Estudios originales
← vista completaPublicado el 3 de enero de 2023 | http://doi.org/10.5867/medwave.2023.01.2627
Barreras para las actividades de investigación en los programas de residencia: estudio de métodos mixtos
Barriers for research activities in residency programs: A mix-methods study
Abstract
Introduction Research activities have a positive impact on the performance of residents. However, information on research conducted by residents from developing countries is scarce. Our study sought to identify the barriers and facilitators for developing research in medical residency programs in a Latin-American faculty of medicine.
Methods A mixed methodology study design was carried out. We used a grounded theory approach for the qualitative phase, collecting data through semi-structured interviews and focus groups with faculty and residents. For the quantitative phase, surveys were administered to residents and teachers. We used factor analysis and scree plot (validity), Cronbach's alpha, and Intraclass correlation coefficient (reliability) to evaluate the surveys' psychometric properties.
Results Focus groups involving ten faculty members and 15 residents were conducted, and the following domains were identified: a) facilitators for resident participation, b) barriers, c) strategies for introducing research into the curriculum, d) arguments supporting research activities throughout medical residency, and e) profile of research-motivated residents. Both residents and faculty members identified a lack of protected time and adequate mentoring as the major barriers. A gender gap was found related to international publications (34% vs. 66% women/men); women perceived that research activities 'compete with other activities' (OR: 2.04, 95% CI 1.03 to 4.07).
Conclusions Research is highly valued by both residents and faculty members at a Latin-American university with a strong academic output. Major barriers to promoting research in this context include lack of protected time and effective mentoring, and gender gaps. Strategies proposed to improve research within medical residency programs include: establishing an interdisciplinary mentoring program between residents and researchers, promoting elective rotations, and rewarding proposals that consider gender equity.
Main messages
- Residents and faculty members in a Latin-American faculty of medicine highly value research during the residency program.
- The main barriers to developing research include gender gaps, lack of mentoring, and protected time.
- We propose establishing interdisciplinary mentoring programs and rewarding proposals that promote gender equity and women's participation to strengthen medical residency research in Latin America and developing countries.
Introduction
Research-related activities can improve residents' clinical care, critical thinking, and lifelong learning [1]. Recent studies have highlighted an alarming decline in the number of medical researchers and, consequently, have called for more effective strategies for promoting the incorporation of research into education curricula and medical training [2]. Postgraduate agencies such as the Accreditation Council for Graduate Medical Education [3] in the United States of America and the Royal College of Physicians and Surgeons of Canada [4] mandate the inclusion of basic clinical research principles in their residency programs, and provide the necessary resources to facilitate their participation, thus guaranteeing the participation of residents in research activities. Medical residency programs have adjusted their curricula to meet these requirements, with varying levels of productivity and satisfaction [5,6]. Residents may encounter several barriers to conducting research, including personal, logistical, and organizational barriers. Studies in Europe and the United States have used specific surveys to identify barriers and facilitators to research development by residents [7,8,9,10,11]. Others have studied this issue using a qualitative approach in specific medical residency programs [12,13], but without approaching the issue from a perspective that considers the diversity among different medical residency programs.
Previous studies [14,15] have reported low percentages, with high heterogeneity of publications in international journals by undergraduate students in medical schools in low- and middle-income countries. However, specific reports on barriers and facilitators to research in Latin American medical residency programs are still lacking.
Our study explored how residents are introduced to or participate in clinical research during training using a mixed methodology in various medical residency programs. We also sought to record the perceptions and beliefs of residents and faculty regarding barriers and facilitators to conducting research activities in medical residency programs. Our study was based on a LatinAmerican faculty of medicine with a high research output. To our knowledge, this report is the first of its kind.
Methods
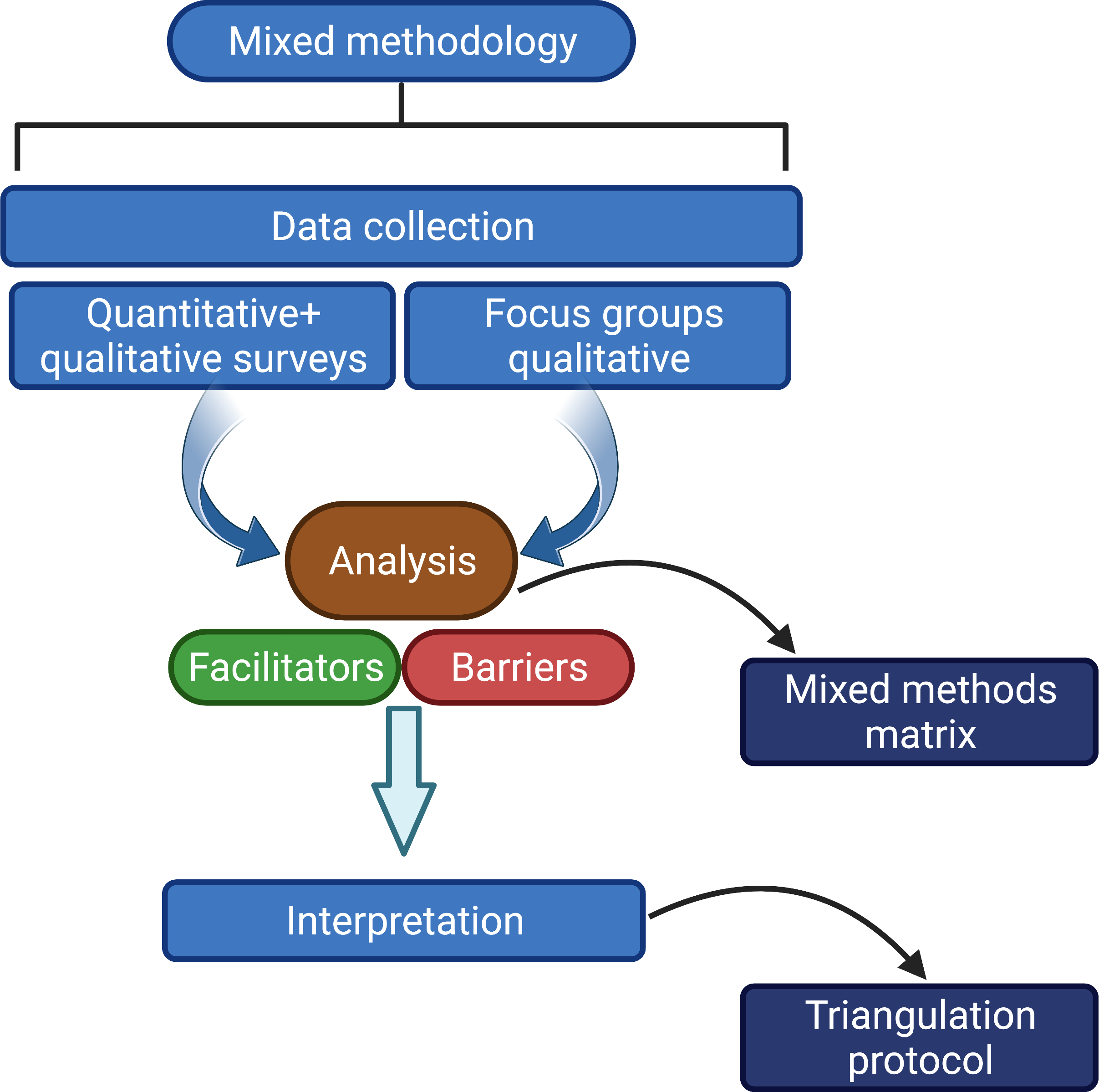
The present study was conducted at the Residency Programs of the School of Medicine of the Pontificia Universidad Católica de Chile (PUC). It was performed following national and international standards and the Declaration of Helsinki. It was approved by the Clinical Ethics Committee of the Faculty of Medicine with the number 181229001. We used a mixed-method research design to expand the understanding of barriers and facilitators for research activities (Qualitative phase) and to propose a systemic approach to research across a wide range of medical residency programs (Quantitative phase). Residents, faculty members, and research and postgraduate directors were invited to participate. Figure 1 shows the research methodology.
Methodology design.
Qualitative methodology
We used a qualitative, exploratory study with ethnographic intent [16,17] to generate the theory of a social phenomenon and better understand the data obtained [18]. The participants were residents, faculty members from different programs, and authorities of the Pontificia Universidad Católica de Chile faculty of medicine. The qualitative phase was by purposive sampling, where the best informants were selected to collect rich data to address the study question. Invitations were sent to faculty members among those with the highest research productivity (estimated by the number of recent 5-year H-index publications) and residents from different programs who had applied for intramural research grants.
We conducted semi-structured interviews with selected authorities of the postgraduate department of the faculty of medicine of the Pontificia Universidad Católica de Chile. Additionally, focus groups were conducted with representatives of residents and faculty members.
First, an in-depth semi-structured interview was conducted with the faculty of medicine's research and Ph.D. program director. Then focus groups with residents and faculty members were carried out, including representatives of the research and graduate offices. The focus groups were guided using a semi-structured guideline (supplementary material) built up from characteristics that impact residents' academic productivity [19].
The principal investigator (TM) and a psychologist (VR) with qualitative research experience conducted focus groups of ten to fifteen participants to facilitate interaction. Each group lasted about 90 minutes and was recorded and transcribed. Focus group results were confidential, and all participants signed an informed consent approved by the research ethics committee.
Data were analyzed using a theory-based methodology [20], and coding was open-ended with constant comparison until sample saturation. Atlas.ti® software was used for efficiency and consistency. Quality control of the results was performed according to Ruiz [21].
Quantitative methodology
Two surveys were designed based on the qualitative data examined in this study and previously reported surveys [22,23] were used to identify potential barriers and facilitators to research among residents. The surveys were designed to represent the five dimensions (categories) of the barriers and facilitators for research activities in residency programs identified in the qualitative section (see the qualitative results section). One survey was created for faculty members and the second (partially different) for residents (supplementary material). Both surveys included five domains: (1) demographic and productivity characterization (presence or absence of national and international publications), (2) value of research in medical residency (Likert scale of one to five for eight statements related to research), (3) barriers to research scale, from one (most relevant) to five (least relevant), (4) priority areas for training (Likert of one to five for topics to include in research training for residents) and (5) preferred forms of participation (multiple-choice-question type).
A pilot study involving ten faculty members and residents was carried out to test the preliminary version of both surveys, in which the participant’s were asked if the questions were clear. In addition, the participants’ responses were reviewed to determine if any questions were left blank or if the same answer was used repeatedly for each question. The surveys were sent by email as an attachment to the administrative assistants of the participating medical departments to be printed out and given to faculty members and residents; after that, twice-weekly reminders were made. After this period, the first author collected and entered the surveys. We also sent the same survey using SurveyMonkey® to the database of faculty members and residents at the faculty of medicine; this software automatically enters the collected data. There were no differences in blank response patterns between the two application formats. In both conditions, confidentiality was guaranteed.
First, we used exploratory and confirmatory factor analyses to identify possible latent factors [24,25]. We used the Cronbach alpha coefficient [26] and the consistency of agreement among means intraclass correlation coefficient, considered homologous to Cronbach's alpha, to assess internal consistency [27]. A Fisher exact test was used to compare the productivity ratios of publications. Contrasts are expressed as medians and interquartile range (IQR: p25 to p75), and statistical differences were analyzed using the Mann-Whitney non-parametric test. We built univariate ordinal regression models to assess the association between each perceived barrier (dependent variable in Likert-type format) and gender. Odds ratios with 95% confidence intervals (95% CI) were calculated. Since the female gender was taken as a reference, an OR greater than 1.0 represented that the men rated a particular barrier as less important. A multivariate ordinal regression model was estimated, including age and grade (academic or resident) as covariates.
We used the triangulation protocol described by O’Cathain [28]. Information obtained from focus group interviews and surveys was triangulated and carried out with three analysts' participation until it was considered saturated after an exhaustive review of the sources.
To apply the triangulation technique, we developed a convergence coding matrix showing the contribution of the qualitative and quantitative methodology to exploring barriers and facilitators for research. Those that presented partial coincidence appeared in the discourse of two referents. Those called silence were mentioned only by one of the parties concerned.
Results
Qualitative analysis
Ten faculty members (four of them female) from various residency programs participated in our first focus group. Our second focus group included fifteen residents across different areas (a single female participant). Our analysis identified five key areas that contained a variable number of categories:
-
Facilitators for research activities performed by residents.
-
Barriers to research activities by residents.
-
Inclusion elements suggested by residents.
-
Principles supporting the inclusion of research actions in resident training programs.
-
Characterization of the resident interested in research
Additional information, including quotes from each focus group and interviews, can be found in supplementary materials (online supplementary tables 12).
Faculty members frequently mentioned good mentorship as a key facilitator for the resident's research. "Having mentors to help with each phase of the research, with the construction of the research question, with the methodology to be used…." Residents also highlight the importance of mentors; in their own words, "If we have any questions, we have direct access to the staff. They include us in the research, and they are present". A research director adds, "Mentors who can bring their expertise so that motivated residents can, over time, develop their ideas."
Another critical facilitator is having protected time for research; faculty members confirm that "when faculty have protected time, residents understand that they have a space for that research" Residents indicate that "we have one or two months protected exclusively for research … that protected time gives us time for research design and implementation…", while the research director states that protected time for research... "Is part of the normal dynamics of researcher's practice …. … just as the university president has to have it...the resident has to have protected time".
A third key facilitator is having a curricular structure for research. One faculty member states that "having a mandatory structure for research with agenda, Gantt chart, time tutors, deadlines… I would summarize in that word structure." Residents added, "now residents have research classes, project development, taught by researchers working within the same service…. the motivation for residents to attend was greater". The research director also agreed, "…. Is no longer something that happened all of a sudden... structurally, it is set up where to acquire certain skills, it is necessary to research and know that it will be evaluated."
Quantitative results
Forty-five faculty members from 20 departments completed the survey; twenty-six (59%) were male. Sixty-five residents from twenty-one departments completed the survey; thirty-two (49%) were female. Further information is detailed in Table 1 and the supplementary material (online supplementary table 3).
Participants' self-reports through anonymous questionnaires
Gender, academic category, age, and academic/resident status were associated with the number of national and international peer-reviewed publications. Most participants without international publications were female (55.6%), under 40 years old (96.3%), medical residents (87%), or faculty members in the “instructor of medicine” category (85.7%). Additional information, including exploratory factor analysis, sedimentation graphs, confirmatory models, and differences in each item comparing residents and faculty, are shown in online supplementary tables S4-S8 and online supplementary figure 1.
Confirmatory factor analysis demonstrated that this scale is a unidimensional instrument. The confirmatory model estimated coefficients of determination (R2) between 0.04 and 0.69. Cronbach’s alpha reliability coefficient was 0.77. Both faculty members and residents highly value research, with responses ranging between four and five points in 8/8 and 6/8 items. There were significant differences between the evaluations made by faculty members and residents. Faculty members' evaluations (median: 4.5; IQR 4.1 to 4.8) were higher than residents (median: 4.1; IQR 3.6 to 4.6).
Given that the scale used in this domain conditioned subsequent responses to previous ones, applying a factor analysis or an estimated scree plot was not considered appropriate. Instead, content and sample validity were ensured by evaluating eight and nine barriers described in the literature in faculty members and residents, respectively. The intraclass correlation coefficient was 0.93 (0.85 to 0.99) and 0.97 (0.92 to 0.99) for faculty and resident surveys, respectively.
For faculties, the main barriers were: lack of protected time, lack of research funding, and competition with other activities (clinical work, study, and family), whereas for residents main barriers were: lack of protected time and competition with other activities. Figure 2 compares residents with faculty; the only significant difference found was that residents deemed the absence of research-trained residents more important than faculty members.
Perceived barriers to research. Participants scored each item using a 6-point Likert scale ranging from one (most important) to six (least important).
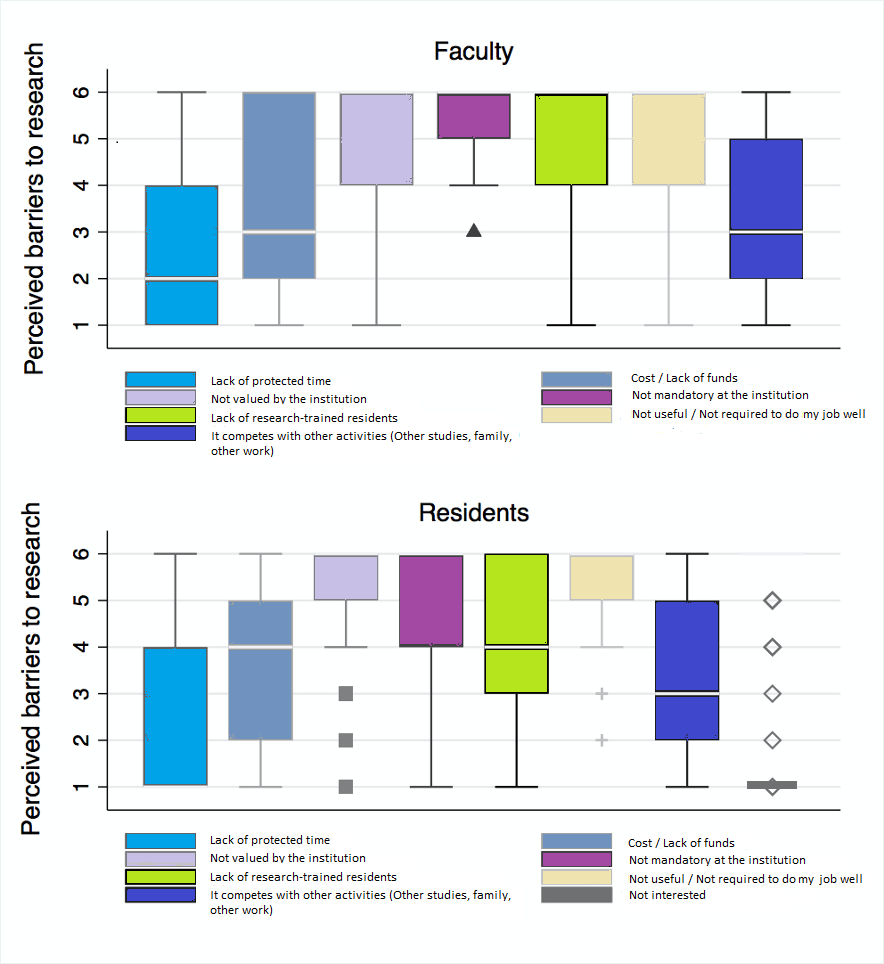
Analyzing our findings by gender, we found significant differences in two barriers: “It is not mandatory for the institution” and “it competes with other activities (other studies, family, other work)” (Table 2). The “It competes with other activities” barrier was less relevant for males (OR = 2.04 95%CI 1.03 to 4.07). Gender was also significantly associated with the abovementioned barrier after adjusting by age and academic status (resident or faculty).
Confirmatory factor analysis showed that this scale is a unidimensional instrument with good internal consistency (Cronbach’s alpha was 0.78). The questions with the highest standardized factor loadings were hypothesis and study objectives (0.78), research ethics (0.67), and mentor relationship (0.64). Thus, each question was strongly correlated with the previously identified latent factor. When comparing residents and faculty, we observed differences in the design priorities, types of studies, and internal and external competitive funding, which were most highly rated by faculty members (online supplementary table 8).
Because this domain was descriptive and different for residents and faculty, factor analysis and scree plot were not applied. Instead, content and sampling validity was assured by assessing four and five items in faculty members and residents. The intraclass correlation coefficient was 0.92 (95%CI 0.73 to 0.99) and 0.92 (95%CI 0.75 to 0.98) for faculty and residents, respectively.
Most faculty members (n=39; 86.7%) expressed interest in supporting research programs for residents. The preferred modality was mentoring (n = 30, 78.9%), followed by a review of research projects (n = 50, 50%) and participation in seminars on research topics (n = 14, 36.8%). Most residents (n = 46, 74.2%) were interested in participating in a research support program. The preferred way to participate was having a mentor (n = 32, 65.3%), followed by writing and developing research projects (n = 30, 61.2%).
Data triangulation
In summary, both groups agreed on mentoring, protected time, and the inclusion of research in the program structure as facilitators. On the other hand, the lack of research culture, knowledge of the residents' research methodology, and interest in conducting research were considered barriers by both groups. A partial agreement was found in the "competition with other activities" barrier. The absence of an early review of research projects, residents' and faculty members' failure to relate research to professional performance, the rigidity of research requirements, and the absence of a formal instance of research communication between programs were only described in the focus groups. In contrast, the presence of gender gaps was only found in our quantitative analysis. The supplementary material (online supplementary table 9) shows additional information on the convergence matrix.
Discussion
Our study sought to identify barriers and facilitators for research development by medical residents in a faculty of medicine at a highly productive Latin-American university. Applying a mixed qualitative-quantitative approach, we identified gender gaps, lack of mentoring and protected time as the major barriers. Conversely, an established structural frame for research and funding weres identified as key facilitators. Medical residents and faculty members agreed on the high value of research and the role of faculty members as facilitators of residents' participation in research by offering more options according to residents' particular interests and abilities. In line with our findings, Peskin et al. [29]] reported that 95.6% of psychiatry residents consider research inclusion essential during their training. However, 76.6% also consider their research training "deficient". Another interesting finding in this study is the relatively low percentage (32.7%) of residents with scientific publications in international journals, much lower than national publications (47.5%). These numbers could be partially explained by the lack of (appropriate) mentoring, limited funding to cover the costs of open access in international journals, and language barriers. A study by Cimbaro Canella et al. [30] reports that about 30.8 % of research projects among pediatric medical residents were eventually published in Argentina. Investigators indicate that lack of time was the most frequent reason (45.9%) behind these low figures.
Our study also found significant differences in terms of academic productivity by gender. While 37% of females had national publications and 34% had international publications, among males, these figures were 62.7% and 66%, respectively. Interestingly this finding went unnoticed in our qualitative analyses of the focus groups and reinforced the power of the mixed methodology applied in our studies. Although this gender gap seems to be a worldwide issue [31], it may be even more significant in South America, where the percentage of female first authors is 28.6%, versus 54.6% and 38.2 in Europe and North America, respectively (p < 0.001) [32]. In this regard, Rexrode et al. [33] further explored this issue, suggesting that cultural differences may account for gender barriers.
As pointed out, lack of time, competition with other activities, and lack of research funding are the main barriers to research among faculty members. Residents also acknowledge the lack of research training as a barrier. These results are consistent with the literature [9,34]. In contrast, a study in Thailand pointed out that many residents had no motivation for research [35].
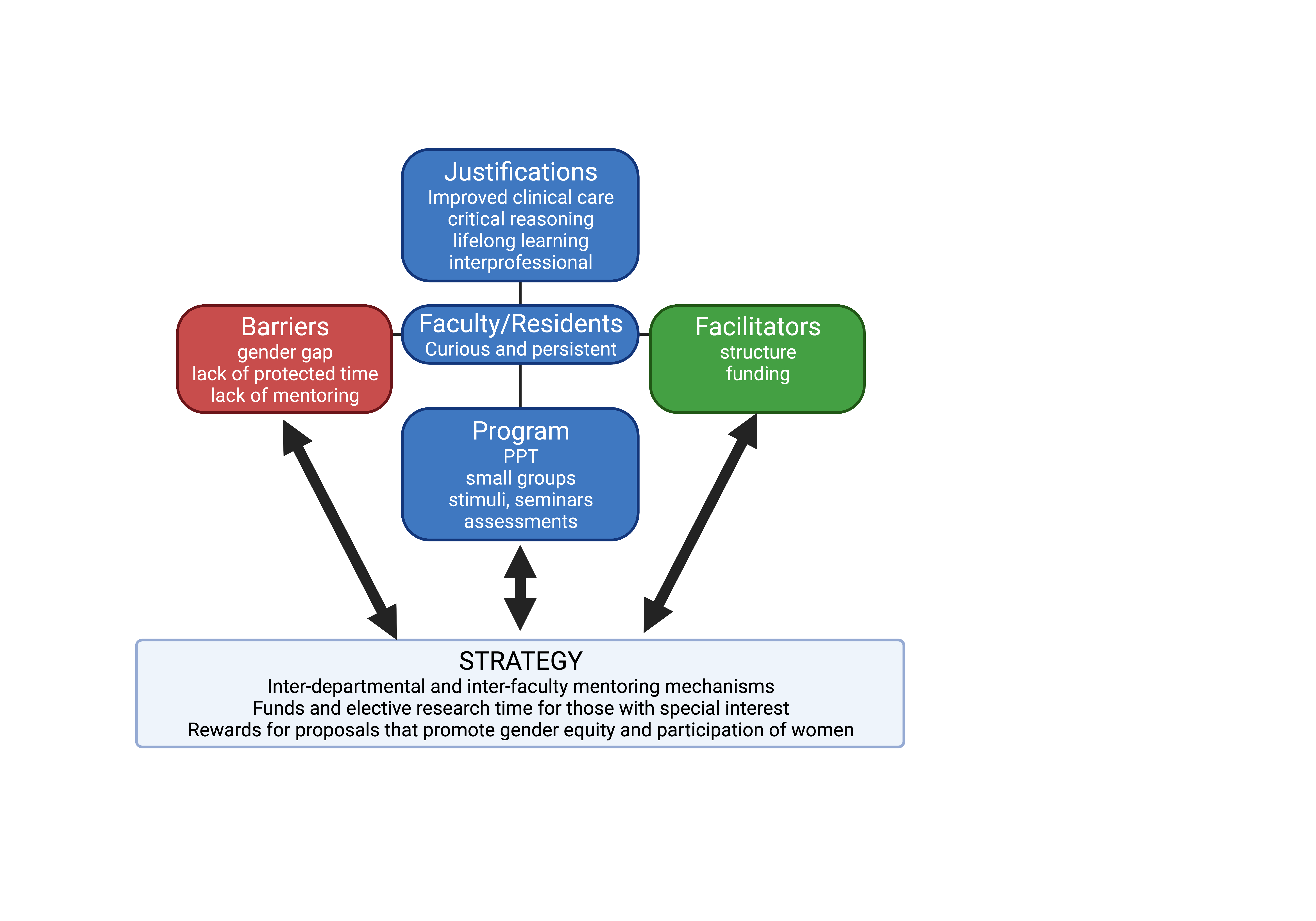
In our experience, large medical programs such as internal medicine and pediatrics have incorporated more structured approaches to enhance research, including mandatory courses along with a requirement to write and develop research proposals for residents. In contrast, smaller programs such as gastroenterology or intensive care have adopted more flexible strategies based on mentorship and research proposals developed under protected time by residents, during their programs, with the support of clinical or basic science researchers. Both approaches should be balanced when seeking to maximize the research potential of residents. A summary of findings and recommendations is presented(Figure 3).
Summary of findings and recommendations.
It is important to recognize some of the limitations of our study. First, our survey sampling strategy did not consider the heterogeneity of the different residency programs. Second, biased participants may have selected themselves since the surveyed population cannot be described. Furthermore, the small sample size may not represent the diversity among medical residency physicians. Finally, the quantitative analysis of publication rates could have been obtained from a validated external source, such as journal citation reports, rather than self-reports. Given the above limitations, some of our findings may not apply to various medical residency programs. Further studies on this topic are needed to confirm or discard our conclusions.
Notably, several questions remain unsolved, for example: how can we improve the transfer of clinical and research experience between departments within an institution? How can we select the best mentors to obtain a better trainee-mentor match? Is there any way to ensure minimum knowledge among all residents? And at the same time, provide enough flexibility to ensure that residents interested in research have access to the necessary resources.
Looking forward, some strategies to enhance research might include: 1) Establishing interdisciplinary mentoring programs that link residents and researchers. 2) Maintaining a balance that ensures minimal research skills for all residents, favoring mentoring with funding and optional research time focused on residents with interest and from under-represented groups or minorities, 3) Rewarding proposals that support gender equality and promote women's participation.
Conclusion
Research is highly valued by both residents and faculty members at a Latin-American university with a strong academic output. Major barriers to promoting research in this context include lack of protected time and effective mentoring, and gender gaps. Future interventions to overcome these barriers may include establishing interdisciplinary mentoring programs for residents and researchers from different medical residency programs and faculties, providing funding incentives and the option of more protected research time for those with a special interest in this field, and finally, rewarding proposals that include gender equality and promote the active participation of women to strengthen the research of Latin-American female residents.

