Estudios originales
← vista completaPublicado el 4 de octubre de 2022 | http://doi.org/10.5867/medwave.2022.09.2536
Factores asociados a complicaciones por COVID-19 en trabajadores hospitalarios: estudio de cohorte retrospectivo
Factors associated with complications from COVID-19 in hospital workers: A retrospective cohort study
Abstract
Introduction SARS-CoV-2 infection in healthcare professionals represents a threat to the healthcare system.
Objectives To identify factors associated with complications from COVID-19 in healthcare workers infected by SARS-CoV-2, in a specialized national hospital level III in Peru in 2020.
Methods This is a retrospective cohort study. Health personnel who were working at Instituto Nacional Materno Perinatal of Peru participated. The clinical and epidemiological characteristics and results of the Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) test were collected from the medical records and epidemiological files. Simple and multiple regression models were used to estimate the risk factors of complications due to COVID-19.
Results We found 1048 suspected cases, and 26.2% had a confirmed SARS-CoV-2 infection. Of those infected, 20.8% had comorbidity, and 55% reported contact with COVID-19 patients in health care settings. Moreover, 27.4% of infected workers were administrative personnel, 24.1% were nursing technicians, 18.3% were nurses, and 13.1% were physicians. We also found that 24.1% presented complications from COVID-19, and three workers died. In a multiple regression, the risk factors for complications due to COVID-19 were the presence of comorbidity (risk ratio: 2.94; 95% confidence interval: 1.95 to 4.42), 30 years or older (1.28; 0.6 to 2.75), 60 years or older (2.04; 0.88 to 4.74), male sex (1.1; 0.71 to 1.7) and care work area (1.02; 0.06 to 2.62).
Conclusions The findings in the present study show an association between the presence of comorbidities and an increased risk of presenting complications due to COVID-19 in healthcare workers, regardless of age, sex and area of work.
Main messages
- SARS-CoV-2 infection in workers represents a threat to the health system.
- This study’s results will help identify vulnerable personnel to prevent severe forms of the disease by taking the corresponding isolation measures.
- Some of the limitations of this work are the collection of information from medical records, not having direct contact with the patient or access to the viral load for its association with the complications analyzed in this study.
Introduction
The COVID-19 disease became an occupational disease of healthcare workers [1] due to the increased risk of exposure to SARS-CoV-2 in healthcare facilities [2,3] compared to the general population [4].
In the Americas region, an accelerated increase of infections and deaths due to COVID-19 in health personnel was found in 2020 [4]. In Peru, 61 808 confirmed cases had been reported among health care personnel, with a mortality rate of 2% [5]. The COVID-19 pandemic is a global health emergency, and the capacity to respond to this crisis consists mainly of ensuring the continuous provision of health services [2]. Health personnel is fundamental to its functioning [4]. Consequently, SARS-CoV-2 infection in workers represents a threat to the health system [6].
Like in the general population, COVID-19 infection in healthcare workers can be asymptomatic or oligosymptomatic, and its complications occur in a low percentage of cases [7]. For this reason, early diagnosis, identification of complications, and appropriate management are essential to decrease COVID-19 mortality [8].
This study aimed to identify factors associated with complications due to COVID-19 in healthcare personnel with a real-time polymerase chain reaction test (RT-PCR) who worked in a third-level care institute in Peru in 2020.
Methods
Study design and setting
This is a retrospective cohort study conducted at a tertiary care hospital of the Ministry of Health of Peru named Instituto Nacional Materno Perinatal. In the context of the pandemic, the Instituto Nacional Materno Perinatal performed a real-time polymerase chain reaction test (RT-PCR) for SARS-CoV-2 on all workers with clinical suspicion and epidemiological contact. In addition, institutional protocols were followed to reduce the risk of transmission by implementing differentiated areas for the care of patients with COVID-19 disease.
The target population was healthcare personnel with COVID-19 infection confirmed by a positive RT-PCR test for SARS-CoV-2 that worked at the Instituto Nacional Materno Perinatal between April 1 and December 31, 2020.
Inclusion criteria for this study were:
- Personnel with face-to-face or hybrid (face-to-face and remote) work.
- Personnel with a positive result in the RT-PCR test for SARS-CoV-2.
Exclusion criteria were:
- Health personnel who only performed remote work.
- Personnel who only had clinical and/or radiological criteria suggestive of COVID-19.
- Personnel who only had a rapid reactive IgM/IgG antibody detection test.
SARS-CoV-2 screening test
Workers presenting compatible symptoms and/or direct contact with a suspected or confirmed case of COVID-19 went to the personnel physician’s office. Once the suspected case was identified, the clinical and epidemiological investigation form approved by the Ministry of Health was filled out, and an RT-PCR sample was taken.
Biological samples from health personnel were obtained from pharyngeal and nasal swabs by qualified personnel from the Epidemiology and Environmental Health area of the Instituto Nacional Materno Perinatal. The RT-PCR diagnostic test was used to process the biological samples at the National Institute of Health of Peru to identify the SARS-CoV-2 virus.
Variables
General information of the health personnel was recorded and included age (classified as young, adults, or older adults if workers had between 20 and 29, 30 and 59, and 60 or more years, respectively), sex, professional profile, and work area (administrative and health care). Moreover, we gathered the presence of any symptoms (sore throat, general malaise, fever, cough, headache, nasal congestion, muscle pain, respiratory distress, anosmia and ageusia, diarrhea, chest pain, joint pain, nausea and vomiting, and abdominal pain), and the presence of any comorbidity (arterial hypertension, type 2 diabetes mellitus, bronchial asthma, cardiovascular disease, cancer, rheumatoid arthritis, and HIV). History of travel in the previous 14 days, contact with a suspected case (contact with a person with acute respiratory infection in the 14 days prior to symptom onset), or confirmed case (contact with a person with confirmatory evidence in the 14 days prior to symptom onset) of COVID-19 were also gathered.
The outcome variable was the presence of COVID-19 complications, defined as presenting acute respiratory infection, dyspnea (oxygen saturation less than or equal to 92%), tachypnea, and clinical or radiological signs of pneumonia. In addition, workers requiring hospitalization (including the intensive care unit) and those who died due to COVID-19 were also considered.
Collection of information
Characteristics of the health personnel and the results of the RT-PCR test were obtained by reviewing the medical records of the COVID-19 cases and clinical and epidemiological files approved by the Ministry of Health. The necessary safeguards were taken to guarantee the anonymity of the participants by coding their identity when collecting data from the information sources.
Statistical analysis
Relative and absolute frequencies were used to describe qualitative variables. The Chi-square test was used for the comparative analysis of variables between groups according to the presence of complications. The relative risk with their respective 95% confidence intervals was used for the bivariate analysis of the strength of association. Poisson regression with robust variance was used to identify the adjusted relative risk. The model adjustment considered an epidemiological approach, including sex, age, work area, and comorbidity as the main exposure variables and complications due to COVID-19 as the outcome variable. The analyses were performed using Rstudio software version 4.1.1.
Ethics
The research was approved by the institutional Research Ethics Committee of the Instituto Nacional Materno Perinatal and had the corresponding institutional permission. The identity of the participants was protected at all times using alphanumeric coding. Likewise, Council for International Organizations of Medical Sciences (CIOMS) guidelines were followed for recording and handling the study participants' data.
Results
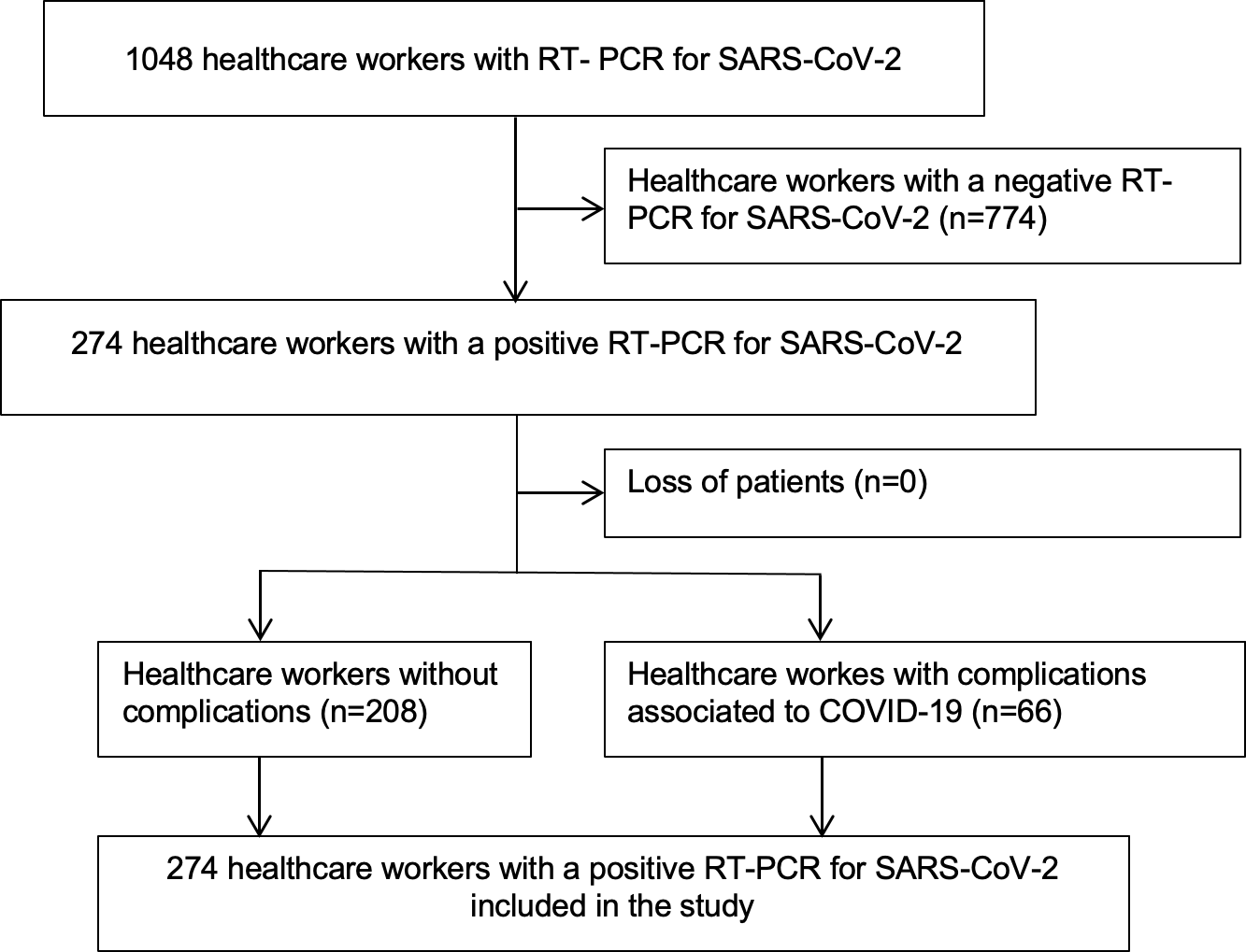
During the study period, 2228 workers were employed at the hospital, and a total of 1048 suspected cases were identified and tested by RT-PCR. Of these, 274 presented a positive result, and 774 had a negative result (Figure 1). A frequency of infection of 26.2% (95% confidence interval: 23.5 to 28.9%) was observed among the suspected cases of COVID-19 in health workers at the Instituto Nacional Materno Perinatal.
Flowchart for the selection of health personnel included in the study.
The first six cases of healthcare personnel with COVID-19 infection were diagnosed in April 2020. In May and June, the number of confirmed cases at the Instituto Nacional Materno Perinatal increased, with 50 and 46 cases, respectively. In July, the highest number of cases was reported, with 77 new cases. During the following months, we saw a decrease in cases, with 50 in August, 18 cases in September, 11 cases in October, and one case in November. In December, there was a new increase in the number of new cases, reaching 15 infected workers in that month.
The most frequent characteristics of health personnel with a positive RT-PCR test were adult age (78.1%), female sex (72.6%), and contact with a person suspected of COVID-19 within the in-hospital setting (40.2%). Fifty-five percent of the infected healthcare personnel worked with patients with COVID-19. Of the infected, 72.3% worked in health care and 27.7% in administrative areas. Among those infected with COVID-19, administrative personnel accounted for 27.4%, nursing technicians 24.1%, nursing graduates 18.3%, and physicians 13.1%. Only 1.5% reported a history of travel 14 days before the onset of symptoms, and all were within the national territory (Table 1).
Among personnel with a positive RT-PCR test, 20.8% (57 cases) had some comorbidity. The most frequent were bronchial asthma in 26 cases (45.6%), arterial hypertension in 23 cases (40.4%), type 2 diabetes mellitus in eight cases (14%), cardiovascular disease in five cases (8.8%), cancer in two cases (3.5%), rheumatoid arthritis in two cases (3.5%) and one case of HIV (1.8%).
Symptoms were present in 95.3% of the personnel with a positive RT-PCR test. The time from symptom onset to sampling for the RT-PCR test had a median of three days (range: 1 to 20 days). The most frequent symptoms were general malaise (66.1%), sore throat (64.2%), fever (64.6%), cough (58%), and headache (51.5%). Other symptoms found were nasal congestion (43.8%), muscle pain (40.1%), respiratory distress (27.7%), anosmia or ageusia (15.7%). With lower frequency, we found symptoms such as diarrhea (12.8%), chest pain (11.3%), joint pain (9.1%), nausea and vomiting (6.2%), and abdominal pain (4%). A total of 24.1% presented some complication associated with COVID-19 (oxygen saturation less than or equal to 92%, clinical and/or radiological signs of pneumonia, or hospital admission), and three died (1.1%) (Table 2).
In the bivariate analysis, the characteristics associated with COVID-19 complications were the presence of comorbidities (p < 0.001), age (p = 0.01) and out-of-hospital contact (p = 0.045). No association was found between COVID-19 associated complications and sex (p = 0.54), work area (p = 0.68) and in-hospital contact (p = 0.595) (Table 3).
In bivariate analysis, the crude relative risk for COVID-19 complications in older adults compared to younger adults was 2.97 (95% confidence interval: 1.21 to 7.30). The crude relative risk for COVID-19 complications in health personnel with comorbidity compared to those without comorbidity was 3.17 (2.15 to 4.67). In the multiple regression analysis, the relative risk of presenting COVID-19 complications in health personnel with comorbidity was 2.94 (1.95 to 4.42) compared to health personnel without comorbidities, adjusted by sex, age, and work area (Table 4).
Discussion
The study showed that 26.2% of workers at the Instituto Nacional Materno Perinatal with suspected SARS-CoV-2 infection had confirmed infection by RT-PCR. We also found that 78.1% presented an age between 30 and 59 years, 20.8% had some comorbidity, and 55% cared for patients with COVID-19. A total of 31.8% worked in hospitalization areas, while 27.7% worked in administrative areas. Of these, 24.1% presented complications due to COVID-19, and three workers died. There was evidence of an association between having some comorbidity and complications due to COVID-19.
The frequency of infection among the workers of the Instituto Nacional Materno Perinatal aligns with other studies in public hospitals in Madrid, Spain [9] and Wuhan, China [10]. These findings also align at a regional level, where similar rates were reported among health personnel in Brazil [4]. In the context of the pandemic, the Instituto Nacional Materno Perinatal established a plan for the surveillance, prevention, and control of COVID-19 at work, following the Ministry of Health guidelines that have been in force since April 28, 2020, and its subsequent modifications [11,12]. In this regard, measures were implemented to identify suspected cases in workers, such as RT-PCR testing for SARS-CoV-2. These measures included the internal spreading of awareness-raising for the prevention of in-hospital infections, emphasizing the importance of hand washing, the mandatory use of masks, social distancing, and early reporting of COVID-19 symptoms. These measures were supervised by the respective service, department, and area managers. In addition, there was strict supervision by the Office of Epidemiology and Environmental Health of the Instituto Nacional Materno Perinatal.
It was evident that the number of confirmed cases at the Instituto Nacional Materno Perinatal followed the trend of the COVID-19 wave at a national level [5,13]. Many of the infections in health personnel occurred in our country’s early pandemic stages. It was observed that a similar proportion of infected workers confirmed contact both within and outside the hospital. This suggests considering the risk of personnel exposure in other environments outside the institution. For this reason, the exposure of health personnel cannot be attributed to the work area alone, which limits the possibility of evaluating the impact of nosocomial versus community-acquired infection.
The study reported 12.2% of COVID-19 infections in healthcare workers at the Instituto Nacional Materno Perinatal for the study period, in contrast to other studies where they represent approximately 1% [10,14,15], which can be explained by the different criteria considered to perform an RT-PCR test. Other studies only apply swab sampling to symptomatic patients, while our institution also included workers who reported direct contact with a suspected or confirmed case of COVID-19. The predominantly affected population were female adults between 30 and 59 years of age, which is compatible with the majority of sociodemographic findings in health personnel in different parts of the world [10,14,15,16,17,18] since most of the personnel working in the institution fall within this demographic profile.
Workers in hospitalization areas and those who provided care to COVID-19 patients represent the majority of infected personnel, consistent with other reports indicating that more than half of the affected personnel work in the direct care of patients with COVID-19 [10,16]. Although cross-infection in the same institution cannot be excluded, it is unlikely that this situation explains most of them.
Among care staff, the most affected were nursing technicians, followed by nursing graduates and physicians. In contrast, multiple studies point to nurses as the most affected occupational group [10,17,18]. Other authors also highlighted high rates of infected support staff [4,14,19]. This situation may be explained by the greater amount of time they devote to direct patient care. However, administrative staff accounted for the highest number of COVID-19 infections among healthcare workers. This proportion may be attributable to different reasons, such as community infection or air recirculation in enclosed spaces. Likewise, the healthcare personnel’s compliance with biosafety measures is higher due to the high risk of exposure in patient care. Administrative personnel maintains constant contact so that someone with SARS-CoV-2 infection who worked at their site 48 hours prior to the onset of symptoms could have been a source of infection for others [20]. Thus, the difference found has necessary implications for reformulating policies to reduce this infection among workers.
In the present study, we found that 4.7% of healthcare personnel with SARS-CoV-2 infection were asymptomatic. The existence of these patients puts the health of the rest of the staff at risk, so it is vital to identify and isolate them to prevent disease spread. To a large extent, COVID-19 infection in healthcare personnel was oligosymptomatic. Like most international papers reported, the main symptoms found were general malaise, sore throat, fever, and cough [10,14,16,16,19,21]. Although anosmia and ageusia were considered specific symptoms, these were reported only in 15.7% of workers. The time from symptom onset to treatment initiation was three days, which is shorter than the general population [21]. This is similar to publications reporting the prioritization of health personnel for testing compared to the general public [22].
On the other hand, 57 healthcare workers with COVID-19 had some comorbidity. Multiple studies indicated that the most frequent comorbidities were arterial hypertension, chronic obstructive pulmonary disease, type 2 diabetes mellitus, and other cardiovascular diseases [10,17,19,22]. Likewise, our findings showed that a quarter of the workers developed complications due to COVID-19. These complications manifested as oxygen saturation less than or equal to 92%, tachypnea, and clinical and/or radiological signs compatible with pneumonia. Other studies also report similar findings [10], but there are no precise data on this situation for health personnel in our country.
Under a bivariate analysis, COVID-19 complications were associated with the presence of comorbidities and being 60 years of age or older. Likewise, adjusting for age, sex, and work area, the relative risk of presenting complications associated with COVID-19 in health personnel with comorbidity was 2.94 times compared to personnel without comorbidities. These findings differ from other studies where no such association was found in health personnel [10,17].
The Center for Disease Control and Prevention notes that most of the deaths registered in health personnel in the United States had some comorbidity [19]. The Ministry of Health also identifies certain conditions that determine a higher risk of dying from COVID-19, where an age over 65 years stands out [21]. Three workers at the Instituto Nacional Materno Perinatal died from complications of this disease. The three deceased were 65 years or more, while only one of them was a healthcare worker. Other studies have shown that the case fatality rate is lower in this occupational group [10,23] compared to 4% in the general population [21]. Although severe forms of COVID-19 disease do not represent the majority of cases, our study showed that more than half of all infected workers with some comorbidity developed complications due to COVID-19.
These findings emphasize the risk of complications in those with some comorbidity, so it is crucial to assess the worker’s health status to determine the modality of work of personnel in vulnerable situations and maintain permanent surveillance of the worker’s health in the context of COVID-19 [11].
The limitations of this study include that workers' information was collected from records and not from direct contact (including medical records and a report of confirmation of COVID-19 infection) and not having access to the viral load for its association with the complications analyzed in this study.
Conclusions
We found a significant association between the presence of comorbidities and having SARS-CoV-2 complications. The most frequently reported comorbidities were bronchial asthma, arterial hypertension, and type 2 diabetes mellitus.
The Instituto Nacional Materno Perinatal was not exempt from caring for COVID-19 patients or COVID-19 infection in health personnel. For this reason, the strategy should focus on reducing SARS-CoV-2 transmission in the hospital setting.
Our study recommends improving awareness and response capacity to reduce the impact of morbidity and mortality in healthcare personnel in the face of a possible new COVID-19 pandemic wave. To this end, the identification of comorbidities in workers is relevant. Likewise, it is necessary to reinforce training and awareness regarding strict compliance with biosecurity measures and individual supervision.

