Research papers
← vista completaPublished on May 9, 2023 | http://doi.org/10.5867/medwave.2023.04.2660
Interscalene block in the context of enhanced recovery for shoulder: A case series
Bloqueo interescalénico en el contexto de la recuperación acelerada para artroscopía de hombro: serie de casos
Abstract
Introduction The application of enhanced recovery in shoulder surgery has not had such a favorable acceptance, therefore, the objective of this study was to present and describe the use of interscalene block to promote enhanced recovery in a series of patients undergoing shoulder arthroscopic surgery.
Methods Thirty-five patients undergoing arthroscopic shoulder surgery were included, in whom interscalene blockade and sedation were administered. Subsequently, pain intensity, nausea, vomiting, dyspnea, presence of Horner’s syndrome, blurred vision, hoarseness, time elapsed to discharge, unplanned readmissions, patient satisfaction, and compliance with hospital discharge criteria in the first 12 weeks were evaluated, hours following the criteria of an enhanced recovery.
Results 27 patients (77,1%) had ASA I and 8 patients (22,8%) ASA II, 97,1% were rotator cuff repairs. Before discharge, two patients (5.7%) had nausea. At discharge, no patient had dyspnea or blurred vision, two patients (5.7%) developed hoarseness, and the median pain intensity was 1.0 (0.0-7.0). Between 24 and 48 hours only one patient (2.8%) presented nausea and the median pain intensity was 1.0 (0.0-8.0). All the patients were satisfied with their willingness to repeat the experience, 100% of the patients met the criteria for medical discharge after 12 hours, 30 patients (85.7%) were discharged the same day, the stay was 12 (11.5 to 12.5) hours, and no patient was readmitted.
Conclusion In selected patients with a committed, trained and experienced surgical-anesthetic team, there is a high possibility that the interscalene block will favor the performance of enhanced recovery programs in shoulder arthroscopic surgery.
Main messages
- Shoulder arthroscopy is one of the world’s most frequently performed orthopedic surgeries, so finding a multimodal perioperative management strategy is a priority.
- The application of enhanced recovery in shoulder surgery is more complex than in other orthopedic surgeries.
- The present case series provides information on how the enhanced recovery protocol can provide quality surgical and anesthetic care to shoulder surgery patients.
- Limitations of this study are the small sample size, which could affect the results, and the indirect assessment of diaphragmatic hemiparesis based on the presence of dyspnea (which was not reported in our patients), lacking an objective analysis, we cannot assert that it did not occur.
Introduction
Enhanced Recovery After Surgery (ERAS) includes a combination of pre-, intra-, and postoperative strategies based on current evidence, which aims to improve patient recovery and function by minimizing the response to surgical stress and postoperative complications and, consequently, reducing hospital stay and costs [1,2]. The application of accelerated recovery in shoulder surgery is more complex than in other orthopedic surgeries [3,4,5], even though interscalene block is a technique that has been shown to produce adequate trans- and postoperative results [6,7,8,9,10]. In an attempt to promote accelerated recovery in shoulder surgery, the University of Pennsylvania published the Shoulder Arthroplasty Enhanced Recovery Protocol (ShARP), where its core points are: patient education, multimodal analgesia based on the use of continuous ambulatory interscalene block, use of antifibrinolytics and postoperative nausea or vomiting prophylaxis, through a multidisciplinary team and the appropriate selection of patients. This means that for those who have adequate home support, who can take care of themselves, and whose diseases are controlled, a reduction of 1.5 days of hospital stay is achieved with this procedure; however, its application and benefits are still under study [8,11]. Despite all this, there is still controversy about its use as a single anesthetic technique since, in most cases, it is used in combination with general anesthesia, and there is even debate about which of the two techniques is more advantageous for this type of surgery [12]. The application of general anesthesia produces numerous adverse effects such as nausea/vomiting, hoarseness, postoperative cognitive dysfunction, and inadequate pain control, the combination of which can result in a longer stay in the postanesthesia care unit and longer hospital stay [11]. The application of regional anesthesia as a single anesthetic technique reduces these effects. Above all, it favors adequate pain control, and if performed within a multimodal analgesia program, such as the accelerated recovery program, it could be carried out in most centers where there are qualified personnel to perform them. Therefore, this study aims to present and describe interscalene blockade in a single dose plus sedation to promote accelerated recovery in a series of patients undergoing arthroscopic shoulder surgery.
Methods
A case series study was conducted from February 1st, 2020, to February 28th, 2022, after approval by the research committee of the Ángeles Metropolitano Hospital and signed informed consent of the patients. All patients scheduled for shoulder arthroscopy at the Ángeles Metropolitano Hospital were included in the study, using a non-probabilistic sampling of consecutive cases. These cases were managed under an enhanced recovery approach after surgery. We included patients of both genders aged 18 to 80, with a physical condition according to the American Society of Anesthesiologists (ASA) classification type I and II, with a body mass index from 18.5 to 39.9 kilograms per square meter. Patients with coagulopathies, renal, hepatic, or cardiac failure, as well as obstructive or restrictive lung disease, pregnancy, dermal or infectious neck problems, who did not understand the nature of the enhanced recovery, with a home more than two hours away from the hospital, or with no means of rapid travel to the hospital, or patients who were unable to care for themselves or who did not have adequate home support were excluded. As of March 2020, patients who were included had to have a negative PCR test for SARS-CoV-2 and a negative chest x-ray on admission to the hospital, both performed within the previous 24 hours. Once selected, their management was explained to them, and they signed the informed consent form.
The preoperative strategies were: first surgery of the day: six or seven o'clock in the morning; fasting no more than eight hours, so the previous night they had to have dinner at 22 or 23 o'clock; no premedication with long-acting benzodiazepines, except for patients with chronic use of benzodiazepines in whom their usual dose was not suspended; and antibiotic prophylaxis with cephalothin two grams, 30 minutes before surgery. In patients with known allergies to cephalosporins or penicillin, we used clindamycin 900 milligrams. Compression stockings were placed for mechanical thromboprophylaxis and preventive analgesia with non-steroidal anti-inflammatory drugs (parecoxib 40 milligrams, in allergic patients, it was changed to ketorolac 60 milligrams).
Transoperative strategies were anesthetic technique with interscalene blockade in a single dose plus sedation, normothermia, first dose of central analgesic (paracetamol 1 gram), initiation of antiemetics (ondansetron 8 milligrams). Postoperative strategies were continuous cryotherapy system (Kodiak Breg Inc. United States) in the affected shoulder, restarting of the oral route as soon as possible, continuous analgesics, and rotation to oral administration; the analgesic guideline for home use was celecoxib, paracetamol, tramadol. In addition, an adequate understanding of the indications in case of emergency, i.e., severe pain not controlled with the established guideline, was corroborated ((Figure 1).
Management Protocol
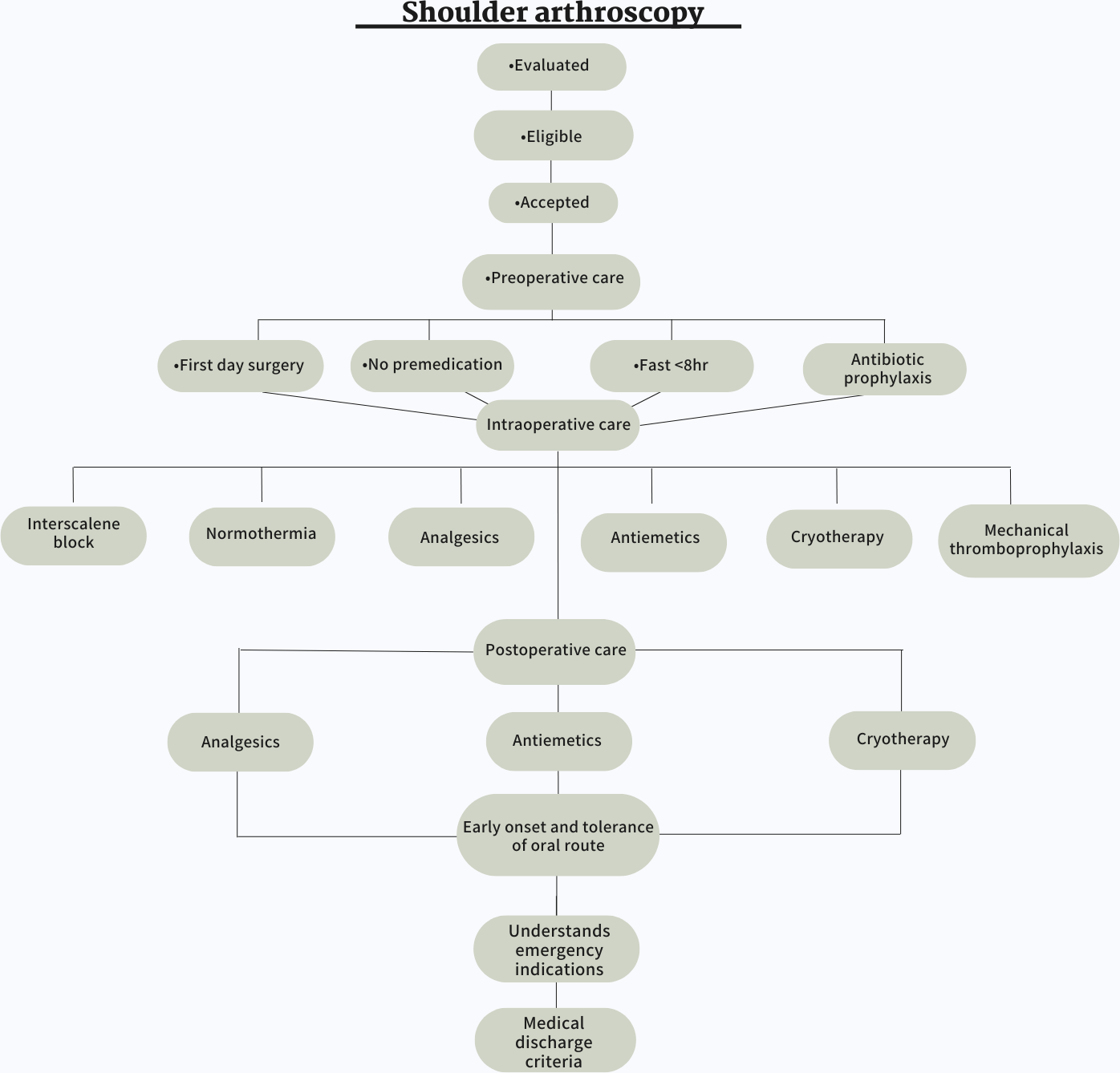
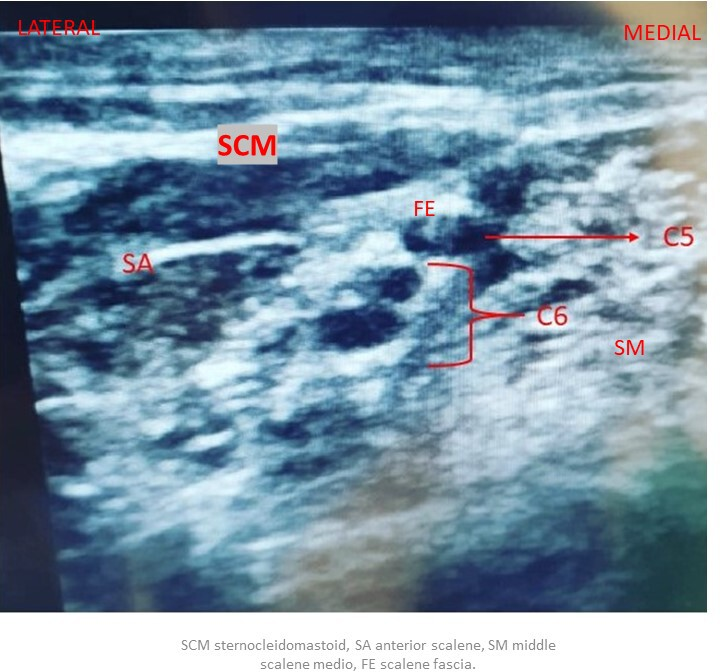
The anesthetic technique used was interscalene block and sedation. All patients were placed in the beach chair position. The interscalene block was performed in a single dose, guided by ultrasound (Edge II Ultrasound System Fujifilm-Sonosite Inc. United States) with a high-frequency linear transducer of 15 to 6 megahertz (HFL 50x Fujifilm-Sonosite Inc. United States). The transducer was placed over the neck at the level of the cricoid cartilage, transversely, until the three hypoechoic structures representing the brachial plexus were located Figure 2. Skin asepsis was performed with 2% chlorhexidine gluconate skin solution (per time) and 70% isopropyl alcohol (volume over volume) with dye (Chloraprep Becton Dickinson, France). The approach was performed on a short axis with a 50-millimeter insulated needle (B-Braun Melsungen AG Stimuplex A50, Germany). Once the nerve trunks were visualized, local anesthetic was applied with the tip of the perineural needle, visualizing adequate circumferential diffusion without the anesthetic leaving the scalene fascia. The anesthetic dose consisted of a fixed mixture of ropivacaine 112 milligrams plus plain lidocaine 100 milligrams, equivalent to a volume of 20 milliliters. Sedation was standardized with midazolam at 400 nanograms per kilogram and fentanyl at 1 nanogram per kilogram, followed by a continuous infusion of dexmedetomidine at a dose of 1 nanogram per kilogram during the first hour and during the second hour at 0.5 nanograms per kilogram to maintain a grade III sedation according to the Wilson scale [13]. Supplemental oxygen was applied with a reservoir mask at six liters per minute. All patients underwent surgery by two shoulder surgeons with more than ten years of experience in this type of surgery.
In all patients, the following outcomes were evaluated: pain intensity with a visual analog scale (VAS) from 1 to 10; the presence or absence of nausea, vomiting, diaphragmatic paresis (indirectly by the presence of dyspnea), Horner’s syndrome, blurred vision or hoarseness at discharge and at 24 to 48 hours after discharge through a telephone call; time to discharge (controlled pain, no nausea or vomiting, no dyspnea and tolerating oral route) in hours; patient satisfaction (very satisfied, satisfied, not very satisfied, dissatisfied, dissatisfied) at discharge; unscheduled readmission to the hospital after discharge. For statistical analysis, measures of central tendency (median) and dispersion (interquartile range, 25th to 75th quartile) were used for quantitative variables with non-normal distribution and absolute and relative frequencies for qualitative variables in the SPSS version 22 statistical program for Windows.
Results
Thirty-five cases were included, of which 20 (57.1%) were males and 15 (42.8%) were females. The median age was 49 (interquartile range 43 to 61). According to physical status, 27 patients (77.1%) were ASA I, and eight (22.9%) were ASA II. The median body mass index was 24.07 (20.24 to 38.01) kilograms per square meter. The preoperative diagnosis was in 34 cases (97.1%) rotator cuff rupture and in one case (2.8%) acromioclavicular osteoarthritis (Table 1).
Before discharge, two patients (5.7%) presented nausea. At discharge, no patient presented dyspnea or blurred vision; two patients (5.7%) presented hoarseness with a median pain intensity of 1.0 (interquartile range: 0.0 to 7.0). After 24 to 48 hours, only one (2.8%) patient presented nausea with a median pain intensity of 1.0 (0.0 to 8.0). Regarding patient satisfaction, all patients were very satisfied and mentioned that they would repeat the anesthetic experience. The oral route was restarted in all patients before the fourth postoperative hour. All patients had adequate medical status at 12 hours. However, only 30 patients (85.7%) were discharged as planned on the same day, resulting in a median hospital stay of 12 (11.5 to 12.5) hours. The remaining five patients (14.3%) were discharged the following morning. This generated a median length of stay of 24 (23 to 25) hours. This delayed discharge was not due to medical issues, as all patients could be discharged. There were no unscheduled readmissions.
Discussion
Shoulder arthroscopy is one of the most frequently performed orthopedic surgeries in the world, so seeking a multimodal perioperative management strategy is a priority, as well as using the most appropriate anesthetic technique to promote the early discharge of patients. As previously reported by Danninger [10], the use of regional anesthesia in conjunction with general anesthesia in shoulder surgery reduced the risk of hospital readmissions in outpatients by 18% and reduced the use of intensive care beds by 50%. These findings may be related to reduced opioid use and improved analgesia produced by the nerve block. No patient underwent general anesthesia in our series, and none required intensive care management for two reasons. First, no potent opioids were used in the postoperative period due to the analgesic effect of the interscalene block, which significantly reduces pain. Secondly, there were no serious complications derived from the nerve block, which, although infrequent, should be considered. The set of benefits produced by the interscalene block analgesia program ensured that the patients were ready to be discharged 12 hours after the surgery. It is important to note that the medical criteria necessary to discharge the patients to their homes were met. Likewise, we should bear in mind that although the analgesic effect of the interscalene block decreases in the following hours, if multimodal analgesic management is started on time, adequate pain management is achieved during the first 48 hours, when postoperative pain is expected to be more intense. A big dilemma exists between performing shoulder surgery with general or regional anesthesia. The most common is the combination of both [14], still in our series, we see that it is entirely possible to use only one technique to perform this type of surgery, which makes it an interesting management proposal [11,15].
Ding’s study [11] found that in shoulder surgery, the use of regional anesthesia alone compared to general anesthesia resulted in significantly higher rates of same-day home discharge compared to institutionalized care, fewer overall hospital complications, and reduced hospitalization and readmission rates. These favorable results are not new, as a study reported in 1995 by D'Alessio [16] showed that there were fewer unplanned readmissions due to severe pain, sedation, and nausea/vomiting, which was corroborated in our patients.
Despite these advantages, regional anesthesia is not widely used. For example, in 27 201 rotator cuff repairs, only 15.4% received interscalene block plus general anesthesia, and no patients received nerve block alone [10]. This may explain, in part, the low utilization of enhanced recovery programs. Some authors argue that this is because regional anesthesia alone may not be suitable on a routine basis. However, in our study and previous studies of our group, we have shown that with an adequate selection of patients, with a standardized management program such as enhanced recovery, as well as having a trained anesthetic team (which would be the foundation of this program), it can be applied to the vast majority of patients and can be widely used. Also, there are other reasons for non-utilization, such as requiring a highly skilled surgeon who is comfortable with an awake/sedated patient. In our case, shoulder surgeons (MR, AC) are fully familiar with this situation and do delicate tissue management and arm movements as they are convinced that the benefits offered to their patients are very good. In addition, an anesthesiologist skilled in regional anesthesia is required. One of our authors (GM) has 15 years of experience in these techniques and, fortunately, the new generations (GA) are taking the use of regional anesthesia very seriously, in accordance with the worldwide trend of an increase in the use of nerve blocks in the last two decades [17].
It is necessary to provide a pleasant environment for the patient. This implies strict normothermia, regardless of the operating room temperature, and control of the noise generated by the hammering and reaming of the anchors since these stimuli can be unpleasant. However, when the block is effective, they are not painful, although sometimes this discomfort cannot be attenuated with mild sedation [18]. For this reason, the recommendation is to perform deeper sedation when these surgical maneuvers are to be performed. This is achieved with a team vigilant to the procedure to adjust the depth of sedation and adequate amnesia and/or anxiolysis in case of untimely awakening by noise. For these reasons, in our study, we kept the patients under grade III sedation, where, despite the manipulation, they remained comfortable. General anesthesia provides this comfort, amnesia and akinesia. It should be noted that these needs are covered with adequate sedation, such as the one we generated. We did not assess akinesia in our cases, but interscalene blockade provides adequate akinesia to perform shoulder surgery [18]. An important benefit of having a patient awake in the beach chair position is the reduction of complications from inadequate cerebral oxygenation [18]. However, it also involves having limited access to the airway, which is a challenge for the anesthesiologist [19,20]. In our study, cerebral oxygenation was not monitored in all patients because, despite its routine use, we have had problems with the supply of sensors. There was no need for urgent airway control in our patients, and although it is a potential risk, in our opinion, the occasions when urgent airway control is required are rare. In these cases, the change of position can be accomplished quickly using commercial beach chairs. Examples of these are the Deluxe Arthroscopic Legholder device (Allen Medical Systems) or the Tmax shoulder positioner device (Smith and Nephew). In our case, we use the former most frequently.
We believe that regional anesthesia is underused in the management of upper extremity surgeries and under-implemented in enhanced recovery protocols after surgery [21]. The present case series provides information on how quality surgical and anesthetic care can be given to shoulder surgery patients with enhanced recovery protocol. Following these systematized strategies, in most cases, will generate favorable results. The limitations of our study are related to the small sample size, which could affect the results.
The limitations of our study are related to the small sample size, which could affect the results. In addition, diaphragmatic hemiparesis was indirectly evaluated with the presence of dyspnea, which was not reported in any patient. However, without an objective analysis (evaluation of diaphragmatic mobility by ultrasound, Figure 2), it cannot be asserted that it did not occur.
Conclusions
In this series of cases, a high possibility that interscalene blockade favors enhanced recovery programs can be observed. This is due to the fact that 100% of the patients had medical conditions for discharge 12 hours after surgery. All that is required is an adequate selection of patients and a trained, committed and experienced surgical-anesthetic team.

