Estudios originales
← vista completaPublicado el 14 de junio de 2023 | http://doi.org/10.5867/medwave.2023.05.2685
Estudio exploratorio de las motivaciones para la criopreservación de ovocitos en forma electiva
An exploratory study of motivations for elective oocyte cryopreservation
Abstract
Introduction Oocyte vitrification is a scientific advance that has changed the reproductive perspective of human society. This procedure has been offered as an alternative to the voluntary postponement of pregnancy, giving women a new perspective on their reproductive autonomy. The number of women who consult and then choose to freeze oocytes has increased almost exponentially in Chile and throughout the world. There is little knowledge about the motivation, experience, and results of elective oocyte cryopreservation in Chile. The objective was to know the motivation, experience, and future reproductive desire of the women who underwent this technique.
Methods Cross-sectional descriptive study based on a questionnaire sent by e-mail in which females who had previously undergone elective oocyte cryopreservation between January 2011 and December 2019 at Clínica Alemana, Santiago, Chile, participated.
Results Of 342 women who had completed a cycle of elective oocyte cryopreservation, 193 agreed to participate, and of these, 98 (51%) answered the survey satisfactorily. Women who underwent this procedure for medical indication, including endometriosis, cancer, and low ovarian reserve, were excluded. The most frequent reason for the procedure was age (44%). Concerning the procedure: 94% do not regret having it done, and 74% of the women believe that they will use their oocytes at some point in their lives. Finally, from the time of oocyte cryopreservation to date, 11% of the surveyed women have used their vitrified oocytes, and 27% have become pregnant.
Conclusions Women who undergo elective oocyte cryopreservation for social reasons are mainly women without a partner whose main motivation is their reproductive age. The vast majority do not regret doing so.
Main messages
- Women are increasingly using oocyte cryopreservation as a contingency measure against the expected decline in fertility.
- This is the first article in the country to understand the social and reproductive motivations of women who undergo elective oocyte cryopreservation.
- Overall, it is a process well evaluated by respondents and presents reproductive outcomes comparable to the published literature.
- The main limitations are the cross-sectional design, the low response rate, and the variable interpretation of the questions.
Introduction
The development of an efficient and reproducible method of oocyte cryopreservation has been of great scientific interest in recent decades [1]. When first developed in the late 1980s, oocyte cryopreservation allowed women to preserve healthy eggs in the face of possible infertility due to a medical condition or medical treatment. Initially, traditional slow-freezing protocols offered unsatisfactory results regarding oocyte survival due to the formation of ice crystals, which impaired cell survival [2,3,4]. However, with the development of vitrification, interest in fertility preservation has reemerged [5,6]. This technique has significantly increased frozen oocytes' survival and fertilization rates [7,8], similar to those of fresh oocytes [9]. Therefore, egg freezing is now considered a way to preserve fertility for medical and "social" reasons [10].
Fertility preservation for social reasons is an increasingly frequent practice, with many women deciding to postpone childbearing [10,11]. From a sociocultural perspective, it could be explained by the expectation of finding a stable partner or achieving financial, professional, or personal maturity [12,13]. However, concerns have been raised regarding the ethics of offering healthy women a costly and potentially ineffective service [12]. The success rates of egg freezing remain highly variable, and the few studies reporting pregnancy rates with frozen oocytes are usually performed in specialized centers working with oocytes from women much younger than those seeking social freezing [7,8,14].
For the American Society of Reproductive Medicine and other scientific societies, "social freezing" (more recently termed "planned" or "elective" fertility preservation) has proven to be a safe and ethically acceptable strategy, even for women who are not in danger of losing fertility immediately [15]. However, there is little evidence in the literature about the clinical outcomes of women who have decided to undergo elective cryopreservation to safeguard their fertility for the future. The main reason is that, despite the increasing number, this option has only recently become available, and the utilization rate of vitrified oocytes is low [16,17,18,19,20]. To date, only one study by Cobo et al. reports that just 8.7% of women have actually used their oocytes [21]. . Further studies show that 20-48% attempted to conceive naturally or by reproductive medicine techniques after elective cryopreservation, in most cases without using their frozen oocytes [22,23,24].
Finally, the motivation of women who undergo planned oocyte freezing and the sociological impact of the procedure has been discussed in multiple scientific articles worldwide, given that there is increasing demand. However, there is little evidence in South America on who is accessing social egg freezing, why they are taking this option, and their experiences and future intentions.
In our country, elective cryopreservation can only be performed out of pocket at high costs and without health insurance coverage. For these reasons, it is interesting to understand the motivations, experiences, and reproductive outcomes of women who underwent cryopreservation in a single center.
Therefore, our study aimed to know the motivation, experience, and future reproductive desire of this group of women who underwent this technique.
Methods
We conducted a cross-sectional descriptive study. For this purpose, a database of all women with elective oocyte cryopreservation by vitrification was created. The period studied was from January 2011 to December 2019 in the reproductive medicine unit of Clínica Alemana of Santiago.
Inclusion criteria were women over 18 who underwent oocyte cryopreservation at our center (regardless of nationality or medical residency country). Women who underwent cryopreservation due to cancer, endometriosis, low ovarian reserve, or vitrification of oocytes left over from in vitro fertilization were excluded.
The cohort of potential candidates for the survey included 342 women who were contacted by telephone. Only 325 women could be reached, resulting in a volunteer participant sample of 193, who received a link to the survey via e-mail.
The reproductive medicine team developed the survey in conjunction with the psychology team and ethics committee. It included 18 closed-ended, multiple-choice questions on the participants' demographics, reproductive and personal status. All women who answered the questionnaire agreed to sign an anonymous informed consent form beforehand.
The questions were designed to relate women’s intentions and attitudes towards elective cryopreservation, educational level, marital status, desire to have children, and reproductive history. Each participant was given a unique code to complete the questionnaire, and all responses were collected in a secure database and analyzed using descriptive statistics. The electronic survey software was REDCAP.
Approval and follow-up based on our questionnaire were reviewed and authorized by the local ethics committee, resolution UIEC 1013.
Results
Between 2011 and 2019, 342 women underwent at least one elective cryopreservation cycle. A total of 325 women were contacted, of whom 193 agreed to participate. They were then sent the questionnaire by e-mail after approval of informed consent. In total, 98 women returned completed questionnaires, yielding a response rate of 51%.
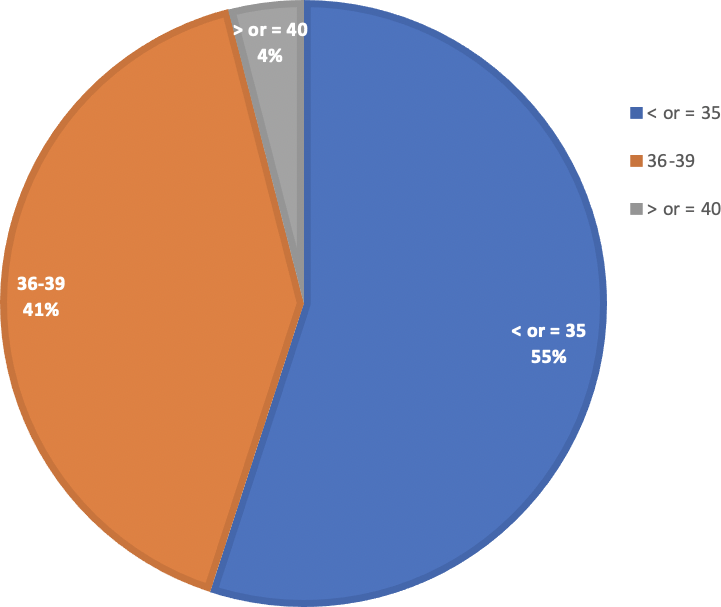
The mean age at cryopreservation was 34.4 ± 2.5 years (Figure 1).
Percentage of oocyte cryopreservation according to age.
The proportion of women who underwent this procedure increased over time, 6% between 2011 and 2013, 15% between 2014 and 2016, and 79% from 2017 to 2019.
At the time of cryopreservation, 72% of women were single. However, when answering the survey, there were substantially fewer single women (30%), as shown in Table 1.
Regarding the experience of the elective cryopreservation process (Table 2), the great majority considered it a good experience (79%) and did not regret having done it (94%). Of the women who regretted having undergone the procedure (6%), the main reason was the feeling of physical and emotional exhaustion (50%).
The main cause for cryopreservation was age (44%) (Figure 2).
Causes for oocyte cryopreservation.
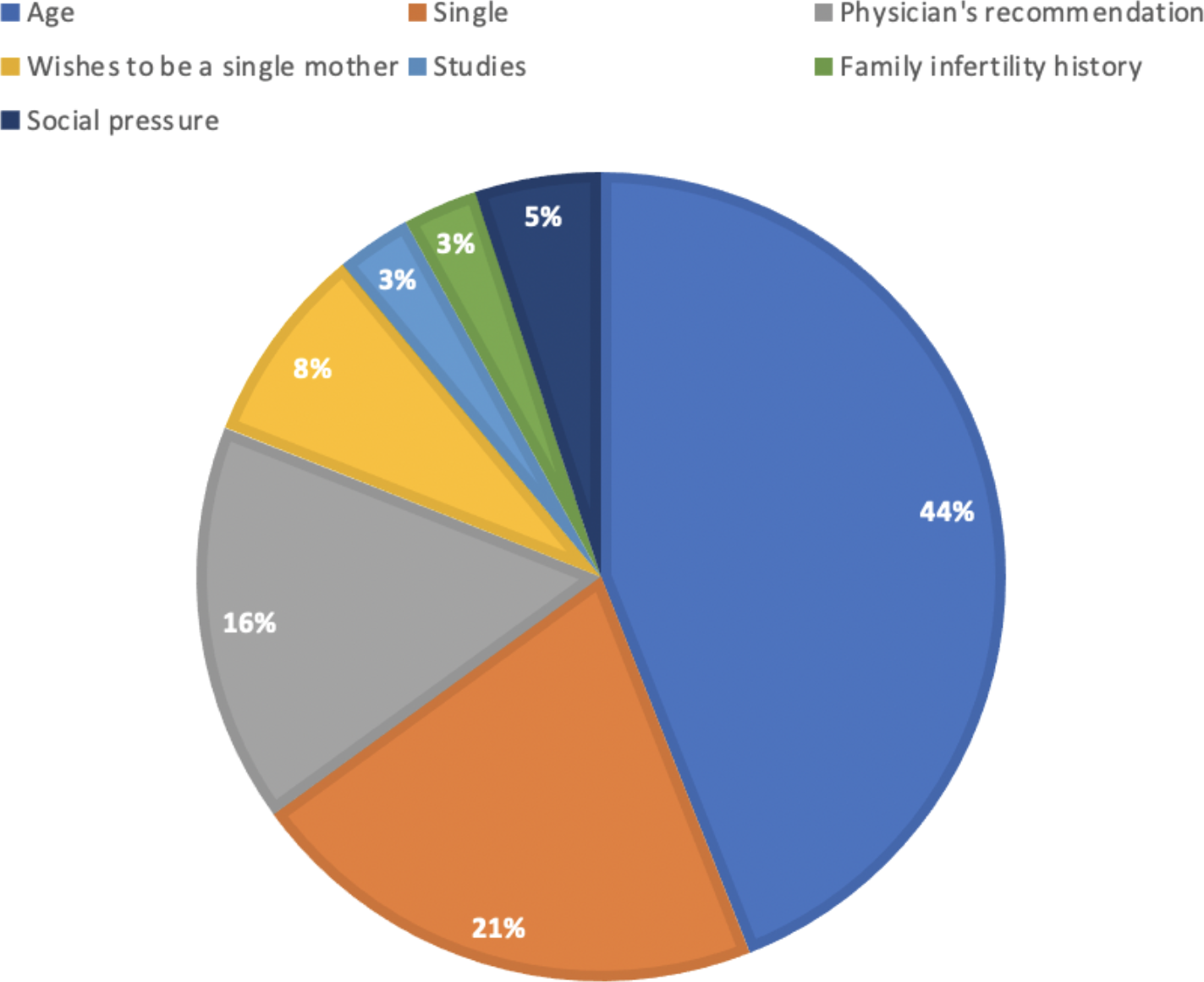
When asked if they would have cryopreserved oocytes earlier if this procedure was less expensive, 54% answered yes, and 41% would have done more than one cycle. Regarding the reasons for cryopreserving oocytes, 44% answered that it was because of their age and 21% because they did not have a partner.
Regarding the women’s attitude towards using cryopreserved oocytes (Table 3), 74% believe they will use their oocytes in the future, and 11% have already used them. When asked how long they expected to keep the frozen oocytes, 47% would keep them for a maximum of 5 years.
Regarding the desire for pregnancy after oocyte cryopreservation, 40% had tried to become pregnant, 69% achieved pregnancy without using their frozen oocytes, 96% with their partner, and 3% with a sperm donor. Of the pregnancies without using oocytes, 55% were spontaneous, 14% through insemination, and 31% through in vitro fertilization. Finally, 11% of the women tried to get pregnant with their frozen oocytes, and 27% succeeded.
Discussion
Declining fertility rates and the increasing age of women at first pregnancy worldwide are multifactorial and would be related to better educational and career development opportunities for women. This new preference for delaying childbearing is reflected in our study by the increase in the number of women who have cryopreserved. Programmed oocyte freezing" is a popular topic in the media, and the demand for the procedure has increased rapidly. In our center, in the last three years, it increased threefold compared to the first six years of freezing. This is related to the dissemination strategies on cryopreservation and the recommended age for cryopreservation. It is interesting to note that the vast majority of respondents obtained information about this process through their physician (44%), which is positively surprising when comparing our results with other works where the main source of information about the program was through friends, relatives, social networks and non-specialized websites [16,23]. This result is important, and although most gynecologists currently inform their patients about age-related fertility decline, there is still much room for improvement regarding communication from healthcare providers to the public [25].
A progressive decline in oocyte quality and quantity is associated with women’s age, expressed in a higher incidence of infertility, increased miscarriage rates, low response to ovarian stimulation, and lower oocyte collection [26,27,28]. There is literature demonstrating the existence of many women unaware of age’s effect on fertility [29,30], which could compromise their reproductive future. This is an important consideration, and multiple studies recommend cryopreservation before 35 years of age [26,27]. In our work, the average age at freezing was 34.4 years, which is lower than in other studies where the average age was 38 years [8,28]. This age is interesting since it probably correlates with the information provided promptly by our healthcare professionals. In any case, it is noteworthy that almost 41% performed it between 36 and 39 years of age, despite this not being the most optimal age to obtain good results, with lower pregnancy and live birth rates [29,31]. A recent study examined the relationship between fertility decline with age and the possibility of achieving the desired family size [32]. This would agree with some studies showing that oocyte cryopreservation is a more cost-effective strategy to perform before the age of 38 years than in vitro fertilization after the age of 40 years [30,33]. As a result of all this information, several countries have a trend toward developing fertility awareness and fertility education platforms for adolescents and young adults [34].
In this study, the participants describe their main motivation for cryopreservation as age (44%) and, to a lesser extent, being without a partner (21%). In turn, the vast majority reported being an advanced professional with a postgraduate degree (58%) and a stable job (80%), which probably allowed them to access information easily through private healthcare providers. These responses are congruent regarding how many years they wish to keep their oocytes frozen; most would leave it longer than five years (47%), demonstrating that they have no plans to use their oocytes in the short term. This observation supports previous findings from other studies about buying time to find the right partner and that most women do not intend to pursue childbearing unless they have established a stable relationship with a suitable partner [35,36,37]. Women who have cryopreserved have more time to realize their family project and are more likely to establish a psychosocially compatible situation with childbearing [38].
Elective oocyte cryopreservation responds to the current demand of women for greater control of their reproductive potential. When evaluating the number of women who tried to become pregnant after the process (40%), most of them succeeded spontaneously (69%). Regarding cryopreserved oocytes, only 11% of women have used them to date, with pregnancy rates of 27%. These results are similar to those of the largest published series on nonmedical fertility preservation by Cobo et al., where only 12.1% of women returned to use their oocytes after waiting 2.1 years [20], with return rates reported in other series being even lower (6.5%) [39].
It is important to mention that most respondents reported having had a good experience (79%), and very few had regrets (6%). Probably, the feeling of security of cryopreservation and the decrease in the pressure of motherhood that is socially generated by age or marital status has produced a high degree of satisfaction with this procedure. This is reflected in the fact that 41% of the respondents would perform it a second time. However, if we analyze the group of women who regretted the procedure (6%), the majority reported that it was very tiring physically and emotionally (50%) or because of the low number of oocytes recovered (33%). These results resemble other studies, such as that of Greenwood et al., in which the perceived less adequacy of information and emotional support during the process were associated with regret of the decision [38]. These findings are extremely important in fertility centers offering elective cryopreservation, where physicians should provide adequate information regarding the possibilities of oocyte collection and pregnancy [40,41].
The strength of this study is that it is the first of its kind performed in our country, contributing local information to the existing literature. This could help inform women about planned oocyte vitrification.
Finally, due to the characteristics of the study, some limitations should be mentioned. The study design has the disadvantage of providing data from a single moment in time so that no conclusions can be drawn about patients who have not yet used their oocytes. On the other hand, the low response rate, the inherent limitations of self-reporting, incomplete responses, and the diverse interpretation of the questions should be recognized as possible sources of bias. Thus, a strategy to reduce selection bias would have been to ask patients the reason for nonparticipation, which we did not do in this study.
Conclusions
The widespread trend toward postponement of childbearing due to social changes has increased pressure on women’s reproductive window. In addition, advances in laboratory technologies encourage women to consider oocyte freezing. The introduction of elective cryopreservation provides options to partially relieve this pressure from a psychological standpoint and potentially improve fertility in a subset of women.
Return rates are low and contrast sharply with the high level of satisfaction with the procedure. However, elective vitrification still generates controversy because of the lack of studies.
As the number of oocyte cryopreservation cycles continues to increase, there is a real need to monitor why it is being done and the success rates achieved and educate our patients about these techniques.

