Reporte de caso
← vista completaPublicado el 13 de octubre de 2023 | http://doi.org/10.5867/medwave.2023.09.2716
Síndrome de disfunción orgánica múltiple progresiva en embarazo adolescente: reporte de caso clínico
Progressive multiple organ dysfunction syndrome in adolescent pregnancy: Case report
Abstract
Introduction Adolescent pregnancy is a physiological process, but it can evolve with premature delivery, severe obstetric or clinical pathologies, mortality, or sequelae for mother and child. We aim to report the progressive multiple organ dysfunction syndrome secondary to pyelonephritis and sepsis during prepartum, delivery, and puerperium of adolescent pregnancy and its sequelae.
Case report A 14-year-old adolescent with a pregnancy of 27 weeks of gestation controlled from 8 to 25 weeks. She was urgently admitted to the high-risk obstetric unit due to signs of preterm labor, pyelonephritis, and acute renal injury. Treatment was started with intravenous cefazolin and betamethasone for lung maturation, oral nifedipine, and magnesium sulfate to prevent preterm labor and fetal neuronal protection, evolving with sustained hypotension and septic shock. At 13 hours after admission, she was transferred to the intensive care unit, where she evolved with persistent and progressive multiple organ failure for 28 days, progressively affecting the cardiovascular, hematologic, respiratory, and gastrointestinal systems. She was treated with vasoactive drugs, antibiotics, invasive mechanical ventilation, ultrafiltration, hemodialysis, pleural drainage, and cholecystectomy. Twenty-four hours after admission to intensive care, preterm vaginal delivery occurred. She developed chronic kidney disease stage KDIGO 5 (Kidney Disease Improving Global Outcomes V) and is awaiting renal transplantation. On the other hand, the preterm newborn presented severe neonatal asphyxia, bronchopulmonary dysplasia, and hypoxic-ischemic encephalopathy.
Conclusion Complicated adolescent pregnancy is a health emergency. Avoiding delays in the diagnosis and treatment of pyelonephritis, septic shock and the progressive multiple organ dysfunction syndrome can prevent mortality and permanent sequelae, both maternal and neonatal.
Main messages
- Obstetric and clinical complications during pregnancy and childbirth are the second leading cause of death worldwide in women between 15 and 19 years of age, doubling the risk in children under 15.
- Progressive multiple organ dysfunction in adolescent pregnancy is a complication of rare occurrence in the perinatal period.
- This work describes the clinical phenotype of progressive multiple organ dysfunction in adolescent pregnancy, the first case reported in Chile.
Introduction
Pregnancy is a physiological process that can occur from menarche to menopause and directly impacts the health, life, and personal development of the mother, child, family, and society. Adolescent pregnancy occurs between menarche and the end of adolescence (between 10 and 19 years of age). It poses major health, psychosocial, and economic risks, which is why preventing it is a global objective. The world rate of adolescent pregnancy is 46 births per 1000 girls. Chile is the only South American country to have achieved a rate lower than the global rate of 40.1 per 1000 adolescents by 2019 [1]. Poor socioeconomic conditions, family dysfunction, teenage pregnancy in the family, and low schooling are the underlying causes of early pregnancy [1,2,3]. Obstetric and clinical complications during pregnancy and childbirth are the second leading cause of death worldwide among 15 to 19-year-olds, with the risk doubling in those under 15 years of age in low- and middle-income countries [4]. The main causes of complications in general and adolescent pregnancy in particular are hyperemesis gravidarum, hemorrhage due to ruptured ectopic pregnancy, and septic abortion during the first trimester. Subsequently, preeclampsia, preterm delivery, pyelonephritis, sepsis, obstetric hemorrhage, fatty liver, and thrombotic microangiopathy with intravascular hemolysis may occur [5,6,7].
Pyelonephritis can progress to sepsis, septic shock, and multiple organ dysfunction. Sepsis, defined as life-threatening organ dysfunction caused by an exaggerated host response to infection, is the leading cause of maternal and pediatric death [8,9]. Septic shock is a severe infection that progresses to cardiovascular dysfunction (including hypotension, requiring vasoactive drugs). Primary multiple organ dysfunction syndrome is defined as two simultaneously dysfunctional organs within the first week of admission and no subsequent organ dysfunction. Meanwhile, other organ dysfunctions develop in sequence in persistent or progressive organ dysfunction syndrome [9,10]. We aim to report this complication of rare occurrence in the perinatal period in a pregnant adolescent.
Case report
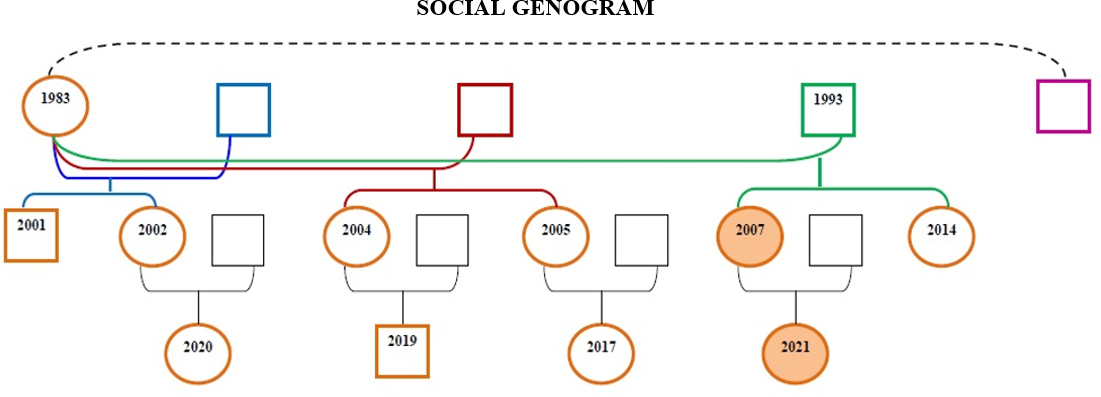
We present the case of a 14-year-old adolescent girl, previously healthy and eutrophic. She had a body mass index of 28.7, was studying eighth grade (last year of primary school in Chile), primigravida, and was 27 weeks pregnant, monitored according to national guidelines from 8 to 25 weeks. Four of these controls were performed in primary care (twice in person and twice online by COVID-19 confinement) and three times in an obstetric high-risk polyclinic. Prenatal examinations were normal, including urinary sediment and urine culture during the first trimester. The patient had poor socioeconomic conditions: single-parent, single-family household, family dysfunction, and a history of adolescent pregnancy in both mother and three sisters (Figure 1).
Social genogram and family relationships.
She was urgently hospitalized at an obstetric high-risk clinic for three days, with a fever of up to 39 degrees Celsius, lumbar pain, vomiting, and painful uterine contractions. She had hypotension 70/34 millimeters of mercury (107.1 ± 8.0/ 67.6 ± 8.5 millimeters of mercury), tachycardia 117 beats per minute (87.4 ± 10.6 per minute), mucocutaneous pallor, cold extremities, capillary refill less than two seconds, cervix effaced 30%, one-centimeter dilatation, membranes intact, fetal heartbeat 130 per minute (110/160 per minute).
Admission tests revealed metabolic acidosis, pH 7.32 (7.35 to 7.45), bicarbonate 18 micromoles per liter (19 to 25 micromoles per liter), anemia, leukocytosis 23 700 per cubic millimeter (6 to 16 x 103 per cubic millimeter), neutrophilia 19 813 (3.8 to 10 x 103 per cubic millimeter), normal platelets 124 000 per cubic millimeter (110 to 400 x103 x cubic millimeter), C-reactive protein 27.6 micrograms per deciliter (less than 0.5 micrograms per deciliter), serum creatinine 2.26 micrograms per deciliter (low 0.8 micrograms per deciliter) and urinary sediment compatible with infection.
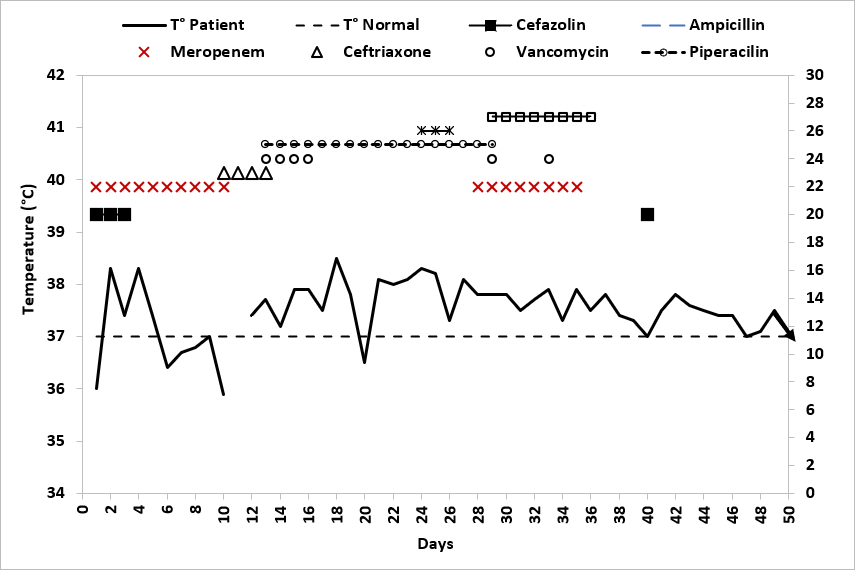
She received intravenous hydration, blood cultures were taken, and she started treatment with cefazolin one gram every 8 hours for 48 hours. In addition, she received two doses of betamethasone 6 milligrams; oral nifedipine 20 milligrams every 20 minutes for three times, then 10 milligrams every 6 hours, and magnesium sulfate five grams followed by one gram every 8 hours, evolving with hypotension and anuria. Blood cultures were positive for Escherichia coli. At 13 hours after admission, she was transferred to the intensive care unit and diagnosed with KDIGO III (Kidney Disease Improving Global Outcomes III) and septic shock due to Escherichia coli with multiple organ dysfunction. She received noradrenaline up to 1.5 micrograms per kilogram per minute, invasive mechanical ventilation for six days, hydrocortisone at a dose of 100 milligrams, then 50 milligrams every eight hours for seven days, meropenem one gram every 12 hours for two days then one gram every 24 hours for six days and renal replacement therapy with intermittent venous hemodiafiltration for four days. Subsequently, she was left on hemodialysis three times a week.
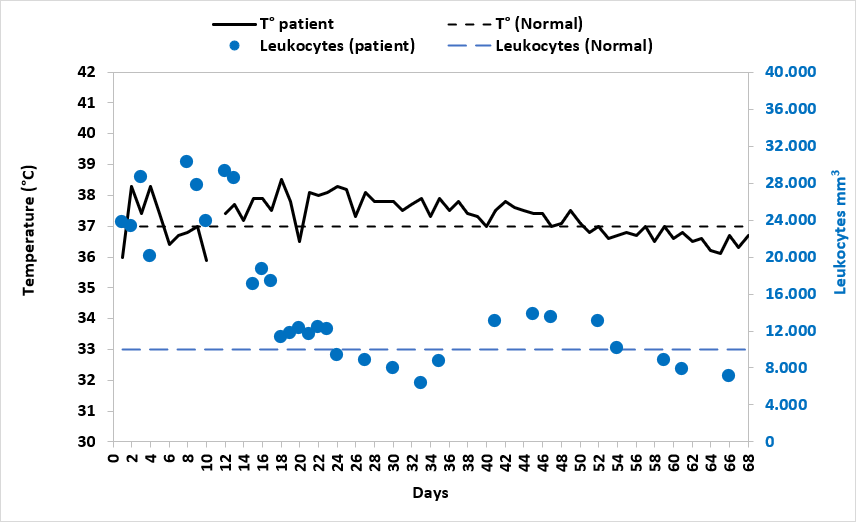
Twenty-four hours after admission to the intensive care unit, vaginal delivery occurred. The 27-week-old newborn weighed 1310 grams, measured 32 centimeters, had a head circumference of 24 centimeters, and APGAR 0-2-2. Resuscitation was performed for 14 minutes with cardiac massage, orotracheal intubation, three doses of adrenaline, and one dose of surfactant, and was admitted to the neonatal critical care unit. The mother evolved with persistent fever, hematological parameters, acute phase reactants compatible with bacterial infection, and elevated creatininemia (Figures 2 and 3). Persistent cardiovascular and renal dysfunction was followed by septic ileus, ascites, and cholecystopancreatitis, which led to cholecystectomy. Subsequently, atelectasis and surgically drained pleural effusion were added. The patient presented with hemolytic anemia and thrombocytopenia that were treated with transfusions of red blood cells, platelets, and erythropoietin. Other etiologies of infection, obstetric, hematologic, and immunologic compromise were ruled out (Table 1). The imaging study showed decreased bilateral renal parenchymal vascularization and extensive necrosis of both kidneys, predominantly right, choledocholithiasis, pneumonia, atelectasis, and pleural effusion.
Temperature curve in degrees Celsius and leukocytes per cubic millimeter curve.
Serum creatinine curve in micrograms per deciliter and hemoglobin curve in grams per deciliter.
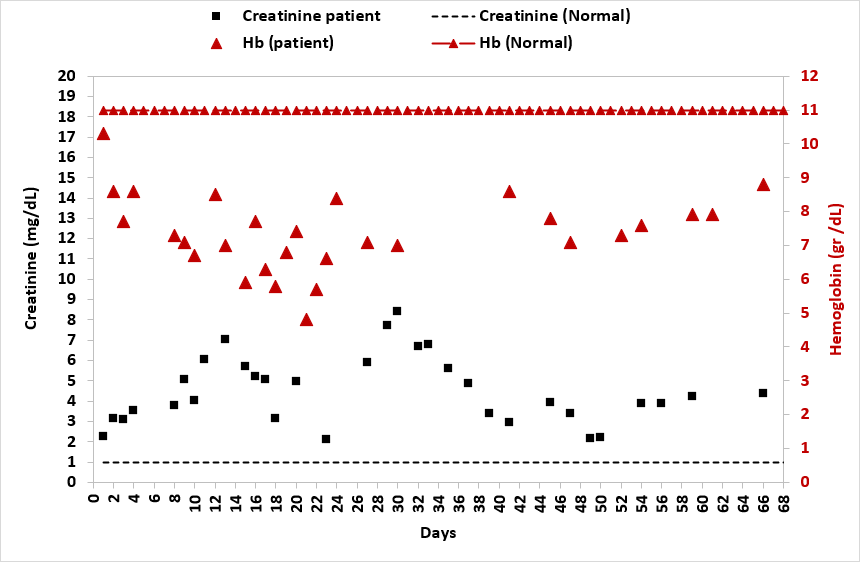
After eight days of meropenem and without bacteriological evidence in the new cultures (except for Pseudomonas aeruginosa in bronchoalveolar lavage and right jugular vein catheter tip, interpreted as colonization but with clinical and laboratory parameters of uncontrolled infection), the patient received several antibiotics and an antifungal agent. Thirty days of antimicrobials were completed, the fever subsided, and the hemogram and C-reactive protein normalized (Figures 2 and 4). Renal function remained impaired, compatible with chronic kidney disease that evolved to stage 5 (KDIGO V) (Figure 3).
Temperature curve and sequential use of antibiotics.
The patient had no previous history of renal pathology. She received psychological and legal support. She resumed her education in a hospital school and in an external online educational institution. During outpatient follow-up at the children’s nephrology polyclinic almost two years later, tests showed pre- and post-hemodialysis urea nitrogen of 36 and 10 micrograms per deciliter, respectively, serum creatinine of 4.38 micrograms per deciliter and glomerular filtration rate of 14.2 milliliters per minute per 1.73 square meters. The adolescent is currently on the waiting list for renal transplantation.
The newborn evolved with hypoxic-ischemic encephalopathy, hyaline membrane, bronchopulmonary dysplasia, oxygen requirements for 200 days, severe gastroesophageal reflux treated with Nissen fundoplication, swallowing disorder, metabolic bone disease of prematurity, sepsis, and severe psychomotor developmental delay. The family court, considering the familiar dysfunction and the characteristics of the adolescent mother, including the severe renal pathology and the child’s condition, gave her custody to a foster family responsible for the assistance of a multidisciplinary rehabilitation team.
Discussion
To our knowledge, this is the first reported case at the national level describing the clinical phenotype of progressive multiple-organ dysfunction in an adolescent pregnancy. The adolescent had a satisfactory prenatal control according to national standards [11], consulting for infectious complications late (three days of fever over 39 degrees Celsius), probably due to an underestimation of urosepsis symptoms, family dysfunction, unfavorable socioeconomic conditions, and home confinement due to COVID-19. Complications in adolescent pregnancy are infrequent but can cause mortality and sequelae. Since 2000, there have been decreases in adolescent mortality, especially in Southeast Asia, where rates have decreased from 21 to 9 per 100,000 [12]. In Chile, there have been no cases of adolescent maternal mortality recorded in the last six years, and the infant mortality rate is 7 per 1,000 newborns under one year of age [13]. International publications report obstetric complications similar to those of adult pregnant women, which in general may also result in acute renal injury [4,5,6,7]. A national report comparing obstetric and clinical complications between adult and adolescent pregnant women shows a percentage difference, although not significant, of a higher incidence of urinary tract infection in adolescents [14]. The publication that addresses the entire population of pregnant women in Chile describes higher rates of preterm delivery and preeclampsia in adolescents [12]. Other national references emphasize the psychological, educational, economic, social, and personal development consequences for the mother, child, family group, and society as a whole [2,3], situations present in our case.
Despite the physiological immaturity, no higher rate of cesarean section has been demonstrated [5,6,7]. Physiological changes in renal function during gestation favor the development of urinary tract infection, so prenatal control tests were requested and were normal. However, the patient developed pyelonephritis, acute renal injury, and urinary sepsis with multiple organ failure during the last trimester.
Pregnancy-related acute renal injury fluctuates between the first and fourth cause of admission to the intensive care unit. It may be due to decreased renal perfusion, ischemia, nephrotoxicity, tubular renal obstruction, tubulointerstitial or glomerular alterations of prerenal, renal, or postrenal cause, with prerenal being more common [15,16,17,18,19,20]. The etiologies depend on the time of gestation: during the first trimester, they are related to septic abortion, hyperemesis gravidarum, and hemorrhage due to ruptured ectopic pregnancy. During the second and third trimesters, they are associated with preeclampsia (including hemolysis syndrome), altered liver tests and thrombocytopenia (HELLP, Hemolysis Elevated Liver Enzymes, and Low Platelet Count), sepsis, obstetric hemorrhage, fatty liver and thrombotic microangiopathy with intravascular hemolysis [15,16,17,18,19,20]. On the other hand, the incidence of acute renal injury in shock and/or sepsis is 50%, and mortality varies between 35 and 60% in patients requiring renal replacement therapy, a risk that lasts two years. It is also a risk factor for chronic kidney disease [21].
Abarca et al. 2021, introduced the current approach for the early diagnosis and treatment of acute kidney injury of any cause [21]. International references reviewed pregnancy-associated acute kidney injury in detail, its causes, pathophysiology, diagnosis, treatment, and fetal and maternal prognosis, albeit in the adult population [15,16,17,18,19,20]. The adolescent presented with acute pyelonephritis that progressed to sepsis due to Escherichia coli, septic shock, and acute renal injury. Sepsis can trigger a systemic inflammatory response, causing disseminated tissue injury [9,10,22]. Bacteria have molecules in their cell wall that are recognized by receptors found on the immune cell surface: toll-like receptors (TLRs). Binding to these receptors triggers the activation of nuclear factor kappa-B (NFKB1), which increases the transcription of cytokines such as tumor necrosis factor α (TNF-α), interleukin-1 ß, proinflammatory cytokines that activate the immune response, but can also produce damage. Sepsis increases the synthesis of nitric oxide, a potent vasodilator. Cytokines activate endothelial cells via adhesion receptors and injure these cells, causing neutrophils, monocytes, macrophages, and platelets to adhere to them. These cells release mediators such as proteases, oxidants, prostaglandins, and leukotrienes that lead to endothelial damage, increasing permeability, generating vasodilatation, and alteration of the procoagulant-anticoagulant balance. Cytokines also activate the coagulation cascade, especially factors Va and VIII a, leading to the formation of thrombin, which converts fibrinogen to fibrin. Fibrin adheres to platelets, forming thrombi in the microvasculature. Thrombi increase injury by mediator release and microvascular obstruction, causing distal ischemia and tissue hypoxia [9,10,22]. Sepsis is the leading cause of multiple organ dysfunction syndrome [23], characterized by simultaneous dysfunction of two or more organs, including respiratory, cardiovascular, neurological, renal, hematological, and gastrointestinal/hepatic systems associated with a severe, dysregulated systemic inflammatory process. Other risk factors for multiple organ dysfunction syndrome include severe hypoxemia, cardiorespiratory arrest, shock (present in our case on admission), trauma, acute pancreatitis, intestinal ischemia, acute leukemia, solid organ or hematopoietic stem cell transplantation, hemophagocytic lymphohistiocytosis, thrombotic microangiopathy, and poisoning. Weiss reports modifiable process-of-care factors associated with multiple organ dysfunction syndrome, including delayed primary and iatrogenic injury treatment [24]. Carcillo et al. have studied the pathophysiology of multiple organ dysfunction syndrome in pediatrics, noting that there are:
-
Reduction of cytochrome P450 metabolism is inversely proportional to inflammation levels.
-
Increased circulating damage-associated molecular pattern molecules (DAMPS) of injured tissues.
-
Increased circulating pathogen-associated molecular pattern molecules (PAMPS) of the infection or endogenous microbiome.
-
Cytokine-driven epithelial, endothelial, mitochondrial, and immune cell dysfunction with persistent macrophage activation.
The combination of decreased cytochrome P450 metabolism, circulating tissue injury-related damage-associated molecular pattern, and circulating pathogen-associated molecular pattern lead to self-injurious cytokinemia. In turn, cytokinemia can lead to:
-
Epithelial cell dysfunction and apoptosis manifesting as acute respiratory distress syndrome, hepatobiliary dysfunction, and/or acute renal tubular dysfunction.
-
Endothelial cell dysfunction and apoptosis manifesting as thrombotic microangiopathy with loss of microvascular homeostasis.
-
Mitochondrial autophagy (mitophagy) and dysfunction manifest as catabolism, hibernation, and dysautonomia.
-
Immune cell dysfunction and apoptosis manifest as lymphoid organ depletion with ineffective microbial clearance and tissue repair [10].
Sepsis is the leading cause of multiple organ dysfunction and death in pediatrics and pregnant women [8,9,10,22,23,24,25,26,27,28,29]. In 2001, the Surviving Sepsis Campaign (SSC) was formed, and in 2016, different guidelines for adults and children were issued in addition to the global initiative against maternal and neonatal sepsis [9,25,26,27,28]. Maternal sepsis was defined as "a life-threatening condition characterized by organ dysfunction as a result of infection during pregnancy, delivery, puerperium, and post-abortion." The Global Maternal Sepsis Study (GLOSS) campaign was designed to accompany the global maternal sepsis study to raise awareness of maternal sepsis. The study conducted in 52 countries of different income levels showed, among other results, that few were able to identify the criteria defining maternal sepsis [27,28], suggesting that diagnosis is not easy. The documents originating from the different adult, pediatric, and maternal working groups [9,23,24,25,26,27,28,29] agreed to emphasize the importance of early diagnosis and treatment, reinforcing the concept that the first hour is transcendental to reduce mortality and sequels. They also agreed that, although education and awareness are transcendental, they alone are insufficient to improve outcomes. This highlights the need for improvements in the healthcare system, such as the availability of critical resources and support. Evans et al. (2021) recommended that hospitals and healthcare services develop a performance improvement program for sepsis, including sepsis screening for patients with acute and high-risk illnesses and standard operating procedures for treatment, as sepsis and septic shock are medical emergencies [25]. Nunnally et al. 2021, emphasized that locally created protocols using standard criteria and outcomes are able to increase interdisciplinary participation and coordination [26].
Another tool to be implemented could be electronic alerts on clinical records, which could support early detection as well as efficient and timely delivery of high-quality interventions to patients with sepsis.
Sequential antimicrobials and aggressive hemodynamic and renal compromise treatment were used in the intensive care unit. She progressively presented gastrointestinal and respiratory impairment, both severe factors that make up the recently described progressive multiple organ dysfunction phenotype, to which higher mortality and sequelae have been attributed. The definition, epidemiology, causes, monitoring, and prognosis are detailed in the references [10,23,30,31].
Conclusions
In the reported case, socioeconomic vulnerability, a family history of adolescent pregnancy, and family dysfunction contributed to the early pregnancy. Despite satisfactory prenatal control, the consultation was late when signs of systemic infection, hemodynamic compromise, and premature delivery were already evident. Adequate management of acute renal injury, sepsis, and progressive multiple organ failure in the intensive care unit allowed both mother and daughter to survive. Nevertheless, both developed permanent sequelae.

