Analysis
← vista completaPublished on November 18, 2021 | http://doi.org/10.5867/medwave.2021.10.8490
Women’s access to health care: Gaps that the future health care reform in Chile must solve
Acceso de la mujer a la atención de salud: brechas que la futura reforma de salud en Chile debe resolver
Abstract
Introduction In the Chilean health system, difficulties complicate women’s access to health care and aggravate the complexity of health-illness processes in their interaction as users or caregivers.
Objective In the national and international literature, we aimed to identify gaps in women’s access to health care derived from gender disparities and the exercise of gender roles in a prioritized set of health problems. These problems exacerbate gender gaps and should be considered in health reform.
Methods We made a literature review through algorithms, snowball sampling, and reference lists from November 2020 to March 2021. The population included were women of all ages, including women users of the health system and women caregivers of specific pathologies. The search was conducted in parallel by four investigators divided into two groups. It was cross-validated to ensure inter-investigator reliability by standardizing evidence eligibility criteria. The analysis showed women users' and caregivers' dimensions for a set of pathologies prioritized by the extent of the disease burden. The pathologies analyzed included stroke, obesity, depression, musculoskeletal pain, and breast cancer.
Results Among women users of the health system, problems of access, rates of use, experience, and outcome for the whole group of prioritized pathologies were observed. In the women caregiver dimension, we found that women are the primary health care providers. There is a knowledge gap concerning obesity and musculoskeletal conditions. However, both were reported as health consequences of women’s caregiving roles.
|
Main messages
|
Introduction
Issues concerning women and gender roles have gained importance in recent times and mainstreaming a gender perspective in different intersectoral policies. Gender is described as the socio-cultural environment of a person [1] attributing roles in different environments. For example, women are being poorly visible and valued in the health sector [2]. These socially ascribed roles have contributed to gender disparities.
The health sector organizes care by prioritizing health problems for access to health technologies and interventions (e.g., care, medicines, medical devices) [3]. These are covered through care regimens [4] that prioritize disease burden, cost-effectiveness, quality, safety, and effects on final health measures. Although these regimens introduce segmentation categories (children, adults, older adults, pregnant women, women of reproductive age), segmentation by gender role is not clearly seen. Thus, it is necessary to investigate whether women's experience due to gender differences and their gender role affect rates of service use, the experience of care, or health outcomes [5]. Despite the low economic exclusion of health insurance in Chile [6], women still have difficulties accessing care, which determines a complex health-illness process. Among Chilean women, the burden of disease is greater than men. The predominant causes of years of potential life lost are neuropsychiatric conditions (25.9%), and digestive (17.9%), cardiovascular (10.8%), and musculoskeletal diseases (6.5%) [7].
The overall objective of this report is to identify experience and care gaps related to gender disparities and the exercise of gender roles among women users and caregivers. This study is based on a targeted review of international and national (Chile) experience in a prioritized set of high magnitude health problems responsible for a high disease burden. This issue is addressed from community-based health care settings up to quaternary care. The secondary objective of the review is to explore the effects on utilization rates and health outcomes affected by such gender gaps.
The overall purpose of this literature review is to provide technical elements to support a local discussion in Chile on what gender differences should be recognized by the health system when prioritizing the sector's activity in future health reform.
Methods
A set of health problems were prioritized for which there is a sufficient body of evidence on their local characterization (according to magnitude - prevalence among the general population and women in the 2016/2017 and 2009/2010 Chilean National Health Survey), and disease burden (final health measures: years of life lost, disability-adjusted life years). The burden of disease data in Chile was compared and complemented with the Institute for Health Metrics and Evaluation databank report of the Institute for Health Metrics and Evaluation at the University of Washington [8] (Table 1).
Based on the triangulation of sources, we chose to address the following health problems: stroke, obesity, depression, musculoskeletal diseases, and breast cancer.
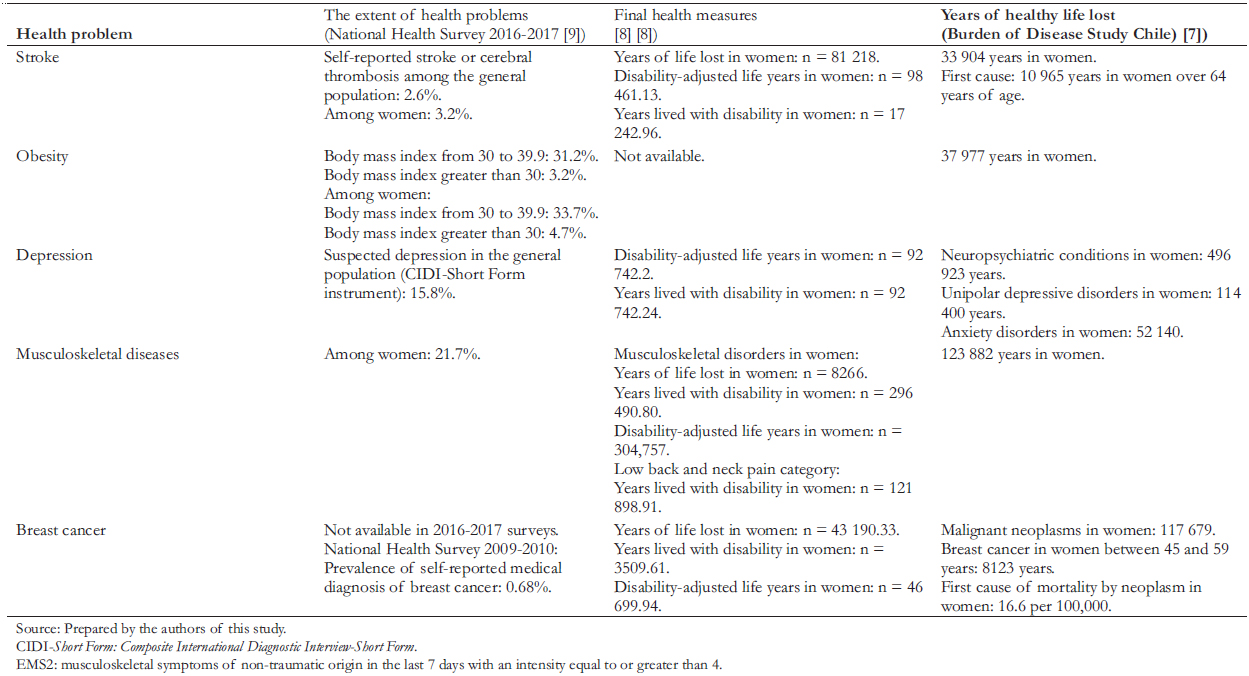 Full size
Full size For the literature review, a search strategy was defined according to population (women of any age, women users of the health system, and women caregivers), concept (access gaps), and setting (from quaternary to community care in any country). Each pathology was analyzed from two dimensions:
- Women healthcare users exposed to gender disparities.
- Women caregivers tied to gender roles.
The possibility of adding emerging categories was left open.
A targeted search was conducted in PubMed/MEDLINE and Science Direct, plus web search engines (Google Scholar, Google). Additionally, the reference list of retrieved evidence was examined and supplemented with snowball sampling to improve scope and saturation.
We chose to add web search engines to control for publication bias of unpublished evidence. For example, in PubMed/MEDLINE, the combination of MeSH terms, free words, and Booleans was created to generate search algorithms such as the following:
(("gender role"[MeSH Terms]) OR ("gender"[All Fields] AND "role"[All Fields]) OR "gender role"[All Fields]) OR (("womans"[All Fields] OR "women"[MeSH Terms] OR "women"[All Fields] OR "woman"[All Fields] OR "women s"[All Fields] OR "womens"[All Fields]) AND ("role"[MeSH Terms] OR "role"[All Fields])) AND (("stroke"[MeSH Terms] OR "stroke"[All Fields] OR "strokes"[All Fields] OR "stroke s"[All Fields]) AND ("healthcare disparities"[MeSH Terms] OR ("healthcare"[All Fields] AND "disparities"[All Fields]) OR "healthcare disparities"[All Fields])) AND ((y_10[Filter]) AND (fft[Filter])).
The search was performed in parallel by four researchers in two groups and cross-validated for inter-investigator reliability between November 2020 and January 2021, mapping full-text articles in English and Spanish, up to ten years old, adjusted to the researcher's skills. This process was done to increase the body of evidence necessary to achieve the objectives of this study, especially in pathologies where gender research is scarce.
Results
After first- and second-level screening, 86 studies were mapped. Most are dated between 2001 and 2016 (n = 54, 62.8%) and come from the Americas (n = 51, 59.3%), with predominant quantitative designs (n = 35, 40.7%). The health problem with the highest number of referrals was stroke (n = 25), followed by obesity (n = 21) and breast cancer (n = 18). The healthcare user dimension contributed 58 studies, while the caregiver dimension contributed 28 (Table 2).
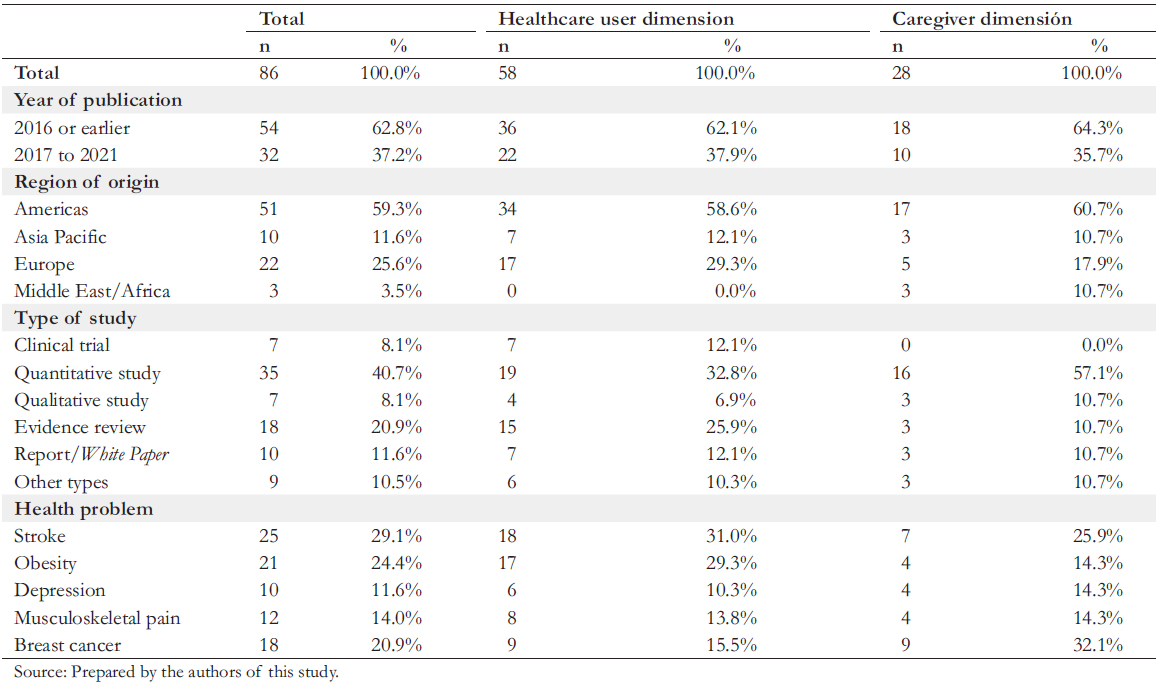 Full size
Full size Healthcare user women exposed to gender disparities
Women users with a stroke
In Chile, stroke or cerebral thrombosis is on the rise in women, with an increase from 1.7% to 3.2%, although it is indicated that the difference is not significant [9].
Even though risk factors such as hypertension and smoking are more frequent in men, these increase the risk to a greater extent in women [10]. Women may be more predisposed to worse outcomes due to their previous burden of disease and sociodemographic factors [11]. Higher prevalences of hypertension are reported among affected women. These vary among studies with statistically significant differences ranging from 4.8 to 9.3% compared to men [12],[13],[14],[15],[16]. The same occurs with atrial fibrillation and diabetes [12],[15],[16],[17].
Stroke affects mostly men, but in women, its occurrence is more lethal and severe [18],[19]. In Australia, women suffered more severe strokes than men (44% versus 36%, P = 0.01) and with a higher 28-day mortality (31% versus 23%, P = 0.003) [20].
Stroke in women is associated with less specific symptoms [10], which may affect recognizing the disease and delay immediate transfer to health centers [10]. This phenomenon is associated with delayed diagnosis and fewer possible timely interventions [21] to restore cerebral blood flow (i.e., thrombolysis and mechanical thrombectomy). In the United States, women were less likely to be thrombolyzed than men (Odds ratio: 0.84; 95% confidence interval: 0.69 to 1.03) [22]. Only 66.3% of women received all the care for which they were eligible, compared with 71.1% of men (adjusted Odds ratio: 0.86; 95% confidence interval: 0.85 to 0.87) [23]. A European multicenter study also reported that the access to benefits was lower in women (P < 0.001), with disparities in access to brain imaging (77.1% in women versus 85.7% in men), Doppler (32.8% versus 44.0%), and angiography (5.5% versus 9.5%) [17].
In addition, greater complications and worse prognosis are observed in women survivors [18],[21],[24], with a higher frequency of depression, impaired quality of life, and care dependence [21]. Coma (P < 0.001), paralysis (P < 0.001), swallowing problems (P = 0.005), urinary incontinence (P < 0.001) and aphasia (P = 0.001) are more frequent in women [17]. The five-dimensional self-administered EuroQoL quality of life questionnaire, the EQ-5D (that assess mobility, self-care, activities of daily living, pain/discomfort, and anxiety/depression), found that in all of its categories, quality of life impairment was higher in women than in men (mean difference of -0.07 on a scale of 0 to 1) [25].
According to international data, women are 60% less likely to regain their independence and experience low access to rehabilitation (46%) [26] and have a greater disability (Odds ratio: 1.20, 95% confidence interval: 1.06 to 1.36) [25]. Women have a 3.5 times higher risk of hospitalizations given their level of disability. Stroke affects their role in the home, employment, community, interpersonal relationships, and independence [26].
Women users with obesity
In Chile, morbid obesity and obesity are higher in women than in men (4.7% versus 1.7%, and 33.7% versus 28.6%, respectively) [9] and is more frequent in people with less than eight years of schooling [9]. According to Atalah, low socioeconomic status in men is not associated with obesity in contrast to women [27]. In the United States, it was reported that women with access to low-quality diets were more likely to suffer from obesity or overweight (Odds ratio: 1.76; 95% confidence interval: 1.16 to 2.69) [28].
Obesity in Chilean women of childbearing age range from 20 to 35.3% [29],[30]. Pregnant women attending the Chilean public system show a sustained increasing trend over two decades, reaching an obesity prevalence of 31.4% in 2016 [31].
Many studies show the association of maternal obesity with adverse maternal and perinatal outcomes during gestation (e.g., weight alterations and preterm labor syndrome) and delivery (e.g., increased risk of cesarean section and delivery complications). This association with adverse outcomes is maintained long after pregnancy due to its transgenerational effect on the development of chronic diseases such as hypertension, diabetes, and metabolic syndrome [30],[32],[33],[34],[35],[36],[37].
In other countries, the aim has been to explore additional ways to solve obesity beyond prevention and nutrition. Not only has medication-based management gained strength, but access to surgical procedures is consolidating as a valid treatment alternative for obesity in its most severe state while being complemented by behavioral medicine-based management. Between 2013 and 2017, Chile reported a total of 9712 bariatric surgeries in collaborating centers, highlighting comorbidities such as hypertension (25%), diabetes (18%), musculoskeletal pain (8%), and depression (5%). At 12 months, sleeve gastrectomy decreased depression from 7 to 3.7%; hypertension from 41.7% to 22.3%; and musculoskeletal pain from 26.3% to 15.7% [38].
The bariatric surgery program of the National Health Fund, in almost a decade of implementation, provided access mainly to lower-income beneficiaries in bracket A (no income; 23.8%) and B (income less than or equal to 337 000 Chilean pesos, equivalent to US$ 496.8 at the exchange rate as of June 2021; 46.75%) [39]. In Chile, 85.4% of the bariatric surgeries in this program benefited women [39]. Similarly, 80.7% and 71.3% of these procedures are performed in women according to international and national studies, respectively [38],[40]. However, within the public sector, only slightly more than three thousand cases are known to have been funded by the public insurance program over eight years. These numbers correspond to 1.02 persons per day nationwide [39].
The role of surgical interventions in obesity is not cosmetic and less so in women. The maternal and perinatal prognosis after bariatric surgery is positive, although some evidence refutes this [41]. In a systematic review, pregnancy followed by surgery was associated with fewer complications. In diabetes, 0% of complications were reported compared to 22.1% of cohorts without the surgery (P < 0.05); and in preeclampsia, 0% of complications compared to 3.1% in those without the surgery (P < 0.05) [42]. The procedure may contribute to a decrease gestational and pregestational diabetes, hypertensive syndrome and preeclampsia; in addition to chronic hypertension complicating pregnancy [43], low birth weight (7.7% versus 10.6%; P < 0.05) and macrosomia (7.7% versus 14.6%; P < 0.05) [42].
It remains to demystify access to therapies that can reduce weight in women and reduce other pathologies with a high burden of disease in them and their offspring. It is worth exploring how coverage schemes and multidisciplinary teams accompany women with obesogenic habits, who have access to diets of low nutritional quality, live in poverty, or are in charge of single-parent households in their struggle to reduce weight.
Women users with depression
Mental health problems constitute the primary source of disease burden in Chile [44]. The incidence of depressive disorders is higher in women, presenting twice the risk of major depression [45]. About 30% of pregnant women suffer symptoms of depression and/or anxiety [44].
Grundy et al. analyzed depression among older adults (n = 2 649) in Santiago de Chile and found that the prevalence of depression was statistically higher in women than in men (36% versus 21%, P < 0.001) [46]. During 2019, the Ministry of Health evidenced a high prevalence of depressive symptoms in the population aged 65 years and older, with women presenting a higher prevalence of depressive symptomatology (16.9% versus 4.1% in men) [47].
In a Covid-19 social survey, 21.4% of people presented a moderate/severe level of anxiety and/or depression symptoms according to the Patient Health Questionnaire-4 (PHQ-4) scale. This percentage was higher in women than men (26% versus 16.5%) [48]. Depression in women is also mediated by hormonal factors, which increase the risk of depression during periods of hormonal transition (menarche, pregnancy, and menopause) [45],[49].
Women users with musculoskeletal diseases
According to the National Health Survey, 42.8% of women have a pain greater than or equal to 4 on a scale of 1 to 10, in contrast to 25.2% in men [50]. In women, pain in the knee (22%), lower back (16.3 to 22.1%), and shoulder (11.1%) [50],[51] are the most frequent.
The prevalence of pain is higher in women [52] and increases over 45 years of age (50.6%), being more frequent among low schooling women (46.6%) [50]. Likewise, chronic and/or persistent pain is more recurrent in women users [53], with one-third of them living with pain for periods of over five years [50]. A total of 83.3% of those affected who live with chronic pain perceive their health as "bad/very bad" [54].
Chronic pain impacts professional life. In Chile, 44.2% of women workers live with chronic pain [55]. While 60.7% of women have medical leave associated with chronic pain, in men, this percentage is reduced to 39.3 [51].
Long waiting times for diagnosis, less access to treatment or less effective treatment, greater use of antidepressants, and more frequent referrals to mental health professionals describe the gender bias existing in pain management among women compared to men [56]. Thus, feminist perspectives on managing chronic pain in women emerge, addressing polypharmacy and cultural norms in their treatment [57].
Women user with breast cancer
Breast cancer is recognized as the most commonly diagnosed cancer in women [58]. In Chile, its incidence is increasing. In 2018 alone, it was the leading cause of death in women, with 1511 deaths [59],[60].
In Chile, breast cancer is covered by the Explicit Health Guarantees regime for access to prioritized benefits for diagnosis, treatment (i.e., surgery, hormone therapy, chemotherapy, radiotherapy), and follow-up. A special fund creates a financial protection system for high-cost diagnoses and treatments (Ricarte Soto Law No. 20,850) for therapies aimed at a subgroup of patients, whose proportion is estimated to be less than 20% of the total number affected women [61]. There was no access to high-cost innovative treatments for women outside this subgroup that improve survival through the Explicit Health Guarantees or the Ricarte Soto Law. Affected women resort to courts of law to access prohibitively expensive drugs without coverage. A Chilean study reported that women perceive that the health system provides coverage for all breast cancer treatments through the Explicit Health Guarantees, lacking knowledge about gaps in coverage in deprioritized subgroups and specific molecular profiles [62]. It is expected that the new High-Cost Drugs Committee will address this problem.
Currently, new models are being sought to be adopted. For example, the "role of the navigator" proposes a professional accompaniment for informative actions, decision-making, and educational needs in women [63]. The information needs of the family circle are part of breast cancer care [64], having been documented in adolescent sons and daughters of women with breast cancer. In Chile, school support is emphasized as an extension of care outside the health sector [65] and the needs of professional help for sons, daughters, and partners of the diagnosed woman, promoting family-centered models of care [66].
Caregiver women tied to gender roles
Women caring for stroke survivors
In the United Kingdom and Brazil, the proportion of women caregiving stroke survivors ranges from 64.2% to 77% [67],[68],[69], and the majority of caregivers are males [68].
The burden of caregiving has been cited as moderate-severe in 65% of survivor caregivers [70], allocating 6.3 hours per day (95% confidence interval: 4.5 to 8.1 hours) to informal emotional, physical, and supervisory caregiving [68]. Also, the time spent is greater in women caregivers than in male caregivers (P = 0.002) [69]. The caregiver's health is lower than the general population [68]. Sleep disturbances, physical and psychological stress [70], and even depression and anxiety increase as the caregiving burden increases [71],[72].
The caregiving pressure decreases when the caregiver is male [68] and increases when the survivor's severity worsens. This burden is greater for wives [69]. Wives and daughters perceive a more significant caregiving burden than other relatives (P = 0.019) [70].
Women caregivers assume caregiving with baseline deficiencies in the knowledge that would enable them to provide care [73], especially at higher levels of dependency [70]. Thus, caregivers must self-educate themselves to exercise this role without proper support from the healthcare system.
Women caring for people with obesity
Morbid obesity challenges caregivers by increasing difficulty assisting with mobility, skincare, and hygiene of physically impaired individuals [74]. In the United States, 62.4% of older adult women had obesity compared to 37.6% of men (P < 0.001). Obese patients had less access to care for daily living activities [75].
Caregivers of obese and pre-bariatric patients had greater lower back, shoulder and wrist pain, which was more frequent in women caregivers [76]. In women caregivers of adolescent patients who benefited from bariatric surgery, limited family dysfunction is reported. In addition, bariatric surgery does not affect caregiver distress, parental stress, or family functioning [77].
Women caring for people with depression
In Canada (n = 23 404), the frequency of women caring for people with depression is higher than male caregivers (26 versus 16.2%; P < 0.001) [78]. Women caregivers have a greater illness, psychological distress, anxiety, and depression than in the control group, perceiving greater emotional and physical burden, with less social support [79].
Male caregivers report caring for people with physical health problems (71.9% versus 66%; P < 0.001), while women caregivers do so mostly in mental health problems (7.7% versus 6.4%; P < 0.001) [78].
Women caregivers may develop depression, and there is insufficient evidence on who provides care for women with depression [80]. However, depressive symptoms in older adults are associated with having a male caregiver (P = 0.006) [81].
Women caring for people with musculoskeletal pain
The evidence focuses mainly on the musculoskeletal consequences of caregiving. In Japan, it is described that 78.2% of women caregivers have experienced low back pain associated with nighttime caregiving activities, changes in the position of the cared-for family member, problematic behaviors, and medication intake [82]. More women (81.8%) are caregivers of children when they have a disability, being more prone to low back pain and disability while caring [83]. Women with low back pain do not stop fulfilling other social and family roles. Nor do they decrease their housework burden (P < 0.05) [84].
Older women workers have a high risk of experiencing low back pain. Some contributing factors are work-family imbalance, exposure to a hostile work environment, and job insecurity. The occupations where women were most at risk of developing pain were agriculture, fishing and, forestry [85].
Women caring for people with breast cancer
Breast cancer impacts the family dynamics since women often have multiple roles: partner, mother, primary source of income and/or caregiver. When the main caregiver requires care, it is another woman, and it is usually a daughter who assumes the task [86],[87],[88],[89],[90], which is not exempt from physical and psychological health damage [91]. The World Health Organization indicates that many women who become ill with breast cancer and caregivers postpone or do not carry out their treatments so their family budget is not compromised [92],[93].
In Mexico, the concept of reciprocity of care is proposed when the cared-for woman provides emotional care to the caregiver. Despite their disease, these women continue to exercise a caregiving role to family members [94].
Discussion
The problems of access faced by women are based on a set of social inequities. Although Chile has a very high human development index [95], it falls to 17.8% when adjusted for inequality. The gender development index for 2018, in terms of gross national income per capita, was $29 933 for men, in contrast to $15 211 for women [95]. According to the Organization for Economic Cooperation and Development, the wage gap in Chile between men and women is 46.4 versus 38.1% average in member states [96], added to gaps in access to work (38.2% in women versus 61.8% in men), and higher unemployment [97],[98].
Extreme and non-extreme poverty is higher among women than among men [99]. When the woman is head of household, extreme poverty increases to 9.2% versus 6.4% in households headed by a man [100]. According to the National Institute of Statistics, 25.4% of women in 1992 were heads of household, a figure that increased 2.8 times in 2017 [101]. Moreover, 55.7% of women-headed households are single-parent [102].
The role of the caregiving women is invisibilized, stereotyped, and usually unpaid [103],[104],[105]. Moreover, it is fulfilled in a context of multi-role and physical and emotional exhaustion [103],[106].
Women caregivers present almost twice as much overload as male caregivers [107]. In Chile, from the total number of caregivers (n = 4313), there are more women than men (66.8% vs 33.2%; P < 0.05), with an average age of 56.5 years (standard deviation: 16.14) [108]. According to the latest National Time Use Survey of the Chilean National Institute of Statistics, employed, unemployed, or inactive women spend at least twice as many hours per day (5.89 hours) on unpaid work compared to men (2.74 hours) [109].
How can the health system address the present gender gaps among women who are users of health services and/or caregivers?
Almost a decade ago, the Economic Commission for Latin America and the Caribbean recommended incorporating a gender perspective in health programs in Chile [110]. Income inequalities open up spaces to propose contributions to social security, which reduce women's expenditure. Meanwhile, they can establish exercises to identify and prioritize benefits to resolve gaps and even regulate differentiated co-payments given the present inequalities.
The 'Chile Crece Contigo' social protection subsystem is oriented to the comprehensive protection of children, with the mission of accompanying, protecting, and supporting boys, girls, and families. This is done through universal actions and services, focusing support on those who present greater vulnerability. The latter is a step forward in the multisectoral approach for the comprehensive protection of children from gestation onwards. This same approach should be extended to other pathologies beyond a woman's role as a mother. The women's health program of the Chilean Ministry of Health has been an effort to prioritize sexual and reproductive health problems. However, the mainstreaming of gender and gender role has not permeated other health problems. In the regime of Explicit Health Guarantees, the approach to health problems between men and women and the exercise of gender roles is mainly undifferentiated. In it, financing is articulated to cover benefits and is not necessarily intended to solve health gaps. The latter would imply considering medical benefits, but also activities to solve gender gaps.
Women have access to health services while simultaneously taking care of children or the sick. Health plans (and the sizing of the services offered by providers in agreements with health insurance companies) should consider a greater offer of services for women. At the same time, these plans and providers should face the non-medical costs of their care.
The approach to care in some programs of the National Service for the Prevention and Rehabilitation of Drug and Alcohol Use provides rehabilitation services to women as users. It supports gender role needs when they are mothers [111]. This approach recognizes non-medical costs that act as access barriers for women. A cost study of such a model indicated that outpatient treatments for women were more expensive than treatments for the general population. The research reported differences of up to 313 053 Chilean pesos, equivalent to US$462.5 per month per patient, at the 2016 annual period exchange rate. In these, spending on food for users and their children implied 6.31% of the indirect cost. To avoid discontinuation of treatment, the centers had to face the following costs: mobilization of users, feeding of children, cradles and baby-changing facilities, and an accompaniment to health check-ups of the son or daughter and the user, and court appearances. Rehabilitation not only involves financing health care (psychiatric consultations, psychodiagnosis, antidepressants), but also supporting the gender role of women [111].
Limitations
In this literature review, the research and availability of evidence using a gender perspective and focusing on gender gaps may bias the interpretation of results. It should be noted that this review reports on care gaps in women users of the health system and caregivers. However, men can also play a gender role that involves caregiving. The latter aspect makes it necessary to articulate responses of accompaniment in health-illness processes, regardless of the sex of the subject of rights.
In addition, although the fact that this review is based primarily on international references may also be a limitation, in the absence of more Chilean evidence, this approach serves as a trigger for discussion.
Conclusions
The evidence shows access gaps in women users and caregivers within pathologies of high disease burden. All this translates into different rates of care access, treatment, and health outcomes (e.g., disability, quality of life). The underlying problem seems to be explained by biological, social, and cultural gender gaps that permeate the health care environment.
Given the exercise of different gender roles, the health sector should recognize that it is necessary to consolidate comprehensive therapeutic models and approaches in social security, aiming at effective formulas for prioritization, health insurance, and gap resolution.
Women's health care has different needs, even more so when they exercise specific gender roles. It is necessary to discuss how Chile will allow a better approach to these gender gaps in view of the constitutional discussion and health reform.
Notes
Contributor roles
DP: conceptualization of the report, methodological development, use of reference management software, verification of the reproducibility of the review process, formal analysis of the evidence review, research process, metadata production, manuscript writing and final editing, supervision, and administration of the research project. RL: verification of the reproducibility of the review process, formal analysis of the evidence review, research process, metadata production, manuscript writing and final editing. BC - CR: development of the methodology, use of reference management software, verification of the reproducibility of the review process, formal analysis of the evidence review, research process, metadata production, manuscript writing, and final writing and editing.
Competing interests
Analysis carried out in alliance between Academics from Universidad de Chile, Academics from Universidad Andrés Bello, and Medtronic Chile. The authors have completed the ICMJE conflict of interest declaration form and declare that they have received support from Medtronic to fund the journal processing charges. The authors declare that they are fully responsible for the content of this article. Forms can be requested by contacting the responsible author or the Journal's editorial office.
Funding
Medtronic supported the present work by paying Medwave's processing charges.
Ethics
The present article is exempt from evaluation by an ethics committee because of the origin of the study design, which corresponds to a review of the literature (study in secondary sources of available literature).
Data sharing statement
Authors declare that they are willing to share data or any information of interest from the manuscript. Contact the corresponding author.
Language of submission
Spanish.

