Estudios originales
← vista completaPublicado el 27 de septiembre de 2023 | http://doi.org/10.5867/medwave.2023.08.2720
Niveles de Burnout y factores asociados en trabajadores de la unidad de cuidados intensivos en la primera ola de la pandemia COVID-19 en Chile: estudio transversal
Burnout levels and associated factors among Intensive Care Unit workers during the first wave of the COVID-19 pandemic in Chile: A cross-sectional study
Abstract
Introduction The COVID-19 pandemic resulted in an unpredictable healthcare crisis with a high psychological burden on healthcare workers.
Objective To evaluate burnout levels and their associated demographics and occupational factors among intensive care unit healthcare workers during the COVID-19 pandemic in a single hospital in the city of Temuco, Chile.
Methods A cross-sectional design in which a sociodemographic questionnaire and the Maslach Burnout Inventory for Human Services were sent to health care workers in a single Chilean Intensive Care Unit during the pandemic COVID-19. Burnout levels, demographic, and occupational factors are reported using descriptive statistics; correlations between burnout levels and demographic-occupational factors were analyzed using Spearman’s and rank-biserial correlation coefficients; and multiple linear stepwise regression was used to assess the contribution of demographic and occupational factors to participants’ burnout levels.
Results A total of 84 participants (46 women and 38 men) were included in the analysis. Depersonalization and low personal accomplishment were evidenced in 95.2% and 98.8% of the intensive care unit healthcare workers, respectively. Emotional exhaustion was positively correlated with having children ( = 0.72; < 0.01). Age ( = 0.79; < 0.05), sex ( = 0.30; < 0.05), and prior experience in intensive care unit facilities ( = 0.71; < 0.05) were correlated with depersonalization. Feeling of personal accomplishment was positively correlated with with sex ( = 0.70; < 0.05) and type of work shift ( = 0.29; < 0.01).
Conclusions The intensive care unit healthcare workers in this study reported high levels of depersonalization and low feelings of personal accomplishment during an advanced stage of the COVID-19 pandemic. Older age, being female, having children, having intensive care unit experience, and working at 4th shift were factors related to burnout dimensions.
Main messages
- This study is the first published to evaluate burnout in Chilean Intensive Care Unit healthcare personnel exposed to COVID-19 patients.
- We found a high prevalence of burnout among Intensive Care Unit personnel.
- We recommend periodically evaluating the mental health of this population to design appropriate preventive programs.
Introduction
On March 11, 2020, the World Health Organization (WHO) declared a global pandemic [1]. To date, COVID-19 has drastically affected all countries [2], placing extraordinary demands on healthcare systems. In this sense, healthcare personnel working directly or indirectly with COVID-19 patients have been subjected to an increased psychological and physical burden [3], to the point that the WHO has identified them as a vulnerable group at risk of developing a wide range of mental health problems [4].
Healthcare workers in intensive care units (ICUs) are exposed to extreme conditions that increase the psychological burden at work [5]. This psychological burden and its impact on the mental health of healthcare workers in Chile has increased during the COVID-19 pandemic [6]. A frequent condition among healthcare personnel is burnout syndrome [7], defined by the 11th revision of the International Classification of Diseases as a state of chronic physical and mental exhaustion related to work activity that is not satisfactorily managed [8]. Before the COVID-19 pandemic, the prevalence of burnout ranged from 10% to 67% in healthcare workers [9,10,11], being significantly higher among surgical and emergency units than clinical specialists [11]. During the COVID-19 pandemic, burnout syndrome in healthcare workers ranged from 36.4% to 90.4% [12,13,14,15,16,17,18]. A recent systematic review by Aymerich et al. [13] that included 30 873 healthcare workers found a burnout prevalence of 37% [13]. Likewise, in their meta-analysis involving 2487 healthcare workers, Batra et al. (2020) reported a burnout prevalence of 37.4% [14]. Healthcare workers burnout has been extensively studied in healthcare workers during the COVID-19 pandemic. A high level of burnout has been observed in 36.4%, 77.0%, 80.2%, and 90.4% of Egyptian [12], Irish [16], Saudi [17], and Korean [18] physicians, respectively. On the other hand, only a few studies have reported burnout levels among ICU healthcare workers, showing high burnout levels in 60% of 136 Italian ICU healthcare workers (physicians and nurses) [19], in 75% of emergency physicians in a United States sample [20], and in 51% of 1001 European physician intensivists [21].
Burnout syndrome is characterized by three dimensions: emotional exhaustion, depersonalization, and a low sense of personal accomplishment [8]. Before the COVID-19 pandemic, high emotional exhaustion, high depersonalization, and low personal accomplishment were observed, ranging from 24.5% to 38.9%, 14.5% to 43.6%, and 28.3% to 34.3% in several healthcare workers [9,11]. During the COVID-19 pandemic, all dimensions of burnout were affected, with emotional exhaustion being the most affected [13], ranging from 24.5% to 46.1% in samples of healthcare workers [22]. Furthermore, high depersonalization and low sense of personal accomplishment have been observed in healthcare workers (nurses and physicians), ranging from 24.3% to 42.4% and 14.5% to 43.6%, respectively [23,24]. Burnout levels in ICU personnel have been described, reporting high emotional exhaustion, high depersonalization, and low sense personal accomplishment in ranges from 22.4% to 41.2%, 9.18% to 47.8%, and 12.5% to 29.7%, respectively [19,25]. In relation to the clinical expression of burnout, symptoms include frequent work absences, a tendency to abandon the profession, decreased self-esteem, and drug abuse, among others [26]. In addition, its consequences are associated with a higher incidence of medical errors, reduced patient safety [27,28], and a deterioration in the healhtcare workers's quality of life [29].
The demographic, occupational, and clinical factors associated with high burnout during the COVID-19 pandemic have been widely investigated. High burnout levels among healthcare workers have been associated with the female sex [22,30], lack of personal protective equipment [30], scarce experience on the job [30], co-worker infection or death [12], not having children [30], single marital status [30], deterioration of ethical climate [21], and having clinical disorders such as depression [19,30], anxiety [19,30], stress [30], and insomnia [19]. In fact, the personal purchase of protective equipment and severe depression increase by 2 and 5 times, respectively, the likelihood of developing high levels of burnout in healthcare workers [12,19]. Interestingly, only 8% of healthcare workers had high resilience [19], and going on vacation seemed the best coping mechanism for occupational burnout [25]. The vulnerability of healthcare workers during the COVID-19 pandemic is explained by a number of factors such as lack of access to adequate protective equipment [31], exhaustion due to the use of personal protective equipment, feeling lack of support [32,33], long working shifts, unexpected changes in the type of work [34], concern about infecting oneself or one's family members [35], leaving their own home [36], and concerns about seeing patients die [35]. Consequently, these factors can trigger feelings of loneliness, helplessness, and a range of additional emotional states: stress, irritability, despair, and physical and mental fatigue [22,37]. Indeed, healthcare workers have frequently experienced negative psychological effects during the COVID-19 pandemic, including recurrent burnout syndrome (34.4%) [37], anxiety (24.9%) [38], depression (24.9%) [38], post-traumatic stress disorder (9.6% to 51%) [34], and insomnia (38.9%) [39]. In this context, the psychological consequences of the COVID-19 pandemic may contribute to reduce the quality of life of healthcare professionals, jeopardizing their work performance [23,40].
In other countries, burnout syndrome in healthcare workers during the COVID-19 pandemic has been studied [19,21,25]. These studies found high burnout levels, ranging from 50% to 60% [19,21] and high risk of emotional exhaustion, depersonalization, and lack of personal accomplishment among ICU healthcare workers [25]. However, to the authors’ knowledge, there are currently no studies on the impact of the COVID-19 pandemic on burnout levels in Chilean ICU workers. In this scenario, understanding the psychological consequences of the COVID-19 pandemic on healthcare workers is critical to protect their mental health [41]. Therefore, understanding the burnout levels and potential risk factors associated with ICU healthcare professionals during the COVID-19 outbreak provides a picture of their mental health and enables authorities to provide timely and suitable measures not only to improve their psychological health and quality of life but also to promote the quality of patient care. For these reasons, the objective of this study was to determine the levels of burnout and its relationship with demographic and occupational factors in ICU workers during the COVID-19 pandemic in a single hospital in Temuco, Chile.
Materials and methods
Study design
A cross-sectional analytical study was designed for workers belonging to the ICU team of a single public hospital in Chile during the COVID-19 pandemic. The ICU facilities in which healthcare workers performed their work consisted of 12 beds located in single rooms, all occupied, and of which 67% (eight beds) were assigned to COVID-19 patients. In addition, each shift/working day had 12 ICU healthcare workers for the care of COVID-19 patients.
Participants
A total of 142 ICU healthcare workers of the Padre Las Casas Hospital were invited to participate in the study, including physicians, nurses, physiotherapists, nutritionists, occupational therapists, speech therapists, and pharmaceutical chemists. Convenience sampling through solicitation of survey responses was performed and the sample size was constituted by the ICU healthcare workers who consented to voluntarily participate in the study. For a sample size of 142 healthcare workers, a burnout prevalence of 84% [42], a 95% confidence level, and a margin of error of 5%, a priori sample size of 84 participant was calculated [43].
Measures
We provided a demographic-occupational questionnaire and the Maslach Burnout Inventory for Human Services Survey (MBI-HSS). The combined demographic-occupational survey was constructed by the authors and consisted of five demographic questions and four occupational questions. The demographic variables were age (years), sex (male, female), native origin (no, yes), marital status (single, married, divorced, widowed, and cohabitant), and having children (no, yes); the occupational variables were ICU experience (stratified years of experience), profession (physician, nurse, nursing technicians, physical therapist, nutritionist, occupational therapist, speech therapist, pharmaceutical chemists), type of employment contract (full-time: 44 hours/week contract, part-time: 22 hours/week contract, casual: variable hours/week contract; categorical, nominal), and type of work shift (regular shift: 8-hours day shift, 4th shift: 8-hours night shift, modified 4th shift: 16-hours day-night shift, and full shift: 24-hours day-night shift).
The Maslach Burnout Inventory for Human Services Survey consists of a 22-item questionnaire that assesses the three dimensions of burnout: emotional exhaustion (nine items): assesses feelings of feeling emotionally overwhelmed and exhausted by one’s work; depersonalization (five items): measures a callous and impersonal response towards recipients of one’s service, care, or treatment; and personal accomplishment (eight items): assesses feelings of competence and satisfactory achievement in one’s work [44]. Each item is ranked on a 7-point Likert scale ranging from 0 ("never") to 6 ("every day"), yielding a total score for each burnout dimension [45]. To characterize participants, total dimension scores were stratified as low, moderate, or high emotional exhaustion (≤ 18, 19 to 26, and ≥ 27 points, respectively), depersonalization (≤ 5, 6 to 9, and ≥ 10 points, respectively), and personal accomplishment (≥ 40, 34 to 39, and ≤ 33 points respectively) in accordance with a previous study [46]. Burnout was defined, in accordance with previous studies [47,48], as high scores on emotional exhaustion (i.e., ≥ 27 points) and/or high scores on depersonalization (i.e., ≥ 10 points). The Maslach Burnout Inventory for Human Services Survey has proven to be a valid (construct validity with Spearman’s rank correlation coefficient > 0.4 on all items for convergent validity) and reliable instrument (Cronbach’s alpha of 0.75 for total score, 0.85 for emotional exhaustion, 0.71 for depersonalization, and 0.76 for personal accomplishment) in healthcare workers [49]. Burnout was measured using the Spanish version of the Maslach Burnout Inventory for Human Services Survey adapted by Gil-Monte and colleagues [50,51]. Prior to the application, the content validity was measured by an expert panel using the Expert Judgment template proposed by Escobar-Pérez and Cuervo-Martínez [52], classifying each of the 22 items into four levels: deficient (1), regular (2), good (3), and excellent (4), to assess the coherence and clarity of the instrument.
Data collection
In September 2021, a researcher wihtout previous contact with potential participants administered the self-report instruments for data collection in person. Before participating, respondents were able to view our self-introductions, the purpose of our research, and a description of the instrument’s self-report contents. Only after respondents agreed to the take the survey was the content of the questionnaires initiated; otherwise, the survey ended immediately. Respondents could terminate the questionnaires at any time and choose whether or not to submit them after completion. Thus, respondents’ right to know was protected, and the questionnaires we received had their approval. There were no privacy issues, and the survey was anonymous.
Data analysis
The degree of agreement among experts was measured with the Fleiss kappa coefficient, an analysis statistic used to assess agreement among three or more raters independently judging measurement criteria from ordinal nature [53,54]. The degree of agreement was classified according to Landis and Koch [55], where kappa 1.00 to 0.81 equals an almost perfect agreement; 0.80 to 0.61 equals a substantial agreement; 0.60 to 0.41 equals a moderate agreement; 0.40 to 0.21 equals a fair agreement; 0.20 to 0.10 equals a slight agreement; and < 0.10 equals a poor agreement. The Maslach Burnout Inventory for Human Services Survey coherence and clarity were “substantial”, with a kappa of 0.71 (Z = 8.14, CI95%: 0.54 to 0.88, p <0.01), and 0.64 (Z = 0.88, CI95%: 0.47 to 0.81, p <0.01), respectively.
Normality of the data was verified by the Kolmogorov-Smirnov test. In order to evaluate the association and the contribution of demographic and occupational factors (ICU experience and type of work shift) to participants’ levels of emotional exhaustion, depersonalization, and personal accomplishment (dependent variables), a stepwise multiple linear regression was used. To define the variables to be included in the regression model, a Spearman’s correlation coefficient (r) was used to quantify the relationship between the total score of the burnout dimensions and the participants’ demographic (age) and occupational factors (ICU experience). Rank-biserial correlation was used to evaluate the association between dimensions of burnout and dichotomous categorical variables (i.e., sex, marital status and having children). Independent variables were included in the model if the correlation with burnout dimensions was significant (p<0.05). Considering that the “type of work shift” could also be an influential factor in the burnout dimensions, this polychotomous categorical variable was transformed into dummy variables before entering the model, as proposed by Zar [56]. The “full-time shift” category was considered as a reference for the analysis. The strength of the association was classified according to Mukaka [57], where r > 0.90 equals a very strong correlation; 0.89 to 0.70 equals a strong correlation; 0.69 to 0.50 equals a moderate correlation; 0.49 to 0.30 equals a weak correlation; and < 0.30 equals an insignificant correlation. Continuous variables are presented in mean and standard deviation (x̄ ± SD), while categorical variables are presented in frequency (%). For all analyses, the significance level was set at 5%. Analyses were performed with IBM SPSS Statistics version 25.0.
Ethics approval
The present study protocol was reviewed and approved by the Scientific Ethics Committee of the Araucanía Sur Health Service, duly accredited by the Ministry of Health of Chile (registry number 206).
Results
Demographic and occupational characteristics
Out of a total of 142 invited ICU workers, 84 completed our combined survey and were included in the study. The mean age was 30.8 ± 5.7 years and 54.8% were female. In addition, 92.9% of the participants were below 40 years old, 63.1% were single, and 69.0% reported not having children. Regarding occupational characteristics, 85.7% of healthcare workers had five or less years of experience in ICUs, 91.6% had a full-time employment contract, and 73.8% had a 4th work shift (night shift). Finally, the most frequent groups corresponded to nurses (32.1%) and nursing technicians (23.8%). Table 1 summarizes the demographic and occupational characteristics of the participants.
Burnout dimension levels
The participants’ burnout level according to each dimension is shown in Table 2 and Figure 1. The frequency of burnout syndrome in the total sample was 95.2%, and the mean total score of the Maslach Burnout Inventory for Human Services Survey was 58.7 points (CI95% = 56.3 to 61.1).
Burnour levels in each dimension according to the number of participants.
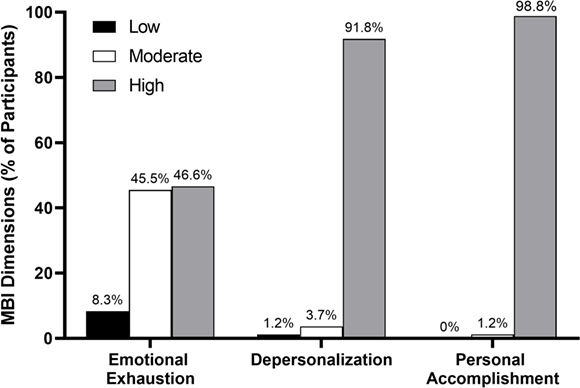
High levels of emotional exhaustion and depersonalization were observed in 39 (46.4%; CI95% = 35.8% to 57.1%) and 80 (95.2%; CI95% = 90.7% to 99.8%) of the study participants, respectively. Furthermore, low personal accomplishment was reported by 82 (97.6%; CI95% = 91.7% to 99.3%) of the participants. For details on each burnout dimension in the demographic and occupational variables, see tables S1 and S2 in the online supplementary material.
Burnout associated factors
Spearman’s correlation coefficient showed a strong and significant positive association (r = 0.72; p < 0.01) between the emotional exhaustion dimension of burnout and having children (no = 0; yes = 1). Furthermore, multiple linear regression analysis showed that having children accounted for 7% of the variation in emotional exhaustion (F1,81 = 6.49; p = 0.01; R2 = 0.10). These results suggest that having children is associated with a higher level of emotional exhaustion among ICU workers during the COVID-19 pandemic. Correlation analysis showed a significant positive association between the depersonalization dimension of burnout and age (r = 0.79; p < 0.05), sex (female = 0, male = 1; r = 0.30; p < 0.05), and prior ICU experience (r = 0.71; p < 0.05). In a multiple linear regression model, sex accounted for 6.2% of the variance in depersonalization (F1,81 = 5.35; p = 0.02; R2 = 0.10). The low personal accomplishment dimension was positively correlated with being male ("strong," r = 0.70; p < 0.05). A multiple linear regression model comprising sex (female = 0, male = 1) and type of work shift transformed into dummy variables (“Full shift” considered as reference) was significant and accounted for 14.9% of the variance in personal accomplishment (F2,80 = 7.01; p < 0.01; R2 = 0.149). Therefore, lower levels of personal accomplishment (higher burnout) was associated with being female and working at 4th shift as compared to the full-shift. See Table 3 and Table 4 for analysis details.
Discussion
The objective of this study was to determine the levels of burnout and its relationship with demographic and occupational factors in ICU healthcare workers during the COVID-19 pandemic. In this epidemiological context, a frequency of 95.2% of burnout syndrome among ICU healthcare personnel was described. In addition, 80 (95.2%) and 82 (97.6%) of participants presented high depersonalization and low feelings of personal accomplishment, respectively. The associated factors were, for emotional exhaustion, having children; for depersonalization, age, sex, and prior ICU experience; and for personal accomplishment, sex and type of work shift.
Burnout dimension levels
Regarding the emotional exhaustion dimension, our results confirm the findings of previous studies in the context of the COVID-19 pandemic [24,58,59,60]. It has been reported that between 20.4% and 67.1% of healthcare personnel had high emotional exhaustion [24,58,59,60]. Differences between studies could be explained by the time periods in which the surveys were administered. For example, Elhadi et al. [59] found that 67.1% of participants reported high levels of emotional exhaustion; however, the data were obtained during the first three months of the pandemic declaration. It is possible that the high uncertainty that accompanied the onset of the healthcare emergency [61] could have contributed to higher levels of emotional exhaustion in healthcare workers. In our study, healthcare workers were surveyed at a late stage of the first wave of the COVID-19 pandemic, which provided a context of greater epidemiological control and, consequently, with a possible attenuation in the severity of emotional exhaustion in our participants. Moreover, the high level of depersonalization found in our study (95.2%) is significantly higher than those reported in other research on ICU [23,24] and non-ICU healthcare workers [19,25] during the COVID-19 pandemic. For instance, Barello et al. [24] found high depersonalization in 24.3% of their 1153 Italian healthcare workers (nurses and physicians) [24], and Lange et al. [23] observed high depersonalization in 42.4% of 364 French physicians [23]—both studies conducted during the COVID-19 pandemic. Similarly, but also in ICU healthcare workers, Shbeer et al. in 2022 found high depersonalization in only 9.18% of 104 Saudi ICU healthcare workers [25], and Stocchetti et al. [19] observed high depersonalization in 47.8% of 136 Italian ICU healthcare workers [19].
There are some relevant methodological and logistic aspects that could explain the high percentage of depersonalization in our study sample compared to previous research. First, the study by Lange et al. defined high depersonalization as a score ≥ 12 points, and in our study the criterion for high depersonalization was a score ≥ 10 points, which could have increased the sensitivity in detecting high levels of depersonalization in our participants. Second, the presence of a copying mechanism, such as employing different workload management strategies and taking vacations in ICU healthcare workers, may have influenced the low proportion of participants with high depersonalization in the Shbeer et al. [25] study. Third, it has been shown that physicians and nurses were the healthcare personnelwith the most exposure and susceptibility to developing high levels of burnout during the COVID-19 pandemic [32]. In our study, 52% of the staff were physicians and nurses who dealt directly with infected patients and their families, which may have led to relatively higher levels of depersonalization. Another noteworthy finding of our study was the level of personal accomplishment, which was low in 98.8% of healthcare workers, which is not in line with what was reported in previous studies [24,60]. For example, only 8.4% to 15.3% of healthcare personnel reported a low level of personal accomplishment [24,60]. Luceño-Moreno et al. [60] indicated that their results could be explained by the fact that many healthcare professionals were deeply committed to patients during the pandemic, especially during the first months, as they felt valued by society and realized the great importance of their professions, positively influencing their perception of personal accomplishment [60]. On the other hand, our study was conducted in an advanced stage of the pandemic where perhaps those protective feelings of personal accomplishment were attenuated by high degrees of emotional exhaustion and depersonalization among healthcare personnel, dimensions that have proven to be critical in the magnitude of the burnout construct [62]. Additionally, the present study was conducted in a country with multiple stressors besides the COVID-19 pandemic, including social, economic, and mental health crises, which could be associated with the reported high level of depersonalization and low personal accomplishment.
Burnout associated factors
In relation to the factors associated with burnout dimensions, high emotional exhaustion was strongly and positively associated with having children, which is contrary to the findings by Claponea et al. (2021) in their systematic review of 35 studies [30]. It is reasonable to consider that ICU healthcare workers without children report lower severity of emotional exhaustion during the COVID-19 pandemic. In fact, having children and the associated higher psychological burden made it relatively difficult for ICU workers to cope with emotional exhaustion during the COVID-19 pandemic [63]. However, in our study, only 7% of the emotional exhaustion variability was due to having children. Also, a prior study found a significant association between the number of worked hours and years of experience with emotional exhaustion [59], however, our research did not find a significant relationship between these aspects.
On the other hand, in our study, high depersonalization was positively correlated with age, sex, and ICU experience. The latter is in line with that reported by Ehladi and colleagues, who observed that more experienced Libyan healthcare workers reported higher levels of depersonalization [59]. Indeed, the study by Ehladi et al. was conducted between April and May 2020 in the context of a collapsed healthcare system and a community experiencing a civil war [59], which could explain the affected attachment, personalized communication, and formality of the relationship with patients reported by healthcare personnel. Finally, in our sample, sex was strongly associated with perceived personal accomplishment. This is in line with recent systematic reviews that reported high burnout levels in female healthcare workers during the COVID-19 pandemic [22,30]. In addition, the work shift was also a contributing factor to personal accomplishment levels. Interestingly, the regression model showed that working a 4th shift led to lower levels of personal accomplishment than those working the full shift. This could be explained by the fewer rest days in 4th shift healthcare workers compared to the other shifts in our study. Furthermore, poor sleep quality and low serotonin levels in night-shift healthcare workers [64] could be factors associated with a low level of personal accomplishment.
This study has limitations to note. First, the Maslach Burnout Inventory for Human Services Survey used is an instrument not validated in Chile, which perhaps compromised the understanding of some statements of the questionnaire; however, this was minimized through cultural adaptation and content validation by an expert panel. Second, concurrent or previous psychiatric conditions, such as anxiety or depression, were not considered as potential confounding variables. Third, differences with other studies may be influenced by the lack of consensus on the burnout dimension’s cut-off definition [10]. Fourth, the sample did not represent the general population of Chilean healthcare workers, and the study was conducted late during the first wave of the COVID-19 pandemic, which may limit the generalizability of our results. Future studies should consider other ICU realities to achieve greater representativeness of the results.
Conclusions
The COVID-19 pandemic has had an overwhelming psychological impact on ICU healthcare workers. Our research demonstrates a high frequency of burnout syndrome (95.2%) and high levels of depersonalization and low personal accomplishment in ICU workers during the COVID-19 pandemic. Additionally, age, female sex, having children, ICU experience and type of work shift are factors significantly associated with burnout dimensions.

