Estudios originales
← vista completaPublicado el 30 de abril de 2024 | http://doi.org/10.5867/medwave.2024.03.2783
Association of IGF-1 and IGF-2 genotypes with respiratory muscle strength in individuals with COPD: A cross-sectional study
Asociación de los genotipos de IGF-1 e IGF-2 con la fuerza muscular respiratoria en individuos con EPOC: estudio transversal
Abstract
Introduction Chronic obstructive pulmonary disease is a systemic disease characterized not only by respiratory symptoms but also by physical deconditioning and muscle weakness. One prominent manifestation of this disease is the decline in respiratory muscle strength. Previous studies have linked the genotypes of insulin-like growth factor 1 and 2 (IGF-1 and IGF-2) to muscle weakness in other populations without this disease. However, there is a notable knowledge gap regarding the biological mechanisms underlying respiratory muscle weakness, particularly the role of IGF-1 and IGF-2 genotypes in this pulmonary disease. Therefore, this study aimed to investigate, for the first time, the association between IGF-1 and IGF-2 genotypes with respiratory muscle strength in individuals with chronic obstructive pulmonary disease. In addition, we analyzed the relationship between oxidative stress, chronic inflammation, and vitamin D with respiratory muscle strength.
Methods A cross sectional study with 61 individuals with chronic obstructive pulmonary disease. Polymerase chain reaction of gene polymorphisms IGF-1 (rs35767) and IGF-2 (rs3213221) was analyzed. Other variables, related to oxidative stress, inflammation and Vitamin D were dosed from peripheral blood. Maximal inspiratory and expiratory pressure were measured.
Results The genetic polymorphisms were associated with respiratory muscle strength ( 3.0 and 3.5; = 0.57). Specific genotypes of IGF-1 and IGF-2 presented lower maximal inspiratory and expiratory pressure (<0.05 for all). Oxidative stress, inflammatory biomarkers, and vitamin D were not associated with respiratory muscle strength.
Conclusion The polymorphisms of IGF-1 and IGF-2 displayed stronger correlations with respiratory muscle strength compared to blood biomarkers in patients with chronic obstructive pulmonary disease. Specific genotypes of IGF-1 and IGF-2 were associated with reduced respiratory muscle strength in this population.
Main messages
- To date, no studies have examined the potential association of IGF-1 and IGF-2 genotypes with respiratory muscle strength among individuals with COPD.
- The single nucleotide polymorphisms of IGF-1 and IGF-2 was associated with respiratory muscle strength in subjects with COPD.
- Individuals with AA genotype of IGF-1 and the CG and GG genotypes of IGF-2 exhibited significantly reduced respiratory muscle strength.
Introduction
Chronic obstructive pulmonary disease is a progressive airflow limitation disorder that represents the most prevalent pulmonary condition worldwide [1]. Chronic obstructive pulmonary disease is considered a systemic condition, characterized not only as respiratory symptoms but also as physical deconditioning, muscle weakness, and weight loss [2]. One common manifestation of this respiratory disease is muscle weakness, including a decline in the strength of respiratory muscles [3], which is associated with increased risk of hospitalization, dyspnea, reduced exercise capacity, and higher mortality rate [4].
Respiratory muscle weakness in chronic obstructive pulmonary disease may arise from various biological factors inherent to this disease, including oxidative stress, chronic inflammation, hormonal imbalances, and genetic factors [5,6,7]. Oxidative stress, resulting from an imbalance between pro-oxidant and antioxidant substances, is highly prevalent in individuals with chronic obstructive pulmonary disease [6]. This imbalance can contribute to muscle weakness, as oxidative stress has been linked to decreased muscle mass and strength in this population [5]. On the other hand, chronic inflammation, closely associated with oxidative stress, is another biological factor implicated in the reduction of muscle mass and peripheral strength in individuals with this disease [8].
Genetic factors also play a crucial role in the prevalence, progression, and adverse events associated with chronic obstructive pulmonary disease [9]. Some genes, such as the insulin-like growth factor (IGF) 1 and 2, have been identified as important contributors to muscle physiology, affecting both peripheral and respiratory muscle strength in studies conducted on populations other than chronic obstructive pulmonary disease [10,11,12]. The IGF-1 gene encodes the hormone IGF-1 (insulin-like growth factor 1), which plays a significant role in muscle hypertrophy, a process known to be diminished in the elderly [10,11,12]. Previous research has indicated that polymorphisms in the IGF-1 and IGF-2 genes, may be associated with decreased muscle mass and strength in young and older adults [11,12,13]. However, the potential relationship between these genes and respiratory muscle strength in individuals with chronic obstructive pulmonary disease remains unexplored. For this reason, the objective of this study was to analyze for the first time the association between IGF-1 and IGF-2 genotypes with respiratory muscle strength in individuals with chronic obstructive pulmonary disease. In addition, we aimed to examine the relationship between oxidative stress, chronic inflammation, and vitamin D with respiratory muscle strength in this population.
Methods
This was a cross-sectional study with a convenience sample of sixty-one individuals with chronic obstructive pulmonary disease from the Outpatient Physiotherapy Clinic from the University Hospital of Londrina, Paraná, Brazil. The participants were selected from institutional databases, and we employed the hospital and university’s social media platforms to broadcast information about the project. Additionally, we utilized snowball sampling techniques to reach out to colleagues and patients. Subjects were contacted via cellphone by the research team and scheduled for an interview where the study project was explained in depth. Subjects signed the informed consent, and if accepted, the evaluation was conducted at the Outpatient Physiotherapy Clinic from the University Hospital of Londrina, Paraná, Brazil. The research team recruited as many patients as possible during the period 2016 to 2019. The study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies [14]. Individuals diagnosed with chronic obstructive pulmonary disease for at least 3 years according to the Global Initiative for Obstructive Lung Disease (GOLD) criteria [1] with peripheral basal oxygen saturation> 90% were included. Individuals who had chronic obstructive pulmonary disease exacerbations, decompensated metabolic disorders in the last two months, as well as chronic respiratory failure during the data collection process and those with neurological, orthopedic, cardiovascular, or psychiatric disorders that could interfere with the performance of the test were excluded. The study was approved by the Research Ethics Committee of the State University of Londrina (N°. 1.830.048) and participants signed an informed consent form. This study complies with the Declaration of Helsinki [15].
Blood biomarkers
Peripheral blood test was performed in all individuals after 10 hours of overnight fasting. Approximately 40 mL of blood sample were obtained by venipuncture into vacuum tubes (Vacutainer®, Franklin Lakes, NJ USA) after 12 hours of fasting. The tubes were centrifuged in 2000 rpm until to separate the blood components and stored in the freezer at -80 °C until extraction time, to analyze the blood biomarkers and genetics. The serum was utilized to analyze the oxidative stress, inflammation and vitamin D and the nucleated cells (leukocytes) were separated for DNA extraction. The blood biomarkers superoxide dismutase (SOD), catalase (CAT), interleukin-6 (IL-6), tumor necrosis factor α (TNF-α) and vitamin D were analyzed according to methodology described previously [16].
Genetics
DNA was extracted from peripheral blood leukocytes which were transferred to sterile flasks and DNA was obtained after enzymatic digestion in a buffer containing proteinase K and SDS and subsequent extraction with organic solvents (phenol / chloroform). Polymerase chain reaction was performed to analyze the prevalence of the following IGF-1 (rs35767) and IGF-2 (rs3213221) single nucleotide polymorphisms according to the published literature [17]. Genotyping was carried out using Taqman according to the manufacturer’s instructions. The single nucleotide polymorphisms analyzed were adenine-adenine (AA), adenine-guanine (AG) and guanine-guanine (GG) for IGF-1 and cytosine-cytosine (CC), cytosine-guanine (CG) and guanine-guanine (GG) for IGF-2. All assays were carried out in 96-well plates. Each plate included negative controls (with no DNA) and positive controls duplicated on a separate quality control plate. Plates were read on the ABI Prism 7900using the Sequence Detection Software (Applied Biosystems).
Respiratory muscle strength
Respiratory muscle strength was assessed by measuring maximal inspiratory and expiratory pressures (MIP and MEP, respectively), assessed with a digital manovacuometer (MVD 300, GlobalMed, Brazil). The reference values used were described by previously standardized procedure [18]. The maneuvers were held for at least 2 seconds and the peak value was recorded. The best result of 3 acceptable and reproducible maneuvers was used for analysis. Respiratory muscle weakness was defined as respiratory muscle lower than 70% of the predicted value [19].
All assessments were consistently conducted by the same professional with 5 years of experience in the evaluation and rehabilitation of patients with respiratory diseases. After recruitment was completed, the genetic polymorphism analysis was carried out by the same researcher, maintaining suitable temperature and lighting conditions for the analysis.
Statistical analysis
Descriptive statistics were used to describe the demographic and clinical characteristics of the patients and other potentially confounding variables. Continuous variables were presented as the mean and standard deviation (SD), and categorical variables were presented as the number and percentage. The parametric distribution of the continuous variables was checked using both the Shapiro-Wilk test and graphical procedures (normal probability plot). To investigate the association between both inspiratory and expiratory pressures (as main variables) with blood biomarkers and genetic biomarkers, age and gender (as explanatory variables) a regression analysis was performed with the general linear model (GLM). The GLM was performed to inspiratory and expiratory muscle strength separately in univariate analysis, and maximal inspiratory and expiratory pressures in multivariate analysis (presented as respiratory muscle strength in Table 2). The overall multivariate Wilks’ Lamda, F-test, partial eta-squared and confidents intervals for regression coefficients were analyzed. ANCOVA analysis was used to compare the different genetic polymorphisms in respiratory muscle strength variables, adjusted for age and gender. Statistical significance was considered as p<0.05 with a 95% confidence interval (95% CI). Statistical analyses were performed using the software IBM SPSS 22 (SPSS Inc., Chicago, IL, USA).
Results
The baseline and demographic characteristics are presented in Table 1. A total of 70 individuals were enrolled, but 61 completed all measurements, including the DNA extraction. The single nucleotide polymorphism of IGF-1 indicates a higher percentage of GG genotype (52%) and lower percentage of AA (5%). In the single nucleotide polymorphism of IGF-2, GG has a higher percentage (43%) and CC has a lower percentage (23%).
Table 2 shows the association between biological factors and respiratory pressures in two models: In the univariate model, respiratory pressures were analyzed separately. Maximal inspiratory pressure was associated with single nucleotide polymorphism of IGF-2 (F = 5.6 and p = 0.007) and IGF-1 (F = 5.4 and p = 0.008), age (F = 5.2 and p = 0.028) and gender (F = 24.5 and p = <0.001). Maximal expiratory pressure was associated with the single nucleotide polymorphism of IGF-2 (F = 4.7 and p = 0.014) and gender (F = 24.8 and p = <0.001). In addition, we analyzed both maximal inspiratory and expiratory pressures in a multivariate analysis. In this model we analyzed only the biological factors that were associated with the pressures separately in univariate analysis (IGF-1 and IGF-2, age and gender). Factors associated with respiratory muscle strength were single nucleotide polymorphism of IGF-2 (F = 3.5 and p = 0.01), IGF-1 (F = 3.0 and p = 0.024) and gender (F = 18.4 and p = <0.001); R2 = 0.57 and partial eta-squared from 0.13 to 0.21. The regression coefficients and the 95% confidence intervals are presented in Table 3. Maximal inspiratory pressure was negatively associated with AA genotype of IGF-1 (coeff= -43.2; CI 95%= from -69.3- to -17.1; p<0.001) in the adjusted model 2. The CC genotypes of IGF-2 was positively associated with both inspiratory and expiratory pressures in the model 1 (raw analysis) and 2 (adjusted by age and gender) (coeff from 26.5 to 39.1).
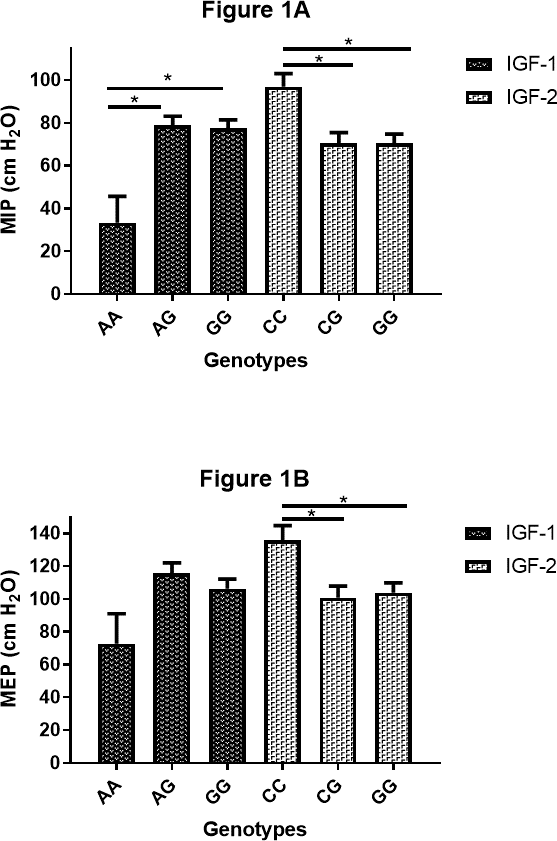
The comparative analysis of respiratory muscle strength among individuals with chronic obstructive pulmonary disease, considering the genotypes of the genes IGF-1 and IGF-2 is presented in Figure 1. This analysis was adjusted by age and gender. The IGF-1 AA genotype (Mean ± SD= 33.38 ± 12.3 cmH2O) showed lower maximal inspiratory pressure when compared to AG (Mean ± SD= 78.86 ± 4.29 cmH2; MD= -45.5; CI 95%= -77.6 to -13.4; p=0.03) and GG (Mean ± SD= 77.47 ± 3.93 cmH2O; MD= -44.1; CI 95%= -76.4 to -11.8; p=0.04) The IFG-2 CC genotype (Mean ± SD= 96.89 ± 6.23 cmH2O) exhibited higher maximal inspiratory pressure compared to CG (Mean ± SD= 70.44 ± 4.98 cmH2O; MD= 26.4; CI 95%= 6.2 to 46.6; p=0.006) and GG genotypes (Mean ± SD= 70.45 ± 4.35 cmH2O; MD= 26.4; CI 95%= 7.4 to 45.4; p=0.004). Similarly, the IFG-2 CC genotype (Mean ± SD= 135.97 ± 8.81 cmH2O) presented higher maximal expiratory pressure compared to CG (Mean ± SD= 100.86 ± 7.05 cmH2O; MD= 35.1; CI 95%= 6.5 to 63.7; p=0.011) and GG genotypes (Mean ± SD= 103.82 ± 6.15 cmH2O; MD= 32.2; CI 95%= 5.3 to 59.1; p=0.014).
Respiratory muscle strength in individuals with chronic obstructive pulmonary disease with different genotypes.
Discussion
In the present study, we conducted a comprehensive analysis to examine, for the first time, the influence of IGF-1 and IGF-2 genotypes on respiratory muscle strength in individuals with chronic obstructive pulmonary disease. Our results demonstrated that the IGF-1 and IGF-2 single nucleotide polymorphisms exhibited stronger associations with respiratory muscle strength compared to blood biomarkers in individuals with this respiratory disease. Specifically, the AA genotype of IGF-1 and the CG and GG genotypes of IGF-2 were found to have a negative impact on respiratory muscle strength in individuals with chronic obstructive pulmonary disease. In addition, CC genotype of IGF-2 is associated with more respiratory muscle strength. These novel findings provide valuable insights into the association between the IGF-1 and IGF-2 genes and respiratory muscle strength in this population.
The IGF-1 gene, located on chromosome 12, encodes the hormone IGF-1, which plays an important role in muscle physiology [11,20]. Genetic polymorphisms are significant determinants influencing levels of insulin-like growth factor [21]. Previous studies have consistently reported that low levels of insulin-like growth factor are closely associated with muscle weakness and poor physical performance [10,11]. Moreover, the IGF-1 rs35767 polymorphism has been specifically linked to decreased muscle strength [11,12,13,22]. In our study, individuals with chronic obstructive pulmonary disease with the AA genotype exhibited significantly lower respiratory muscle strength compared to those with the G allele (AG and GG). Notably [21], recently observed a strong association between AA genotype an the prevalence of metabolic diseases and inflammatory biomarkers [21]. Metabolic disorders and chronic inflammation are well-established factors that contribute to oxidative stress, ultimately resulting in muscle atrophy and reduced protein synthesis, thereby promoting muscle weakness and sarcopenia [23,24].
Additionally, specific SNPs within the IGF-2 gene, such as the SNP rs3213221 have been found to be correlated with various markers of muscle damage and weakness, such as greatest strength loss, highest muscle soreness, and greater creatine kinase and myoglobin response after exercise [13]. A study conducted by [13] further demonstrated a strong association between the CC genotype and enhanced capacity for muscle hypertrophy and higher muscle strength [13]. Despite our study was conducted on a different population compared to previous research [11,12,13,22], we observed consistent results regards CC genotype, which exhibited greater respiratory muscle strength. Although most of the studies in this field have not been specifically conducted on individuals with chronic obstructive pulmonary disease [11,12,13,22], it is reasonable to hypothesize that reduced levels of the insulin-like growth factor caused by the polymorphisms of the IGF-1 and IGF-2 may affect respiratory muscle strength, as these polymorphisms have been associated with muscle function.
While associations between certain blood biomarkers and muscle mass or peripheral strength have been reported in individuals with chronic obstructive pulmonary disease [25], these associations have not been extensively studied in relation to respiratory muscles. It is widely recognized that oxidative stress, systemic inflammation, and hormonal imbalances are closely linked to various comorbidities in individuals with this disease [5,6,7]. However, despite the fact that these biomarkers have been associated with worse pulmonary function [17], there remains a significant knowledge gap concerning respiratory muscle strength. It is plausible to hypothesize that respiratory muscles may be influenced by distinct biological factors compared to peripheral muscles in individuals with chronic obstructive pulmonary disease. The presence or reduction of these biological biomarkers in the blood may be insufficient to elicit changes in respiratory muscle strength when compared to the impact of genetic factors, given the substantial genetic influence observed in individuals with this pulmonary disease [9,26]. These findings suggest that genetic variables, independent of the inflammation and oxidative stress commonly observed in chronic obstructive pulmonary disease, exert an influence on respiratory muscle strength and may affect the prognosis and quality of life of patients with this condition. For this reason, the study of genetic variables should be considered to better comprehend the state and changes in muscle function. Additionally, the classification of genotypes could be valuable in identifying specific subgroups of individuals with chronic obstructive pulmonary disease who require personalized clinical interventions, particularly those with the AA (IGF-1), CG, and GG (IGF-2) genotypes, as they exhibited lower muscle strength [27].
While the results of this study are encouraging, it is important to acknowledge several limitations. Firstly, the small sample size consisting of individuals classified as GOLD I and IV restricts the generalizability of the findings and their extrapolation to other individuals with this respiratory condition. Secondly, the lack of control for confounding factors inherent in observational studies, such as concomitant interventions like medication usage and comorbidities, may have led to some overestimation of the results. Lastly, the absence of medium or long-term follow-up hinders the determination of potential changes in outcomes and how biomarkers may be associated with respiratory muscle weakness over time. Despite these limitations, it is worth highlighting the strengths of this study, which include the utilization of gold standard techniques for outcome assessment and the incorporation of various blood and genetics tests reported in the literature. Furthermore, this study stands out as one of the few that examines the relationship of these factors using these methods. However, not all biomarkers and biological pathways related to muscle mass and function were explored. Hence, future research is warranted to corroborate these findings and investigate additional genetic and blood biomarkers. As a future perspective, it would be important to carry out additional types of research, such as longitudinal studies with long-term follow-up, to determine their implications on long-term prognosis and the potential development of genetic therapies or interventions.
Conclusions
In conclusion, our study represents a pioneering investigation into the association of IGF-1 and IGF-2 genotypes with respiratory muscle strength in individuals with chronic obstructive pulmonary disease. The results revealed that the single nucleotide polymorphisms of IGF-1 and IGF-2 displayed stronger correlations with respiratory muscle strength compared to blood biomarkers in patients with chronic obstructive pulmonary disease. Specifically, the AA genotype of IGF-1 and the CG and GG genotypes of IGF-2 were associated with reduced respiratory muscle strength in this population. In addition, CC genotype of IGF-2 is a protective factor for respiratory muscle strength. These novel findings shed light on the relationship between the IGF-1 and IGF-2 genes and respiratory muscle strength in individuals with this respiratory disease, providing valuable insights into the underlying genetic factors influencing this aspect of muscle function. The early identification of these genotypes could be used to generate interventions to prevent functional alterations and carry out a more specific early treatment.

