Reporte de caso
← vista completaPublicado el 8 de abril de 2024 | http://doi.org/10.5867/medwave.2024.03.2792
Traqueobroncopatía osteocondroplástica: reporte de cuatro casos clínicos
Osteochondroplastic tracheobronchopathy: Four case reports
Abstract
Introduction Osteochondroplastic tracheobronchopathy is a rare benign chronic disease of unknown etiology. Bronchoscopy remains the gold standard for diagnosing osteochondroplastic tracheobronchopathy. Its typical findings are described as a cobblestone, rock garden, mountainscape, or stalactite cave appearance. The present work aims to show the main clinical features of this rare pathology.
Clinical cases The clinical data of four middle-aged patients, three men and one woman, were analyzed. The main clinical symptoms were chronic cough, dyspnea, and dysphonia. The patient's preliminary diagnosis was made by computed axial tomography of the chest, confirmed by bronchoscopy and histopathological examination. Treatment included medication for symptoms and, in one case, cryosurgery and argon plasma coagulation.
Discussion Diagnosing osteochondroplastic tracheobronchopathy was not easy, given its uncommon nature and non-specific symptoms often found in other pathologies. No case series articles on this pathology have been published in Peru. Therefore, we used the original articles published in other countries to reference our findings.
Conclusion Osteochondroplastic tracheopathy is a benign disease that typically affects adults. Men are more likely to be affected. Its clinical manifestations are non-specific and frequently of pharyngeal origin, and the cause is not yet defined. Chest computed axial tomography combined with bronchoscopy are the main diagnostic procedures. There is no standard treatment with consistent therapeutic effects.
Main messages
- Osteochondroplastic tracheobronchopathy is a rare chronic disease of unknown cause with non-specific clinical manifestations.
- This paper provides information on the clinical and bronchoscopic presentation of osteochondroplastic tracheobronchopathy, which may be useful in suspicion, early diagnosis, and management of such a rare condition.
- A limitation of this report is the small number of cases.
Introduction
Osteochondroplastic tracheobronchopathy is a rare, chronic benign disease characterized by multiple submucosal cartilaginous or bony nodules, which project into the lumen of the lower two-thirds of the trachea and the upper part of the main bronchi [1]. In some cases, the larynx and subglottic trachea may also be involved [2,3], causing multiple respiratory symptoms. The disease progresses slowly and can obstruct the trachea and bronchi [4]. The etiology of osteochondroplastic tracheobronchopathy remains unknown. Numerous theories have been proposed, including genetic factors, metabolic disorders, chemical or mechanical irritation, and chronic inflammation and carcinogenesis.[3,5,6].
The English physician Wilks made the first observation of osteochondroplastic tracheobronchopathy on necropsy specimens, which was initially diagnosed as tuberculosis [7]. Von Schroetter is credited for being the first to document the diagnosis in vivo in 1896 [8]. The incidence is estimated to be approximately 0.5% [9,10].
It is frequently misdiagnosed or missed for the following reasons: etiology and pathogenesis are unclear [11,12], clinical symptoms are non-specific, specific risk factors are not defined, and physicians have little knowledge.
The most common clinical symptoms include chronic cough and wheezing; other non-specific symptoms include chest tightness, shortness of breath, dyspnea, and hoarseness [5].
Currently, bronchoscopy remains the gold standard for recognizing osteochondroplastic tracheobronchopathy. Its typical findings are described as a cobblestone, rock garden, mountainscape, or stalactite cave appearance [6,13,14,15]. It is classified bronchoscopically according to its evolution:
-
Stage I: Scattered inflammatory plaque-like yellow-whitish infiltrations throughout the mucosa, as well as edema and mucosal hyperemia.
-
Stage II: The scattered or diffuse presence of sessile spicules and cartilaginous nodules projecting into the lumen gives a "typical cobblestone" or stalactitic cave appearance.
-
Stage III: Characterized by deformation, rigidity, and stenotic airway that may cause airflow obstruction [10].
Case reports
Case report 1
Patient EYEOM, a 47-year-old woman from Trujillo, Peru. She reported having a dry cough, recurrent dysphonia, and pharyngeal pruritus for approximately nine months. Several otorhinolaryngologists evaluated her. On different occasions, she was treated with corticosteroids, antihistamines, N-acetylcysteine, and antibiotic therapy, considering the diagnosis of chronic allergic rhinitis. Due to persistent symptoms, on December 30th, 2019, a rigid video laryngoscopy was performed. This revealed the presence of multiple subglottic nodulations up to the trachea (Figure 1). As a result of these findings, and because she developed wheezing, she was referred to a neumonology specialist.
Rigid laryngoscopy video: Subglottic and tracheal whitish nodulations.

Medical history: no relevant history.
Risk factors: none.
Physical examination: respiratory rate of 16 cycles per minute, pulse rate of 78 per minute, oxygen saturation of 98% at 21% oxygen-inspired fraction.
Lungs: vesicular murmur in both lung fields, no audible wheezing.
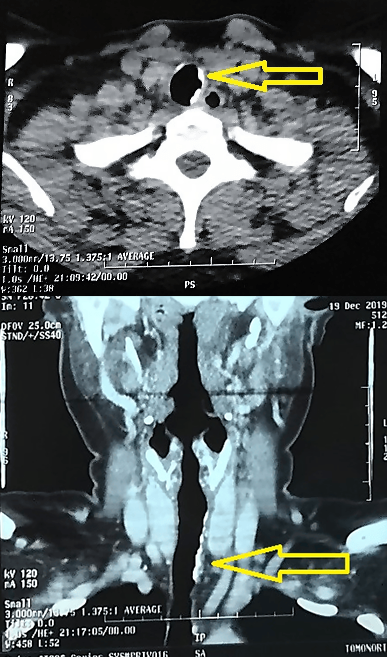
Complementary studies: chest and neck computed axial tomography (performed on December 20th, 2019) showed the trachea with irregular mural calcifications up to three millimeters thick, predominantly on the left side throughout its length, conditioning irregularity and slight stenosis of the lumen (Figure 2, A and B).
Chest computed axial tomography: A, Coronal view. B, Sagittal view. Irregular mural calcification of up to three millimeters thick predominantly on the left side, throughout its entire length, conditioning irregularity and slight stenosis of the lumen (arrow).
Hematology and biochemistry (taken on January 10th, 2020): hemogram, hemoglobin, coagulation profile, glucose, urea, and creatinine within normal ranges.
Spirometry (taken on February 17th, 2020): restrictive spirometric pattern.
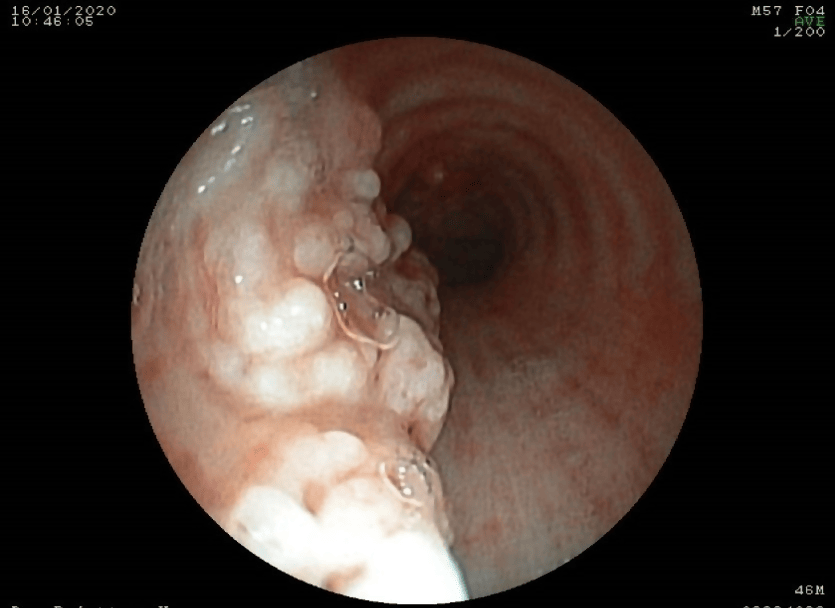
A video bronchoscopy was performed, which revealed the presence of abundant whitish nodular lesions of cartilaginous appearance, emerging from the submucosa in the anterior and lateral walls of the trachea and proximal area of the right and left main bronchial branches (Figure 3). Biopsy samples, carina and tracheal wall brushings, and bronchial aspirate were taken. Histological examination of the biopsies reported segments of respiratory epithelium without significant histological alterations. Brushing of the main carina lesions showed the presence of respiratory epithelial cells without evidence of neoplastic cells. Few areas of leukocytic exudate were observed. Fungal culture, common germs culture, and bronchial aspirate smears were negative.
Bronchoscopy showing cartilaginous nodules projecting into the light like a "typical cobblestone" or stalactite cave-like appearance.
Due to episodes of increased coughing, dysphonia, and dyspnea on exertion, and with the diagnosis of osteochondroplastic tracheopathy, she was referred to a private institution where she received five cryosurgery sessions with flexible cryoprobe and argon plasma coagulation at intervals of six to eight months. The last session was performed in December 2022. After each session, she presented partial remission of symptoms. She attended her check-ups, and on June 17th, 2023, a spirometry study was performed, which showed values of forced expiratory volume in the first minute of 109% and forced vital capacity of 97% (normal).
The patient reported that cryoprobe and argon plasma interventions are long processes but seem to "work".
Case report 2
CVM patient, male, 55 years old, from Trujillo, Peru. He reported dysphonia and pharyngeal pruritus for two months; he denied having cough or dyspnea. He was evaluated by otorhinolaryngology several times and received several antibiotic therapy regimens without improvement. In October 2022, rigid video laryngoscopy was performed, which revealed the presence of subglottic granulomas. Due to the persistence of symptoms and the described findings, he was referred to the neumonology department.
History: two-years history of psoriasis.
Risk factors: None.
Physical examination: Respiratory rate of 18 cycles per minute, pulse rate of 75 per minute, oxygen saturation of 98% at 21% oxygen-inspired fraction, blood pressure of 120/70 millimeters of mercury.
Lungs: there was a vesicular murmur in both lung fields; no abnormal respiratory sounds were auscultated. The rest of the examination revealed no relevant findings.
Complementary studies (taken on November 5th, 2022): chest X-ray showed no alterations. Non-contrast computed axial tomography of the neck reported diffuse tracheal irregular nodular thickening, partially calcified, associated with stenosis, suggesting osteochondroplastic tracheobronchopathy (Figure 4).
CT scan of the neck showing diffuse tracheal irregular nodular tracheal thickening partially calcified (arrows).
Hematology and biochemistry (taken on November 10th, 2022): Hemogram, hemoglobin, coagulation profile, glucose, urea, and creatinine within normal ranges.
Spirometry (performed on November 17th, 2022): Forced vital capacity, forced expiratory volume in the first second, and forced expiratory volume in the first second/forced vital capacity within normal ranges.
Bronchoscopy showed abundant granulomatous lesions emerging from the submucosa, extending from the anterior and lateral wall of the trachea to the right and left main bronchial branches. Whitish nodular lesions of cartilaginous appearance were also seen, emerging from the submucosa in the anterior and lateral walls of the trachea and proximal to the right and left main bronchial branches. In addition, mucopurulent secretion was observed in moderate quantity (Figure 5). Biopsy samples were taken from the carina, trachea, and right and left main bronchi. Bronchial aspirate was also performed to study common germs and fungi.
Bronchoscopy video shows abundant granulomatous trachea lesions extending into both main bronchi.
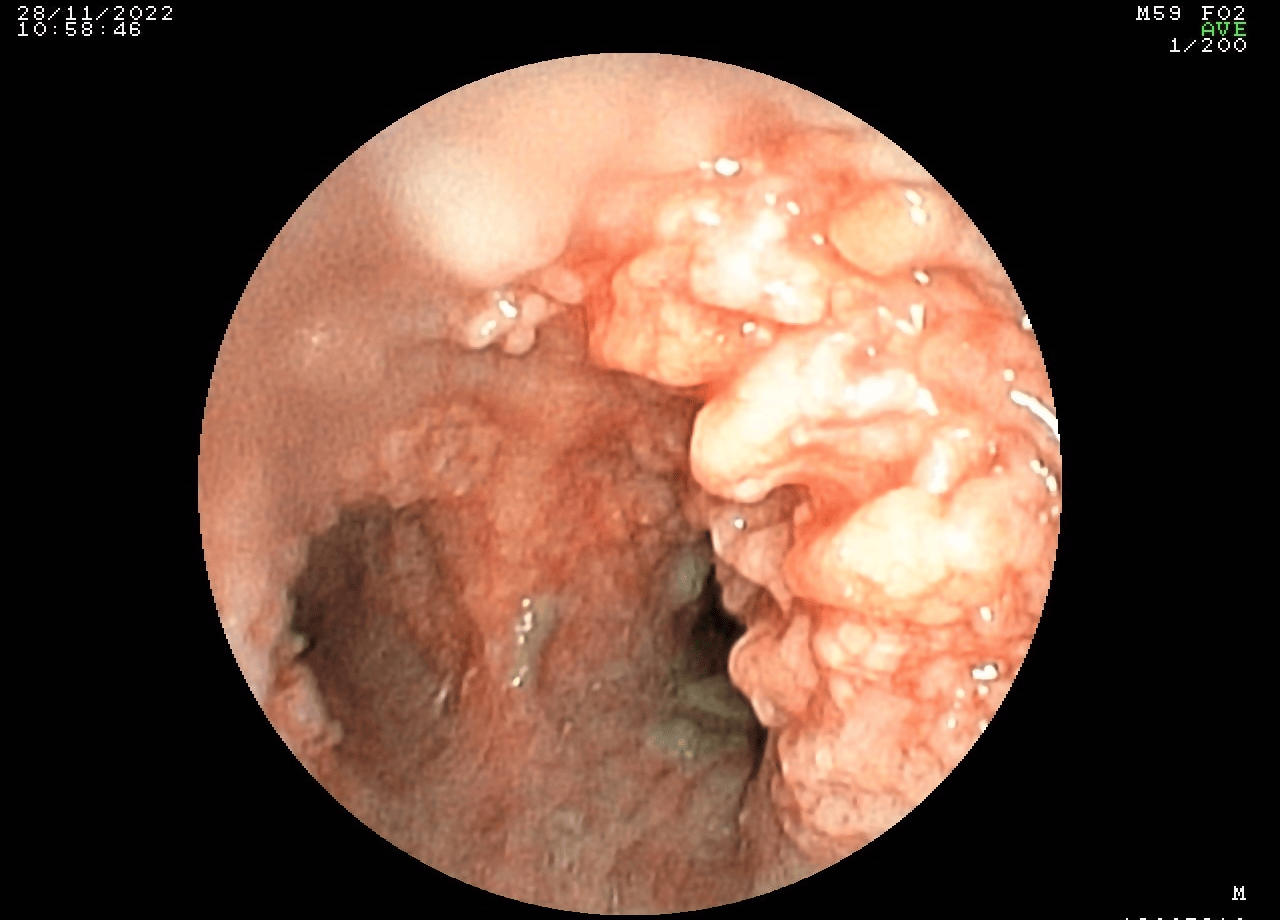
Histological examination of the biopsies reported segments of respiratory epithelium without significant histological alterations or evidence of malignancy.
Fungal culture tests, culture of common germs, and bronchial aspirate smears were negative.
With the diagnosis of osteochondroplastic tracheopathy, the possibility of cryotherapy and argon plasma was explained to the patient.
He reported that the symptomatology was tolerable, so he decided not to undergo further treatment when writing this report.
Case report 3
Male patient RMS, 51 years old, from Casa Grande, La Libertad, Peru, reported a history of throat clearing and pharyngeal pain of approximately three years of evolution. He visited otorhinolaryngology several times. At the beginning of 2020, a diagnostic laryngoscopy was performed, which evidenced a possible subglottic tumor. The patient did not return for check-ups due to the COVID-19 pandemic. In December 2022, he decided to return to otorhinolaryngology due to increased symptomatology. A new laryngoscopy was performed in the unit, revealing granulomatous lesions at the tracheal mucosa. With these findings, he was referred to the neumonology department.
Medical history: in 2018, a foreign body (chicken cartilage) got stuck in his esophagus, which was extracted through endoscopy.
Risk factors: None.
Physical examination: respiratory rate of 16 cycles per minute, pulse rate of 79 per minute, oxygen saturation of 97% at 21% oxygen-inspired fraction, blood pressure 120/60 millimeters of mercury.
Lungs: vesicular murmur in both lung fields. No abnormal respiratory sounds were auscultated. In the rest of the examination, no significant findings were found.
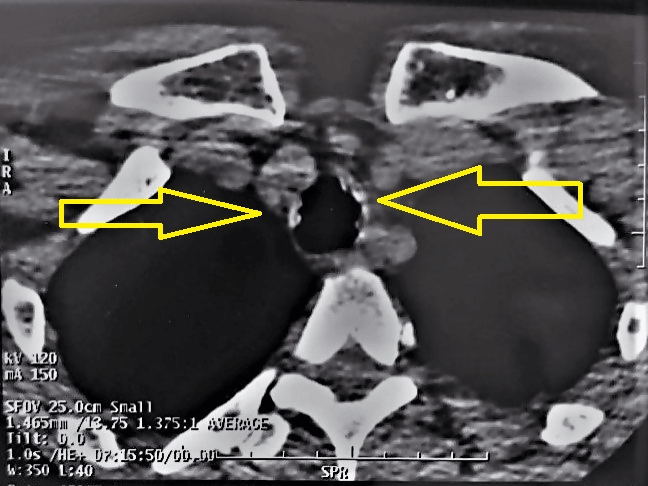
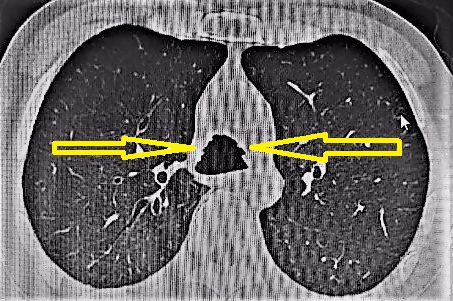
Complementary studies (taken on December 5th, 2022): computed axial tomography of the thorax reported trachea with irregular calcifications, diffuse nodular thickening partially calcified, suggestive of osteochondroplastic tracheobronchopathy (Figure 6).
Computed axial tomography of the thorax showing diffuse tracheal irregular nodular thickening partially calcified (arrows).
Hematology and biochemistry (taken on December 15th, 2022): hemogram, hemoglobin, coagulation profile, glucose, urea, and creatinine within normal ranges.
Spirometry (taken on December 17th, 2022): suggesting a restrictive pattern.
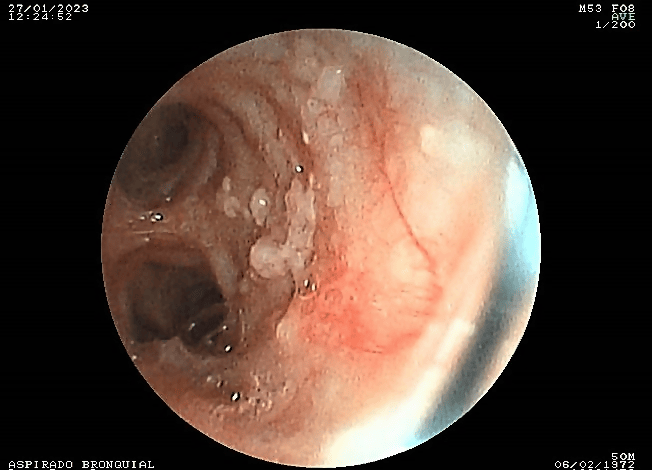
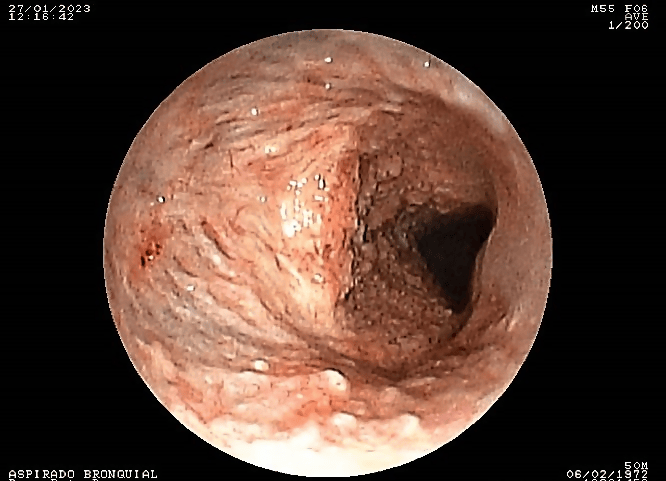
Bronchoscopy was performed, which evidenced abundant whitish nodular lesions of cartilaginous appearance, emerging from the submucosa through the anterior lateral walls of the trachea, without affecting the posterior wall, extending to the right and left main bronchial branches (Figures 7 and 8). Biopsy samples of the tracheal wall, carina, and main bronchi were taken, in addition to bronchial brushing and bronchial aspirate. Histological examination of the biopsy did not find neoplastic cells, but polymorphonuclear cells, lymphocytes, histiocytes, and red blood cells were observed. Bronchial brushing showed edema, mononuclear inflammatory infiltrate, and areas of dystrophic calcification below the respiratory epithelium. Bronchial aspirate examinations for fungal culture, common germs culture, and smear microscopy were negative.
Bronchoscopy video showing granulomatous lesions in the trachea.
Bronchoscopy video showing granulomatous lesions in the main bronchi.
Subsequently, the patient exhibited bronchoconstriction episodes that improved with short-acting beta-adrenergic inhalers using a metered-dose device. With the diagnosis of osteochondroplastic tracheopathy, the possibility of cryotherapy and argon plasma was explained to him.
The patient reported that the symptomatology did not significantly affect his activities. He did not accept the proposed treatments, not ruling them out for the future.
Case report 4
A 59-year-old male patient, VSJ, from Huanchaco, Trujillo, Peru, reported a history of cough for approximately ten years, associated with episodic whitish expectoration. For the last two years, before consulting, the cough was also associated with dyspnea on moderate exertion, throat clearing, and dysphonia, for which he visited several otorhinolaryngologists. He received multiple pharmacological treatments without improvement. Due to the persistence of symptoms, he attended a neumonology consultation.
Physical examination: Respiratory rate of 18 cycles per minute, pulse rate of 82 per minute, oxygen saturation of 97% at 21% oxygen-inspired fraction, blood pressure 110/60 millimeters of mercury.
Lungs: Vesicular murmur in both lung fields and inspiratory wheezing in the right hemithorax.
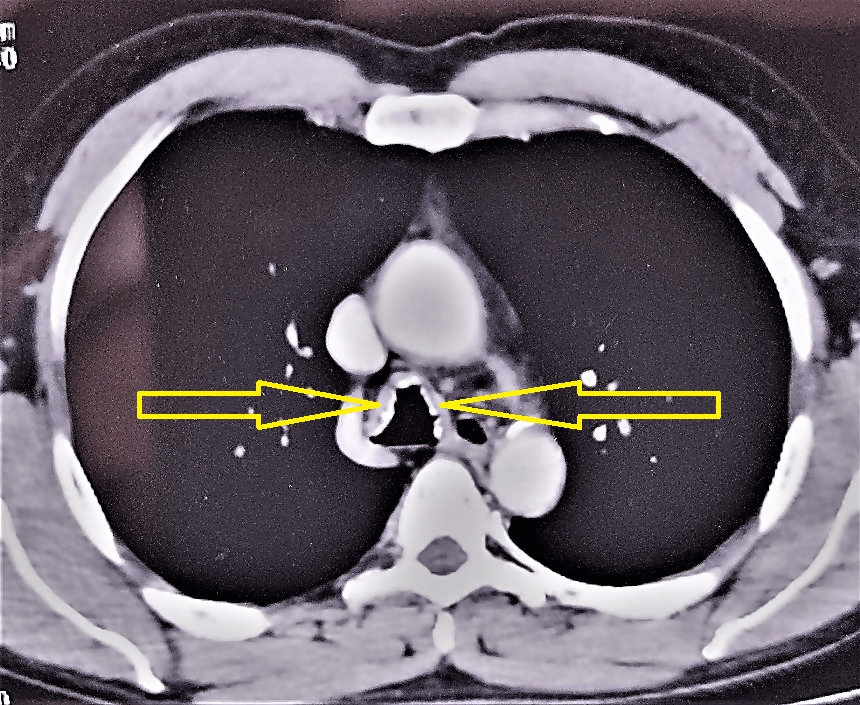
Complementary studies: chest computed tomography scan (taken on December 23rd, 2022) showed diffuse mural calcification with nodular appearances in the trachea and main bronchi without affecting the posterior wall, signs suggestive of osteochondroplastic tracheobronchopathy (Figure 9).
Computed axial tomography of the chest showing nodular calcification in the trachea (arrows).
Spirometry (taken on May 19th, 2023): parameters within normal range.
Diagnostic bronchoscopy demonstrated abundant whitish nodular lesions of cartilaginous appearance, emerging from the submucosa on the anterior and lateral trachea walls, without affection of the posterior wall (Figure 10). The lesions extended to the right and left main bronchial branches, evidencing a 60% decrease in the right main bronchus lumen. Biopsy samples were taken from the tracheal wall, carina, and main bronchi (when sampling the nodular lesions, these were of extremely hard consistency), in addition to bronchial brushing and bronchial aspirate for common germs and fungi. The fungal culture, common germs culture, smear tests, and bronchial aspirate results were negative. Histological examination of the biopsy reported insufficient specimen.
Bronchoscopy video: Whitish nodular lesions of cartilaginous appearance in the trachea.

In subsequent check-ups, the patient had episodes of bronchoconstriction that improved with a short-acting beta-adrenergic bronchodilator using a metered-dose device. With the diagnosis of chondroplastic osteopathy, the possibility of laser or argon plasma therapy was explained to him.
The patient reported that the symptomatology (cough) was tolerable, but he did not accept the proposed treatment due to economic limitations.
Discussion
The diagnosis of osteochondroplastic tracheobronchopathy was not straightforward, given its rarity and non-specific symptoms, which are very common in other pathologies [1]. The low incidence of osteochondroplastic tracheobronchopathy may be attributed to its non-specific symptomatic nature. No case series articles on this pathology have ever been published in Peru. Therefore, we refer to original articles published in other countries as references for our findings.
The pathophysiology is not clearly defined. Several theories exist, such as the role of econdrosis and exostosis of the lateral tracheal rings [16,17]. Metaplasia followed by ossification of connective tissues has also been suggested [18]. Another hypothesis suggests the role of bone morphogenic protein 2 (BMP-2) and transforming growth factor β-1 (TGF β-1) in nodular and new bone formations [19]. A recent study analyzing the genome-wide expression and epigenetics of tracheobronchial basal cells from subjects with and without osteochondroplastic tracheopathy identified the role of these cells in epithelial metaplasia and mesenchymal osteochondrogenesis. This study highlights the dysfunctionality of airway stem cells and the induction of neo-osteogenesis in osteochondroplastic tracheobronchopathy [20].
In our study, the median age at diagnosis was 53 years, predominantly male (75%). This is similar to that found in other publications [21,22,23,24] but different from another case series of osteochondroplastic tracheobronchopathy, where there was no difference in the proportion between males and females [25].
In our cases with osteochondroplastic tracheobronchopathy, the associated symptoms identified were chronic cough, exertional dyspnoea, dysphonia, throat clearing, and pharyngeal pruritus. Chronic cough was the most common symptom, similar to other reports [24,25,26,27,28,29]. We found no link between osteochondroplastic tracheobronchopathy and other inflammatory respiratory diseases, nor did we find any family history in our study, which is similar to that reported in other reports [25].
As in previous studies [25], in 100% of cases, tomographic abnormalities were present. These included submucosal nodules with localized calcifications in the trachea and proximal bronchi. Computed axial tomography is considered the most reliable imaging study to detect osteochondroplastic tracheobronchopathy [30,31,32].
Blood tests and bronchial secretion cultures are not useful and generally tend to be normal or negative [1], as was the case in our patients.
The results of pulmonary function tests are variable, depending on the location and extent of the lesions. Our spirometry results with bronchodilation test showed a normal pattern in 50% and a restrictive spirometric pattern in 50%, in contrast to other series where patients with smoking and chronic obstructive pulmonary disease were included [24,25].
Diagnosis is based on observation of the lesions by bronchoscopy. Biopsies of these lesions can be difficult, mainly due to the hard, stony consistency of the nodules. There is disagreement about the necessity of biopsy for definitive diagnosis [8,33].
The bronchoscopic features of osteochondroplastic tracheobronchopathy are expressed by the presence of numerous cartilaginous and/or bony, whitish cobblestone-like nodules. These nodules can be of different sizes, ranging from 1 to 3 millimeters, located in the submucosa of the tracheobronchial tree, protruding into the lumen and usually respecting the posterior membranous wall [34,35,36]. Our four cases showed typical bronchoscopic features; the lesions were scattered, involving the trachea, and respected the posterior wall. In addition, the proximal bronchi were compromised.
Osteochondroplastic tracheobronchopathy can induce tracheal stenosis in 10 to 27% of cases, sometimes with significant involvement [30,37,38]. In most of them, only symptomatic treatment has been proposed [1,8,34]. In other cases, some authors have proposed surgical treatment with resection, anastomosis, stenting, and laser techniques. In our report, only one case was treated by cryosurgery with a flexible cryoprobe and argon plasma coagulation.
Our study has several limitations, including the small number of cases. We believe that few cases of this entity are identified because it is infrequent and difficult to diagnose [39]. Despite these limitations, our work provides experience in the clinical and bronchoscopic presentation of osteochondroplastic tracheobronchopathy, which may be useful for suspicion, early diagnosis, and management of such a rare condition.
Conclusions
The most frequent clinical manifestations were of laryngeal origin, particularly pruritus and throat clearing. Thus, the cases were initially seen in the otorhinolaryngology department.
The diagnosis of osteochondroplastic tracheobronchopathy is based on typical bronchoscopic features and can be suspected based on computed axial tomography findings.
Given its limited consequences regarding symptoms, pulmonary function, and evolution, it does not usually require specific treatment except for complications.

