Problemas de salud pública
← vista completaPublicado el 4 de mayo de 2021 | http://doi.org/10.5867/medwave.2021.04.8180
Condiciones pre-existente en Latino América y factores asociados con resultados adversos en COVID-19: Una revisión
Pre-existing conditions in Latin America and factors associated with adverse outcomes of COVID-19: A review
Abstract
The coronavirus disease 2019 (COVID-19) pandemic, produced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly throughout the world. Latin American and the Caribbean countries have been harshly affected by the pandemic mainly due to less prepared healthcare systems and fragmented social safety nets. In the region, health status population-based indicators are worse than compared to the Organization for Economic Cooperation and Development. Recent evidence suggests that the progression and severity of COVID-19 are associated with the prior health status of individuals, and studies have shown that the case fatality rate is highly stratified among different populations. This narrative review aims to describe factors associated with adverse outcomes of COVID-19 in the context of social determinants of health in Latin American and Caribbean countries. In this review, we state that genetic and biological factors interact in a sophisticated way with social determinants of health, impacting the rapid spread of COVID-19 in Latin American and Caribbean countries. Behavioral factors, such as physical inactivity, smoking, and unhealthy diets, are related to chronic systemic inflammation. Also, air pollution can prolong inflammation and the hyper-activation of the immune system. Air pollutants could facilitate the spread of the virus. Finally, frailty and comorbidities can be associated with COVID-19 severity through increasing vulnerability to stressors and leading to more severe symptoms of COVID-19 disease, including a higher mortality risk. All these factors contribute to increasing the impact of COVID-19 in Latin American and Caribbean countries. We highlight the relevance of considering social determinants of health in Latin American and the Caribbean countries, not only in controlling the likelihood of getting the disease but also its progression and severity. All these social determinants can guide the design and implementation of tailored interventions promoting healthy lifestyle behaviors, which should lower the spread of the disease, its severity, and lethality.
Main messages
- Evidence suggests that the progression and severity of COVID-19 are associated with the social determinants of health.
- Latin American and the Caribbean countries have been harshly affected by the pandemic mainly due to less prepared healthcare systems and fragmented social safety nets.
- Our study explains how social health determinants have influenced the health indicators related to the COVID-19 pandemic in Latin American and Caribbean countries.
- Comorbidities, obesity, tobacco use, environmental pollution, physical inactivity, age, and frailty have been strongly associated with the progression of COVID-19.
- We are still in time to make behavioral changes that improve our health status and boost our immune response to infections.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, resulting from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly throughout the world. Latin American and the Caribbean countries have been harshly affected by the pandemic mainly due to less prepared healthcare systems and fragmented social safety nets. In the region, healthcare systems have significantly lower capacity, but the health status of population-based indicators is worse than other Organization for Economic Cooperation and Development (OECD) countries [1]. In addition to the health impact of the COVID-19 pandemic, a significant socioeconomic effect is expected in the region along with the resulting exacerbation of health and social inequalities.
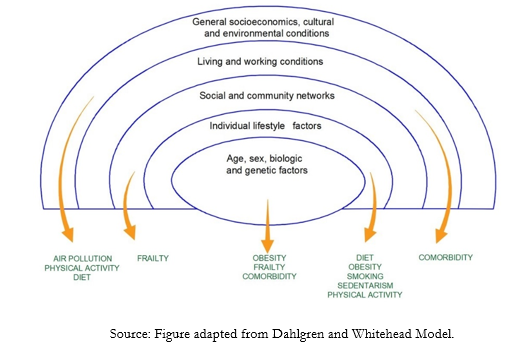
The evidence is still growing regarding the factors associated with adverse outcomes of COVID-19. However, some recent evidence suggests that the progression and severity of the disease are associated with the prior health status of individuals [2], and studies have shown that the case fatality rate is highly stratified among different populations. The analysis for the differences between risk groups must be done on individual risk factors and considering the sociological and ecological perspectives of health. The social determinants of health include the conditions in which people live and work and the broader forces that influence daily life, such as biological and genetic factors, individual lifestyle factors, living and working conditions, and general socioeconomic, cultural, and environmental conditions. These conditions affect a wide range of health risks and outcomes, and COVID-19 is no exception (Figure 1).
 Full size
Full size Comorbidity, obesity, tobacco use, environmental pollution, physical inactivity, age, and frailty have been strongly associated with COVID-19 progression. These risk factors could generate overlapping vulnerability levels and be better understood through the social determinants of health model. The social determinants of health model states that health is affected by the interaction between individual characteristics, the community, and the environment and provides a framework for understanding the factors associated with the unfavorable progression of COVID-19. Furthermore, the social determinants of health model makes it possible to address preventive measures in a comprehensive approach. Each level in the social determinants of health model can be thought of as a level of influence and a key point for prevention. This narrative review aims to describe factors associated with adverse outcomes of COVID-19 in the context of social determinants of health in Latin American and the Caribbean as an overview of the current evidence base to provide recommendations to achieve a practical impact at multiple levels.
Social determinants of health and pre-existing health context in Latin American and the Caribbean countries
The pre-existing health status of a population is affected by the social determinants of health that include economic stability, social context, education, the physical environment, and the health care system. Despite significant advances in recent years, inequality and poverty remain high in Latin American and the Caribbean, with great disparity between countries [3]. The Human Development Index, which divides countries according to a composite index that takes into account health, education, and economy, classifies Latin American and the Caribbean countries into four categories: “very high” (Chile, Argentina, and Uruguay), “high” (Panama, Costa Rica, Cuba, Mexico, Brazil, Colombia, Peru, Ecuador, Bolivia, and the Dominican Republic), “medium” (El Salvador, Guatemala, Nicaragua, and Honduras) and “low” (Haiti) [4]. This inequality is reflected in structural factors, and few Latin American and the Caribbean countries have focused their efforts on developing intersectoral policies that address the social determinants of health [5].
Regarding to health systems, reforms have attempted to implement universalization of a minimum of healthcare coverage. Different strategies have been observed in public policies: the explicit health guarantees plan in Chile, the popular health insurance in Mexico, and the health reform in Colombia. Likewise, Brazil has opted for universal access through the creation of a Unified Health System. Some Latin American and the Caribbean countries have shown a relatively high margin of response capacity in the surge of demand for health services due to the COVID-19 pandemic, such as Barbados, Cuba, and Argentina. At the other extreme, countries such as Honduras, Haiti and Guatemala have shown a lower capacity [6].
Social protection policies in Latin American and the Caribbean have a long history in Argentina, Chile, and Uruguay, with more recent trajectories in this field, such as El Salvador, Guatemala, and Honduras [7].
The social determinants of health influence the health population and make people more vulnerable to more COVID-19 severe infections. Latin American and the Caribbean countries are the geographic areas where the COVID-19 pandemic has attacked more severely, accounting for 34% of deaths attributable to the infection worldwide [8]. Brazil is the second country globally with the highest number of confirmed cases after the United States. On the other hand, Mexico, with a relatively low incidence of COVID-19 but a very high prevalence of obesity, diabetes mellitus, and hypertension, has one of the highest fatality rates in the region [9]. In Chile, the proportion of hypertension, diabetes mellitus, and obesity among patients hospitalized for COVID-19 is two to three times higher than those who did not require hospitalization [10].
Regarding aging, cross-national studies on the prevalence of frailty have shown that frailty was positively associated with older age, female sex, and lower socioeconomic status [11], manifesting health inequities in Latin American and the Caribbean.
Social determinants of health influence behaviors like smoking, diet, and physical activity; also, the exposure to environmental pollution is higher in low socioeconomic status communities [12]. Related to air pollution, the annual mean values of particulate matter (PM) 10 and particulate matter 2.5 in large cities of Latin American and the Caribbean are significantly higher than the World Health Organization Air Quality Guidelines. Approximately 58,000 deaths per year are attributable to ambient air pollution in Latin American and the Caribbean [13]. Lima, the capital city of Peru, is one of the most polluted cities in Latin America. A recent study conducted in Peru showed that exposure to high levels of 2.5 particulate matter in the years preceding the COVID-19 pandemic was associated with a higher incidence and mortality from COVID-19 [14], suggesting that the current incidence of COVID-19 could be associated with chronic exposure to air pollution.
Diet in the region is a matter of concern because there have been profound changes in the last decades, resulting in unhealthy diets characterized by high consumption of ultra-processed food, which favors overweight and obesity [15]. According to the Organization for Economic Cooperation and Development, Chile has the highest rate of overweight and obesity (74%), followed by Mexico (72.5%) [16]. Furthermore, more than 80% of active smokers live in low and middle-income countries [17]. In Latin American and the Caribbean, approximately one in four men aged 15 or older reported smoking every day, but the proportion of daily tobacco smokers varies greatly across countries [1]. Finally, on average, 35% of the adult population does not engage in enough physical activity.
Methods
A narrative review was performed. The purpose of narrative reviews was to describe factors associated with adverse outcomes of COVID-19 in the context of social determinants of health. This paper summarizes the critical and personal analysis of the authors. The search was carried out between April and June 2020. The terms used for the primary search were: “risk factors” combined with “COVID-19”. In a second search, the terms used were: “comorbidity,” “obesity,” “tobacco,” “air pollution,” “physical activity,” and “frailty” combined with “COVID-19”.
No limitations were set for study countries. The search was carried out in MEDLINE/PubMed, EMBASE, Cochrane, and bioRxiv. The study included original articles, reports, reviews, and preprints paper.
Results and discussion
Factors associated with adverse outcomes of COVID-19
The pre-existing health context could explain the significant impact of the pandemic on incidence and mortality indicators in Latin American and Caribbean countries. The biological plausibility for factors associated with adverse outcomes of COVID-19 is explained with an emphasis on comorbidity, obesity, tobacco use, environmental pollution, physical inactivity, age, and frailty. Although we do not deny that these risk factors can interact with each other, worsening COVID-19 progression, we choose them for several reasons. First, they are highly prevalent in the Latin American and the Caribbean population; second, they understand how several risk factors from different population levels can compromise health outcomes; and third, they can be targeted with interventions to reduce their health impact.
Comorbidity
The relationship between COVID-19 and chronic diseases such as hypertension, diabetes mellitus, cardiovascular disease (CVD) are complex and could increase infection susceptibility or affect the prognosis. The interactions between comorbidities and COVID-19 are sufficiently supported by angiotensin-converting enzyme 2 (ACE2) participation in the pathogenesis of many chronic diseases and its role as a SARS-CoV-2 receptor [18]. On the other hand, angiotensin-converting enzyme 2 is not restricted to the respiratory epithelium; it is also found in myocardium cells, endothelium, renal tubular and intestinal epithelium, and pancreatic islets [19]. Chronic diseases such as diabetes mellitus, in addition to the recognized deficit in neutrophil chemotaxis and phagocytosis, generate membrane furin protease overexpression that favors the SARS-CoV-2 entry into the cell and interleukin 6 (IL-6) overexpression that increases the COVID-19 cytokine storm [20]. Finally, protease dipeptidyl peptidase IV (endopeptidase DPP4), involved in diabetes treatment, could have a role in SARS-CoV-2 infections.
Many studies on chronic disease prevalence in COVID-19 do not establish whether the carriers of these comorbidities are at higher risk of getting the infection [21]. The evidence that links comorbidities with the prognosis of COVID-19 is much stronger. A systematic review and meta-analysis by Wang et al. included primary studies that compared COVID-19 clinical severity according to the presence of chronic disease [22]. They found that the risk of serious illness expressed as an odds ratio was 5.97 for chronic obstructive pulmonary disease, 3.98 for stroke, 2.93 for cardiovascular disease, 2.51 for kidney disease, 2.47 for diabetes mellitus, and 2.29 for cancer and hypertension. Similarly, a prospective cohort study from the United Kingdom analyzed the risk of dying from COVID-19 with multiple variables such as comorbidities, age, sex, and socioeconomic factors [23]. The adjusted risk of dying from COVID-19 expressed as a hazard ratio was 2.36 for uncontrolled diabetes mellitus, 1.79 for stroke and dementia, 1.72 for kidney disease, 1.61 for liver disease, and 1.27 for chronic cardiovascular disease. Having a hematological and non-hematological neoplasm with less than one year of diagnosis carried a hazard ratio of dying of 3.52 and 1.56, respectively.
Obesity and nutrition
Obesity is a risk factor for SARS‐CoV‐2 severity, especially in young people and men [24]. A link between obesity and SARS-CoV-2 implies a hyperactivation of the complement system, increased interleukin 6 secretion, chronic inflammation, and a possible detrimental local effect on the lung. A study reported a higher body mass index in non-survivors (body mass index > 25 kilograms per meter squared in 88.24% of non-survivors). Moreover, a recent report by the Intensive Care National Audit and Research Centre (ICNARC) of the National Health Service (NHS) reported that 38% of SARS-CoV-2 patients in critical care in the United Kingdom were obese and that these patients died in critical care in 57.6% of the cases versus 45% of those with a body mass index < 30 kilograms per meter squared [24].
Patients infected with COVID-19 can develop a “cytokine storm.” Excess body fat is associated with an overreaction of the complement system, which acts as a mediator in disease due to SARS-CoV-2. It has been suggested that the virus uses the angiotensin-converting enzyme 2 receptors as an intracellular entry. This receptor is also expressed in adipocytes. Watanabe et al. [24] hypothesize that obesity can play a role in the predisposition to more severe manifestations for COVID-19 through chronic systemic inflammation, increase in the activation of the complement system, and secretion of interleukin 6, in addition to its relation to other chronic pathologies. Excess body fat can also allow ectopic adipocytes to enter into the alveolar interstitial space, possibly worsening the prognosis. On the other hand, a balanced and wide-ranging diet that provides the necessary nutrients to help in maintaining immunity is essential for the prevention and management of viral infections [25].
Different studies have shown that micronutrients such as vitamins (A, B6, folate, B12, C, D) and minerals (zinc, iron, selenium, magnesium, and copper) play an essential and synergistic role in the immune response [26],[27]. However, the daily micronutrient intake required to maintain immune function may be higher than current recommended dietary allowances [27].
There are several ways in which vitamin D reduces the risk of viral infection [26],[27],[28]. These include inducing cathelicidins and defensins, both with broad antimicrobial activity, that can lower viral replication rates and reduce the cytokine storm induced by the immune system. Also, hypovitaminosis D can increase the risk of death in patients with COVID-19, boosting pro-inflammatory cytokines [29]. A meta-analysis of clinical trials demonstrated that vitamin D has a protective effect against respiratory tract infections (odds ratio: 0.64; 95% confidence interval: 0.49 to 0.84) [30].
Vitamin C is another micronutrient that has emerged as a potential therapy due to its multiple benefits [31]. There is an ongoing randomized clinical trial assessing the efficacy and safety of vitamin C in SARS-CoV-2 viral pneumonia (NCT04264533).
Jayawardena et al. showed in a meta-analysis that in addition to a healthy diet, the supplementation of vitamin A, D, and zinc, and selenium might be beneficial for the prevention and treatment of COVID-19 according to the measurement of immunological parameters in viral and respiratory infections. On the other hand, several nutraceuticals (for example, capsules of aged garlic extract, fish oil, or elderberries) and probiotics (of example Lactobacillus and Bifidobacterium) can enhance immunity against viral infection [25].
Tobacco use
Although evidence is still accumulating on the links between COVID-19 and tobacco, emerging data indicate that smoking increases the severity of COVID-19 symptoms. A recent systematic review with the limited available data, which included five studies conducted in China, shows that smoking is most likely associated with negative progression and adverse outcomes of COVID-19 [32]. A study conducted in China among patients infected with COVID-19, a history of smoking increased the likelihood of progression of pneumonia by up to 14 times [33]. Previous studies have also shown that smoking affects the immune system, making smokers more vulnerable to infectious respiratory diseases like influenza or the previous Middle East respiratory syndrome coronavirus (MERS-CoV) [34] because cigarette and tobacco smoke contains numerous human carcinogens, toxins, chemically reactive solids, and oxidants, which generate adverse effects on the airway epithelial cells [35],[36]. Thus, tobacco smoke exposure conducts to increased mucosal inflammation, oxidative stress, and expression of inflammatory cytokines, such interleukin 6, interleukin 8 (IL-8), and tumor necrosis factor-alpha (TNF-a), and the direct effects on the respiratory epithelium include enhanced permeability, impaired mucociliary clearance, mucus overproduction, increased release of pro-inflammatory cytokines, enhanced recruitment of macrophages and neutrophils and disrupted The helper 1/The helper 2 lymphocyte balance towards The helper 2 [35].
It is known that chronic obstructive pulmonary disease is strongly associated with smoking habits. Chronic obstructive pulmonary disease is significantly associated with an increased risk of various respiratory tract infections and appears to increase the risk of a more severe course of the COVID-19 infection [37]. Besides, there is an increased risk of more severe symptoms and death among COVID-19 patients with other underlying chronic conditions, such as hypertension, diabetes mellitus, cardiovascular disease, and cancer. Tobacco use is also a major cause of cardiovascular diseases globally and is a leading global cause of death. On the other hand, smoking cessation is the single most preventable cause of chronic diseases. Moreover, nicotine has been associated with the upregulation of angiotensin-converting enzyme 2, the receptor for SARS-CoV-2, highlighting the importance of smoking and vaping cessation.
Environmental pollution
There is emerging evidence about the association between air pollution and incidence and lethality of COVID-19. Air pollution adversely affects health, prolonging inflammation and eventually leading to an innate immune system hyper-activation. Air pollution has several components, including various gases and tiny particles of solids or liquids suspended in the air, called ambient particulate matter. Particulate matter 2.5 is defined as ambient airborne particles measuring up to 2.5 microns in size, and it is the pollutant most harmful to human health because its microscopic size allows the particles to enter the bloodstream via the respiratory system and travel throughout the body [38].
A study conducted in Italy showed that air pollution played a crucial role in propagating COVID-19 [39]. Another study found a correlation between the high lethality of COVID-19 and the high level of air pollution in northern Italy. There is a possible association between air pollution and the development of acute respiratory distress syndrome and death due to COVID-19.
The high agglomeration of air pollutants could facilitate the spread of SARS-CoV-2 [40]. This association was shown during the severe acute respiratory syndrome (SARS) outbreak in China in 2002. A study found a correlation between the increase in the air pollution index and fatality rate due to SARS across five regions in China [41]. The atmospheric particulate matter exercises a carrier (or boost) action along with the virus. Atmospheric particulate matter has a sub-layer that facilitates the survival of the virus in airflows for hours or days. The local atmospheric aspect is another issue that must be considered in the accelerated diffusion of this virus. On the other hand, COVID-19 has facilitated activation rates in the presence of high local relative humidity, while it is inhibited in hot climates [39]. Data from northern Italy and Wuhan (China) show that air pollutants, such as particulate matter, nitrogen dioxide, and carbon monoxide, are most likely to facilitate the longevity of virus particles in favorable climate conditions [40].
Wu et al. investigated the effect of long-term average exposure to particulate matter 2.5 on COVID-19 mortality in the United States. They found that an increase of only 1 microgram per cubic meter in particulate matter 2.5 is associated with a 15% increase in the COVID-19 death rate (95% confidence interval: 5% to 25%) [42]. The study included approximately 3,000 counties (98% of the population), with data on exposure to air pollution from 2000 to 2016. Urgent actions are required to control air pollution to reduce the burden of COVID-19 in the countries most affected by the pandemic.
Physical activity and sedentary
It has been suggested that we are currently facing the coexistence of 2 pandemics [43], one produced by COVID-19 and another of physical inactivity (characterized as a global pandemic in 2012) [44], and the two could be interacting. SARS-CoV-2 infection is characterized by an aggressive inflammatory response triggered by the generation of pro-inflammatory cytokines and chemokines. This inflammatory process and the host response are strongly implicated in the resulting damage to the airways and disease severity [45]. Additionally, it is known that regular physical activity and exercise are associated with numerous physical and mental health benefits and reduced risk of all-cause mortality. Moreover, exercise is a therapy for several chronic diseases characterized by chronic low-grade inflammation, such as metabolic, cardiovascular, or pulmonary diseases [46]. Thus, a recent review suggests that prior exercise training and high levels of cardiorespiratory fitness are likely to be immune-protective in patients who contract SARS-CoV-2 [47], where interleukin 6 plays a crucial role in the anti-inflammatory effect of exercise. Myokines like interleukin 6 inhibit tumor necrosis factor-alpha production and stimulate the anti-inflammatory cytokines interleukin-1 receptor antagonist (IL1ra) and interleukin 10 (IL-10). Therefore, endurance exercise training that improves cardiorespiratory fitness, such as increasing maximum oxygen uptake [48], creates an immediate anti-inflammatory environment of particular interest for subjects with illnesses like obesity, diabetes, or cardiovascular diseases that cause chronic low-grade inflammation. Implementing strategies to reduce the spread of COVID-19 (such as quarantines at regional or national levels on all continents) and the adverse population effects of physical inactivity and sedentary behavior should be a central issue because it is highly acknowledged that physical inactivity (for example, not meeting physical activity guidelines) and sedentary behavior (for example, sitting for too long) are associated with cancer, cardiometabolic and mental risk [49] factors and diseases as well as a reduction in functional capacity, among others. Nowadays, people worldwide are staying at home more, avoiding public spaces such supermarkets or even parks due to physical distancing strategies, resulting in a considerable reduction in mobility [50]. The situation we are experiencing affects all age groups, and the adverse population effects of physical inactivity and sedentary behavior are still unknown. However, given that physical inactivity and sedentary behavior are so widespread, we can estimate significant negative impacts on physical fitness, including functioning and metabolic responses. Experimental studies have shown adverse effects after relatively short exposure to physical inactivity and sedentary behavior (1 to 2 weeks), affecting mood and depressive symptoms [51], reducing muscle protein synthesis rates [52], and reducing multi-organ insulin sensitivity and cardiorespiratory fitness, with associated effects on central and liver fat and dyslipidemia [53]. For all this, it is necessary to make an effort to implement strategies that reduce the negative impact of physical inactivity and enhance the beneficial effects of physical activity and exercise.
Frailty
Age is associated with an increased risk for severe COVID-19 disease and mortality [54]. Chronic illnesses may not only be a contributor to COVID-19 mortality but also other related conditions like frailty. Frailty is a geriatric clinical syndrome characterized by three or more of the following criteria: unintentional weight loss, exhaustion, weakness, slowness, and reduced physical activity. This syndrome is formed due to the alterations produced by the diseases or by the skeletal muscle changes, skeletal muscle mass loss, or anorexia due to age. Various physiological systems will be altered in this condition, leading to presenting greater vulnerability to a stressor. Thus, frailty syndrome could explain the increased vulnerability to a more severe COVID-19 disease and greater risk of mortality in the older population.
Older adults with poor diets, unhealthy lifestyles, and comorbidities will have a higher risk of developing frailty. In this sense, we hypothesized that mobility restriction due to COVID-19 would generate an increase in frailty levels in the short term. A recent rapid systematic review drew on scientific literature published before COVID-19 to state possible strategies to combat frailty. Part of these considerations was that older people in their homes with a reduction in their daily activities due to prevention by COVID-19 must receive telerehabilitation to prevent/combat frailty, sarcopenia, and other mental states such as cognitive impairments and depression [55]. The evidence is there showing that regular physical activity is safe for both healthy and fragile older people. Different types of physical activity, whether low intensity such as walking or high intensity such as practicing vigorous sport, reduce the risks of developing cardiovascular, musculoskeletal, or metabolic pathologies [56]. Finally, evidence in physical activity shows that it can improve functional independence and reduce mortality associated with chronic diseases despite starting at advanced stages of life.
Conclusion
COVID-19 disease is spreading rapidly worldwide. Its progression, severity, and lethality are associated with biological and genetic factors and social determinants of health such as lifestyle behavior, living and working conditions, socioeconomic position, environmental and cultural factors. This context could explain the significant impact of the pandemic on the incidence and mortality indicators in Latin American and Caribbean countries.
In this review, we state that genetic and biological factors interact in a sophisticated way with social determinants of health, impacting the rapid spread of COVID-19 in Latin American and the Caribbean. Two mechanisms underlying this association are chronic systemic inflammation and the angiotensin-converting enzyme 2, expected in several chronic conditions such as diabetes and obesity. Behavioral factors, such as physical inactivity, smoking, and unhealthy diet, are also relevant. These factors are related to chronic systemic inflammation and impact the respiratory tract permeability, mucus production, and impaired mucociliary clearance. Diet quality can contribute micronutrients that may foster the immune system, lower viral replication rates, and the impact of pro-inflammatory cytokines.
Environmental variables are also related to COVID-19. Air pollution is potentially linked to COVID-19 severity. It has been well demonstrated that air pollution can prolong inflammation and the hyper-activation of the immune system. Furthermore, air pollutants could facilitate the spread of the virus.
Finally, frailty syndrome can be associated with COVID-19 severity. Due to its decline in the functioning of multiple physiological systems, frailty increases vulnerability to stressors and could lead to more severe symptoms of COVID-19 disease, including higher mortality risk.
We highlight the relevance of considering social determinants of health in Latin American and Caribbean countries, not only in controlling the likelihood of getting the disease but also its progression and severity. These social determinants can guide the design and implementation of tailored interventions promoting healthy lifestyle behaviors, such as reducing weight and ameliorating comorbidities, which should lower the disease’s spread, severity, and fatality.

