Case reports
← vista completaPublished on May 26, 2016 | http://doi.org/10.5867/medwave.2016.04.6453
Squamous cell carcinoma of the conjunctiva with extraocular involvement: case report and literature review
Carcinoma escamoso de la conjuntiva con compromiso extraocular: reporte de caso y revisión de la literatura
Abstract
Squamous cell carcinoma of the conjunctiva is the most frequent malignant tumor of the ocular surface. It is a rare disease with an incidence of 0.13 to 1.9 per 100,000 inhabitants, mainly affecting individuals between 50 and 75 years of age. It tends to have a slow, non-aggressive course. Treatment depends on the extent of the tumor. If there is intraocular involvement, enucleation is indicated, and in the presence of extraocular involvement the orbital exenteration is the standard treatment. We report and discuss the case of an 82 year old male patient having a conjunctival squamous cell carcinoma with intra and extraocular involvement, together with a review of the literature.
Introduction
Conjunctival and corneal tumors represent a wide spectrum of benign conditions such as myxoma, keratoacanthoma or papilloma, and malignant conditions such as squamous carcinoma of the conjunctiva, conjunctival melanoma or Kaposi sarcoma [1].
Squamous cell carcinoma of the conjunctiva is the most frequent malignant tumor of the ocular surface. It is a rare disease with an incidence of 0.13 – 1.9 per 100,000 persons, affecting mainly individuals between 50 and 70 years old and mostly men. It is more frequent in areas near the equator and Africa, where sun exposure is very high which is considered the highest risk factor. Low squamous cell carcinoma incidence in Europe and North America, where people are less exposed to ultraviolet sunlight, supports this idea in the genesis of this disease. The presence of actinic skin diseases, such as solar keratosis and squamous cell carcinoma of the skin have been associated with this as well. Other factors involved are human papillomavirus (HPV) type 16 and 18, human immunodeficiency virus (HIV), exposure to oil derived products, industrial oils and tobacco [2],[3]. While the importance in the pathophysiology of the human papillomavirus is unknown, an association between type 16 human papillomavirus and bilateral conjunctival dysplasia has been reported. In other reports up 77% of cases have had immunochemistry evidence of the virus. Concerning immunodeficiency, it has been estimated that the risk of epithelial malignancies of the conjunctiva is 13 times higher in patients with acquired immunodeficiency syndrome (AIDS). Some authors suggest that at least 50% of patients under 50 years old with conjunctival malignancy might have acquired immunodeficiency syndrome [4]. Kabra and Khaitan, in a comparative analysis detected that patients with human immunodeficiency virus have a more aggressive disease progression and tend to be younger, this suggests that in young patients with a more aggressive ocular malignancy undiagnosed human immunodeficiency virus should be considered [5].
It clinically appears as an exophytic, sessile or pedunculated lesion with superficial vessels that affect the interpalpebral region near the sclerocorneal limbus, but it can affect any area of the ocular globe. It might be confused with benign lesions and delay diagnosis and treatment, therefore suspicion and histopathology study are fundamental [6]. The treatment depends on the extension of the tumor and can include a wide range of possible treatments that can go from topical chemotherapy to orbital exenteration [1].
A case report of a patient with squamous cell carcinoma of the conjunctiva with intra and extraocular involvement is presented here along with a review of the literature.
Case presentation
We present an 82 year-old patient with no clinically significant medical history that reports three months of an exophytic lesion of 3 cm in diameter in the right eye, painless, with no bleeding. It presents a progressive growth and covers a big part of the anteromedial surface of the ocular globe involving the conjunctive and medial border of the cornea. The examination reveals isochoric pupil, absence of proptosis, normal ocular motility, normal intraocular pressure (9-10 mmHg) and appropriate visual acuity for that age. Oral cavity does not present any damage, no palpable preauricular or cervical lymphadenopathy. The ophthalmology team preformed an incisional biopsy with a topical anesthesia. The pathology reports conjunctival mucosa infiltrated by squamous cell carcinoma moderately differentiated, pigmented. The head and neck oncological surgery team evaluated the patient and an orbital magnetic resonance is requested. The results reveal an 11x6x12mm right preseptal orbital tumor adjacent to the medial rectus muscle, with no neighbor adipose tissue or retrobulbar compartment involvement (Figure 1). A right conjunctival tumor lesion can be observed, that appears to have continuity with the medial rectus muscle (since the apparent extraocular involvement is focal and in the muscle insertion site, it is not unusual that the patient presents a preserved motility; if the compromise was in the muscular body, periorbital adipose tissue or periostium, altered ocular motility and diplopia would be expected).
Cervical ultrasound is requested for staging and it shows no suspicious lymph nodes.
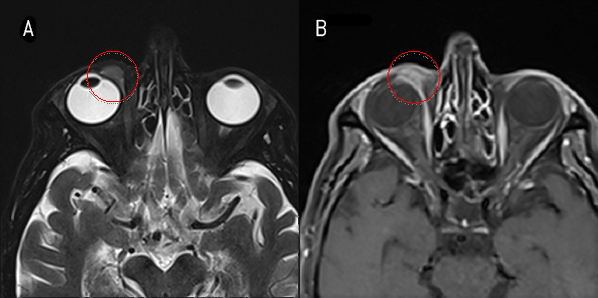
Figure 1. Orbital image with (b) and without contrast magnetic resonance imaging (MRI) (a).
The case is discussed in a meeting with the ophthalmology team and decided to perform surgery with extended enucleation towards muscle tissue, with the intention to preserve the orbital content to facilitate future rehabilitation. The surgery is performed finding an evident macroscopic involvement of the globe (Figure 2).

Figure 2. Right conjunctival exophytic tumor at first evaluation.
Enucleation is performed, with resection of the upper medial periocular tissue, preserving the eyelids. The pathology report informed: squamous cell carcinoma of the conjunctiva poorly differentiated with areas of spindle cell morphology of 2.1 cm larger diameter, with infiltration in conjunctiva, sclera, cornea, medial rectus muscle and superior oblique muscle tendon, with presence of tumoral vascular permeations. All margins were negative at more than 3mm (Figure 3).
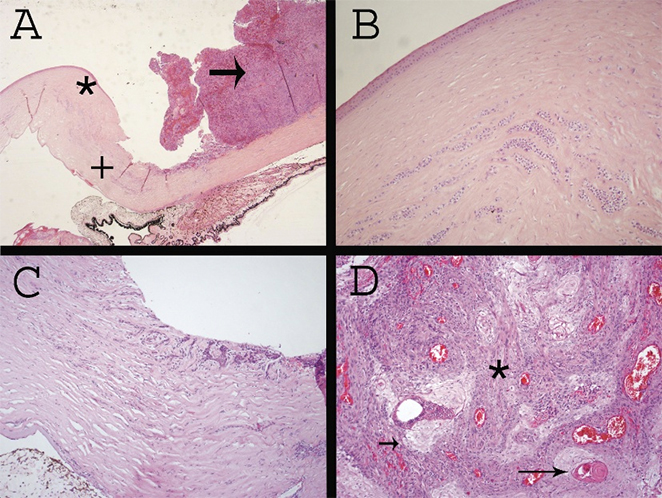
A: Anterior portion of enucleated eyeball sample at 40X.
B: Sample at 200X highlighted with (*) in figure A; infiltration is observed for squamous cell carcinoma in the corneal stroma.
C: Sample at 200X highlighted with (+) in figure A; infiltration of the sclera by squamous carcinoma with extension into the cornea.
D: Sample at 200X highlighted with an arrow in figure A; a solid tumor composed of epithelioid cells with wide eosinophilic cytoplasm (short arrow), keratinized epithelium (long arrows) and spindle cells (*) compatible with spindle cell variant of squamous cell carcinoma.
Figure 3. Microscopy of squamous cell carcinoma of the conjunctiva.
The case is presented to the Tumor Board with the diagnose of squamous cell carcinoma of the right ocular conjunctiva pT4 NO MO. Different therapeutic alternatives are discussed such as orbital exenteration, external radiotherapy or follow-up. The decision to follow-up and a close monitoring is made along with the patient and his family. Five months later a crusty bleeding interpalpebral nodular lesion compatible with tumor recurrence is detected. Orbital exenteration and repair of the defect with a frontal flap is performed. The pathology report showed: squamous cell carcinoma poorly differentiated, with infiltration of connective and adipose tissue, skeletal muscle, tendon structures and upper eyelid. All edges are negative, the nearest one at 3mm. The case is anew presented to the Tumor Board and post surgery radiotherapy is decided. The patient and his family reject this option and continue with follow-up. After 36 months of follow-up the patient is asymptomatic and with no evidence of tumor recurrence (Figure 4).

Figure 4. A later control of orbital exenteration and frontal flap shows no evidence of tumor recurrence.
Discussion
We presented a patient with a squamous cell carcinoma of the conjunctiva diagnose, male sex and old age who presents long ultraviolet sunlight exposure during his working life as the only risk factor.
Squamous cell carcinoma of the conjunctiva is the most frequent malignant tumor in the eye surface. It produces early symptoms associated to problems originated by contact with orbital soft tissues. It normally compromises the sclerocorneal limbus area affecting only at a superficial level; this makes it easy to recognize it. However, it can advance compromising the whole bulbar conjunctiva and later extent through the orbital septum invading the orbital globe or the sclerocorneal lamina penetrating the eye globe [7]. In our case the tumor is located in the most common area of the eye, however the patient consulted at an advanced stage to the hospital probably because of his rural condition.
Differential diagnoses include: 1) benign epithelial tumors, squamous papilloma and pseudoepithelial hyperplasia, 2) precancerous epithelial tumors, actinic keratosis and intraepithelial malignancy, 3) other malignant epithelial tumors, mucoepidermoid carcinoma, 4) benign melanocytic tumors, congenital or acquired nevus, ocular melanocytosis and secondary acquired melanosis, 5) precancerous melanocytic tumors, nevus with atypia and primary acquired melanosis, 6) conjunctival melanoma, 7) other soft tissue tumors and adjacent tissues such as the caruncle, haemangioma, lymphangioma or Kaposi sarcoma [6].
Intraocular invasion is infrequent affecting between 2 and 11% of cases. The spindle cell and mucoepidermoid are the most aggressive variants with a tendency to penetrate intraocular structures as it is shown in this case. The adenoid variant is even more aggressive with intraocular invasion and distant nodal metastasis [8]. It is morphologically important to have a differential diagnosis with the sebaceous carcinoma [9]. If it is required, immunohistochemical techniques can be used against BRST-1 or BER-EP4, which are positive in the sebaceous carcinoma and negative in the squamous carcinoma [10]. The presence of pigmentation in the lesion should lead to think of a melanoma, this was discarded.
Distant metastatic disease is rare (1%), but it can affect regional lymph nodes (preauricular, submandibular and cervical) [7],[8]. The dissemination study should be oriented towards the involvement of regional lymph nodes; in our case we performed it with staging cervical ultrasound without detecting any suspected metastasis lymph nodes. We did not find any reports of sentinel lymph node, however, due to the low frequency involvement of lymph node, the study seems to have a low efficiency.
The TNM classification [11] allows a proper characterization, however there is no staging.
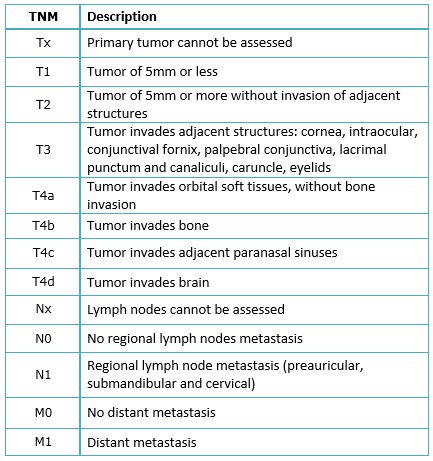
Table 1. TNM classification of conjunctival carcinoma (American Joint Committee on Cancer 2010).
Treatment depends on the extension of the disease at diagnosis, there is a full range of different alternatives [6],[8],[12]. Surgical excision is the chosen treatment in early lesions. Excision success depends on the margin involvement, a surgical margin from 2 to 3 mm is recommended. Recurrence with free margins is from 5 to 15% compared to 50 to 60% when margins are affected. Cryotherapy uses nitrous oxide and liquid nitrogen to destroy tumor cells and adjacent normal tissue. A combined use of this with surgery reduces recurrence to 0-12.3%. When the cornea or the sclera is involved, keratectomy or deep laminar sclerotomy is recommended.
When there is intraocular invasion the treatment is enucleation, this consists of eye globe resection separating orbital content (muscles and periocular adipose tissue) and removing the orbit after section the optic nerve. It is important to avoid manipulation of the tumor during the surgery, to respect tumor integrity and to keep a rigorous haemostasis; all this to reduce intraoperative dissemination. In cases with orbital invasion the treatment is exenteration, this consists of the resection of the eye globe with the whole orbital content (muscles and periocular adipose tissue) with or without preserving the eyelids. In general, when the palpebral conjunctiva is not invaded by the tumor, preservation of the eyelids is safe [13].
Topical chemotherapy with mitomycin c/5 FU / interferon alpha 2b has been used as a primary treatment for dysplasia and carcinoma in situ. It has also been used as adjuvant treatment with the invasive carcinoma after surgical excision or in case of recurrence. With the purpose of preserving the eye globe, Interferon alpha 2b has been used with the invasive carcinoma obtaining good results, but with a short term monitoring. Nanji et al. [14] compared the results of surgical treatment (local resection) versus treatment with drops and/or intraconjunctival injection of Interferon alpha 2b in patients with squamous cell carcinoma of the conjunctiva. Most of patients had T3 tumors (American Joint Committee on Cancer) and after one year follow up they did not find any difference in recurrence, therefore supporting the non-surgical treatment.
Radiotherapy has been historically used as an adjuvant treatment as an alternative to surgery or as palliative care [15]. Many different radiotherapy treatments can be used with this pathology. The use of brachytherapy allows a precise treatment highly focused on the target with a low radiation exposure for the surrounding organs at risk [16]. The use of brachytherapy has been described as an adjuvant treatment to control microscopic disease by using strontium-90 and Ru-106 [17],[18],[19], with local control rates higher than 90%. In cases with orbital invasion, diffuse disease, incomplete resection and multiple recurrences, the use of brachytherapy with isotopes such as Sr-90, I-125 or Ru-106 has been described with good results in terms of local control as an alternative to surgery [20],[21]; with a recommended dose of 6000 cGy.
Due to the low incidence of this pathology along with the concern about the possibility of ocular tissue damage, the use of external radiotherapy with photons [22] and most recently with protons [23],[24] as an adjuvant treatment or alternative to surgery has been reported in the context of institutional series and case reports. This is why postoperative radiotherapy indication is not totally accepted in patients with orbital and intraocular involvement with free margins. Several series have reported good results only with surgery. Tunc et al. [4] in a descriptive retrospective series did not find any recurrence in enucleated or exenterated patients after an average follow-up of 56 months. McKelvie et al. [25], in a retrospective series, found a local recurrence and a cervical lymph node in seven patients either enucleated or exenterated ones, after an average follow-up of 26 months. Gökmen Soysal et al. [26], also, in a retrospective series of patients with orbital involvement did not find any trace of recurrence or mortality associated to the disease after an average follow-up of 36.2 months. Other series, with a low number of patients as well, have supported the use of external radiotherapy with photons or electrons in the case of multiple recurrence or the presence of poorly prognostic factors such as: local advanced disease, perineural invasion or surgical margins involvement. Hsu et al. [22], in MD Anderson Cancer Center described the feasibility of this treatment in 20 patients with an average follow-up of 20 months, no presence of local recurrence was detected; 13 patients presented dry eye syndrome, three patients presented keratinization of the conjunctiva and four patients presented trichiasis, blepharitis, radiation retinopathy and keratopathy respectively. Since there are not any comparative series (patients treated with and without adjuvant therapy), the real value of these factors and recurrence risk in a context of exenteration surgery remains still undetermined [27].
In our case, in spite of complete resection with free surgical margins, we detected early local recurrence; orbital exenteration was required achieving disease control heretofore. This supported aggressive surgery in the presence of extraocular involvement at the time of diagnosis.
Conclusion
Squamous cell carcinoma of the conjunctiva is a low incidence condition. It usually has a less aggressive and slow course. Its treatment depends on the tumor extension. In cases of intraocular involvement enucleation is indicated. Some other non-surgical therapies are still under evaluation with poor follow-up. In case of presence of extraocular involvement, orbital exenteration is the standard treatment. Due to limited available information in locally advanced cases, adjuvant therapies must be considered by a multidisciplinary team along with the patient.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The patient signed the consent form requested by Medwave and a copy was sent to the Journal editorial board.
Conflicts of interest
The authors completed the ICMJE declaration of conflicts of interest and declare they have not received funding for the completion of the report; have no financial relationships with organizations that may have interests in the article published in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or editorial direction of the Journal.
Funding
The authors declare no external funding sources for this study.

