies has been partial. Notably, during the beginning of the pandemic, PHC took a back seat, being delayed by curative interventions at the intensive care level and whose control of the situation revolves around the follow-up of cases to determine the behavior of the curve, which has led to inadequate control of the pandemic. For example, in the case of Ecuador, the capacity of care was quickly exceeded, which led to the overflow of the system and increased mortality to the point of hindering the proper management of corpses. In contrast, countries such as Cuba, where PHC has been a fundamental pillar for the response, appear as points of reference for the opportunities offered by PHC for the region[56],[57].
Also, the scarcity of resources of individuals must be considered, as this may limit access to new telehealth technologies[31] and limits the adoption of self-care measures in vulnerable populations given the impossibility of acquiring personal protection elements or comply with recommendations for preventive isolation in the absence of formal employment and even, in more extreme cases, in the absence of a roof over their heads. For this reason, despite the timely implementation of the regulations in Colombia, there are still considerations to be considered for their feasibility[58],[59].
On the other hand, health care priorities have been reoriented towards responding to the pandemic, which, in combination with the role of hospital services in the transmission of the virus, has led to a decrease in emergency room visits due to fear of infection, leading to delayed care of acute pathologies, starting care at more advanced stages, all of which contributes to an increase in complications and mortality. Similarly, there is a risk of a decrease in the outpatient follow-up of the population with chronic diseases, which, in the future, may generate more complications in terms of their progression and lead to a possible collapse of the care systems due to mass consultations when the usual activities are resumed[60].
Faced with this situation, the PHC approach allows for the continuity of service provision during the pandemic. The implementation of these measures can effectively contribute to the maintenance of the health of the populations, becoming the primary tool in terms of preparedness for future health crises. However, it should be noted that the global situation due to COVID-19 transcends health barriers, and its approach requires intersectoral efforts given the social and political considerations involved in the restructuring of PHC-oriented health policies.
The limitations of this study include the rapid evolution and changes of the scientific literature on PHC and COVID-19, which will limit the applicability of the findings of this study over time. Additionally, due to the topic’s novelty, the available literature is scarce on the COVID-19 pandemic, particularly notorious for the Colombian case.
Conclusions
In Colombia, primary care is presented as an opportunity to respond to COVID-19 and the problems and needs derived from this situation. However, in the country, despite all the above, there is resistance to adopt this type of approach and to complement the hospital-centric model to face the pandemic.
Operatively, the response of relevant entities in Colombia to the situation has been timely, and the established regulatory framework allows for the adequate development of the work of health care personnel. However, it is necessary to strengthen the approach to the current situation from PHC in its practical component, to allow the maintenance of the integrality and intersectionality of health services, considering the follow-up of patients not affected by COVID-19.
The restructuring of the provision of services, the maintenance of mental health, and the implementation of new technologies are actions in response to the pandemic that, through PHC, not only contribute to the control of the spread of the virus but also optimize access to services through the integration with the community, empowering it in terms of self-care and health maintenance. For this reason, their articulation should be sought in the Colombian context once the health crisis is solved to guarantee the fundamental right to health.

