Estudios originales
← vista completaPublicado el 11 de noviembre de 2024 | http://doi.org/10.5867/medwave.2024.10.2939
Comportamientos preventivos del COVID-19 en Chile: lecciones de un seguimiento poblacional en 2021 y 2022
Preventive behaviors for COVID-19 in Chile: Lessons from a population follow-up for 2021 and 2022
Abstract
Introduction The rapid emergence of COVID-19 urged policy responses worldwide, focusing on vaccination and mobility restrictions. Chile represents a unique scenario for analyzing personal preventive measures amid intensive communication and vaccination campaigns. This study aims to explore changes in population adherence to non-pharmacological preventive measures during the pandemic and the factors that explain this adherence each year.
Methods 386 individuals who participated in two population-based studies (2021 and 2022) were considered. An interview was conducted to measure adherence to self-care practices, and case and contact tracing by the health authorities. The Wilcoxon signed-rank test was performed to measure change between 2021 and 2022, bivariate analysis, and a linear regression model for each year were performed.
Results Mask-wearing in public places was the most commonly used measure (95.9% in 2021, 89.9% in 2022). Follow-up of cases and cases contacts by the health authority had high coverage in 2021 (94.3% and 83% respectively). A greater decrease was observed in contact tracing in 2022 totaling 33.3%. An increase in the score of adherence to preventive practices was observed in 2022 (p < 0.00). The regression model showed in 2021 that women were more likely to adopt preventive behaviors (95% confidence interval: 0.27 to 1.13) and the overweight/obese had higher adherence compared to normal body mass index (95% confidence interval: 0.06 to 0.98). In 2022 being a young adult (30 to 49 years) predicted the adoption of behavioral precautions (95% confidence interval: 0.00 to 1.32).
Conclusions Adherence to preventive measures increased even with high vaccination coverage, likely due to the epidemiological situation with the Omicron variant circulating in 2022.
Main messages
- This is the first population-based serial study carried out in two Chilean cities during the pandemic that assesses changes in adherence to non-pharmacological preventive measures against COVID-19 and factors that explain adherence in the context of a high vaccination rate.
- Adherence to non-pharmacological preventive measures increased from November 2021 to April to May 2022.
- Women and overweight/obese in 2021, and young adults (30 to 49 years) in 2022 were more likely to adopt precautions.
- Preventive behaviors were self-reported and may be affected by recall and social desirability bias.
Introduction
dDuring the COVID-19 pandemic, individual preventive actions and community involvement played a crucial role in reducing transmission, especially when vaccines were not yet available [1].
These actions included the use of personal protective equipment like masks and practicing hand hygiene, environmental measures such as disinfection and improving ventilation, maintaining social distancing in public places, school closures, and imposing travel restrictions [2]. Facemasks was one of the main individual preventive practices to reduce COVID-19 transmission [1,3]. Additionally, quarantine was an effective intervention to reduce virus transmission, as demonstrated in Wuhan, where its early and strict application significantly reduced the reported cases [4]. One study indicated a 35% reduction in COVID-19 incidence with classroom ventilation measures [5], though assessing ventilation independently is complex [6].
Non-pharmacological interventions are challenging as they require changes in personal behavior. However, a scoping review that explored the efficacy of behavioral non-pharmacological interventions on COVID-19 outcomes concluded that combining such measures and its early implementation can significantly reduce infections and transmission of COVID-19 [7].
The implementation of these measures varied based on the epidemiological situation of the disease and the political guidelines of each country, as well as the public adherence to the recommendations from authorities [8]. Adoption of preventive measures depends on the population’s knowledge [9] and individual perception of disease risk. Studies show that individuals with low-risk perception are less likely to follow preventive measures [10], while those with chronic diseases have higher adherence [11].
The World Health Organization (WHO) has provided recommendations according to the epidemiological stage of the disease. Currently, some recommendations persist due to the endemicity and epidemic cycles of SARS-CoV-2. These WHO guidelines focus on individual health protection and preventing the spread of the disease including maintaining a physical distance of at least one meter, wearing masks when physical distancing is not possible and, in poorly ventilated environments, frequent handwashing, covering the mouth and nose with the elbow or tissue when coughing or sneezing, and isolating positive cases [12].
Upholding these preventive measures is a challenge even with the availability of vaccines [13], due to the emergence of new SARS-COV-2 variants reducing vaccine effectiveness and the lack of prevention in mild infections, as well as low vaccination coverage [14,15].
Variations in adherence to non-pharmacological measures have been described throughout the pandemic, due to vaccination, decreased risk perception, or pandemic fatigue [16,17,18]. In Chile, the Ministry of Health followed up COVID-19 patients and their contacts during the pandemic. A study in Chile showed a decrease in compliance with some non-pharmacological measures in the post-vaccination stage in 2021. However, the 2020 evaluation (pre-vaccination) performed by Varas was done retrospectively in 2021 and may be affected to recall bias [19]. No studies in Chile have measured adherence to non-pharmacological measures during the vaccination stage, especially with the implementation of booster doses for the entire population. Understanding adherence to non-pharmacological measures for COVID-19 is critical as evidenced by the 16% increase in SARS-CoV-2 infections in Chile in November 2021 [20].
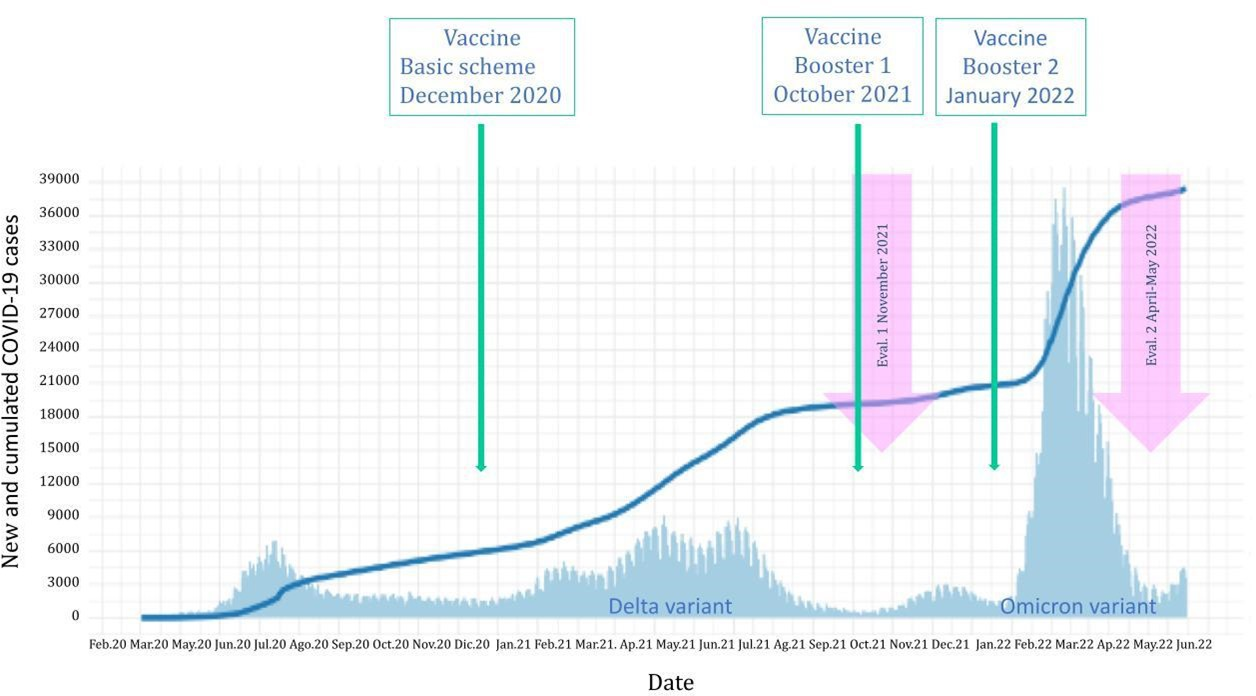
This research aims to explore: 1) changes in public adherence to non-pharmacological measures across two distinct stages of the COVID-19 pandemic, using a cohort from 2021 to 2022 in a country with high levels of vaccine coverage and, 2) the factors explaining adherence at the two times measured. We hypothesize that there was a decrease in non-pharmacological measures adherence as the pandemic and vaccination progressed. The first stage in 2021 coincided with the completion of the basal vaccination schedule and the circulation of the Delta variant. Conversely, the second stage in 2022 took place amidst the implementation of vaccine boosters and the circulation of the Omicron variant [5] (November 2021 and April-May 2022). Epidemiological characteristics of the pandemic in Chile in these two years were different regarding the population affected, variant circulation, and vaccine schemes offered to the population (Figure 1).
Epidemiological characteristics of COVID-19, Chile 2021-2022.
The analysis of behavioral changes over time and the identification of factors that influence compliance with non-pharmacological measures provide a deeper understanding of how individuals respond to health crises like the COVID-19 pandemic. This study is particularly relevant in the context of vaccine rollouts and booster implementations, as it highlights the ongoing importance of non-pharmacological measures even in the presence of pharmacological interventions. The findings from Chile, which has closely followed WHO recommendations and achieved high vaccination rates, offer a unique perspective on the effectiveness of these strategies. Understanding these dynamics is crucial not only for managing the current pandemic but also for preparing for future health emergencies. By learning from these patterns of adherence, we can develop more effective approaches to prevent and mitigate the impact of new disease outbreaks, ensuring a more resilient public health response in the future.
Methods
Study design and setting
This is a serial cross-sectional study performed in two moments. We studied 386 individuals aged seve years or older who participated in three serial seroprevalence studies against SARS-CoV2 between 2020 and 2022 in two cities located in the central zone of Chile: Coquimbo-La Serena and Talca. Random sampling stratified by census districts was carried out in two stages: first block (random selection) and second home (systematic jump).
Participants
All household members aged seven years or older were invited to participate.
Sample size
Sample size calculation was done based on population sizes of 200 000 people in Talca and 500 000 in La Serena-Coquimbo, with an expected variance of 50%, considering a 95% confidence interval and 5% error. The sample size needed was 384 individuals in each location. In the two cities, the minimum sample size was exceeded in all three stages.
Variables
Independent variables were the sociodemographic and health characteristics. Dependent variables were the self-care measures. Self-care measures were assessed at home by a structured interview in the second (November 2021) and the third round (April-May 2022) using the same core questionnaire. The questions in 2021 and 2022 included frequency of (a) hand washing; (b) avoiding handshakes, kisses, or hugs; (c) ventilating the environment where you are; (d) mask usage in public places, and (e) mask use with people outside of household members. In addition, three other questions were used differently in each round to capture different stages of the recommendations defined by the health authority (adherence to curfew and compliance with mobility restrictions evaluated in 2021, and physical distancing of at least one meter evaluated in 2022). The self-care measures questionnaire was validated through expert judgment [21]. The Institutional Review Board of the Universities in the two cities approved serial prevalence studies. Participants signed an informed consent, and the children signed an assent.
Statistical methods
To describe the results, the following scoring was considered for the answers of the five questions measured in both years: never = 0; rarely = 1; frequently = 3, and always = 4 ranging from 0 to 20. The total score was evaluated continuously with central tendency and position measures. Changes in adherence scores were analyzed using a non-parametric test (Wilcoxon signed-rank test). To analyze frequency and score of preventive measures all responses available were considered for each category and year. Therefore, the number of participants varies because not all of them answer every question. Additionally, we evaluated whether there was contact tracing from the health authority for isolation following a COVID-19 diagnosis and quarantine for being a close contact.
Finally, non-parametric bivariate analyses with the Wilcoxon rank sum test (Mann-Whitney) were performed for variables with two categories, and Kruskal-Wallis for variables with three or more categories. Those variables with a p-value <0.10 in any of the two years measured were included in a linear regression model for each study time, with a confidence level of 95%. The linear regression model was performed for participants with complete data for the variables included (n = 341). It should be noted that the following variables changed between study rounds: in-person work, healthcare worker, episodes of illness, number of episodes, COVID diagnosis, symptomatology, comorbidity, and vaccine dosage. Also, the Body Mass Index category of underweight was discarded given the low number in the bivariate analysis.
Results
In our sample, 52.3% were residents of Talca and 67.4% were women. The median age was 49 years (interquartile range: 33 to 64). 85.8% were covered by public health insurance, and 9.6% identified as belonging to an ethnic group. 53.3% of people aged 18 and over completed secondary education and 22.2% have completed professional education.
During the 2021 evaluation, 35 individuals had a positive COVID-19 diagnosis and 88 in 2022. Regarding contact tracing, the health authority contacted 94.3% in 2021 and 81.8% in 2022 to assess isolation status (reduction of 13.3%). Among the participants who were advised to remain in quarantine for being in contact with a COVID-19 positive case, 83.0% were contacted by the health authority to assess quarantine compliance in 2021 and 33.3% in 2022 (reduction of 60.3%) (Table 1).
In 2021, the prevention practices that participants indicated they "always" performed were wearing masks in public places (95.9%), complying with step-by-step mobility restrictions (95.1%), and adhering to curfew (94.6%). For the 2022 assessment, wearing masks in public places and wearing masks with people outside of household member (89.9% and 90.7%, respectively) showed also high frequency. However, the measures with lower levels of high compliance were wearing masks with people outside the household (55.3%) and avoiding greetings with handshakes, kisses, or hugs (61.4%), the latter also having the lowest frequency for 2022 (59%). The only measure that was individually related to the COVID-19 diagnoses was the ventilation of closed spaces (p = 0.01), people who rarely ventilated spaces presented the disease in a higher proportion, compared to those who ventilated frequently or often (Table 2).
Figure 2 illustrates the transitions in the public’s adoption of non-pharmacological measures to prevent the spread of COVID-19 in each individual in the dataset.
Evolution of preventive measures adopted by the population followed from 2021 to 2022.
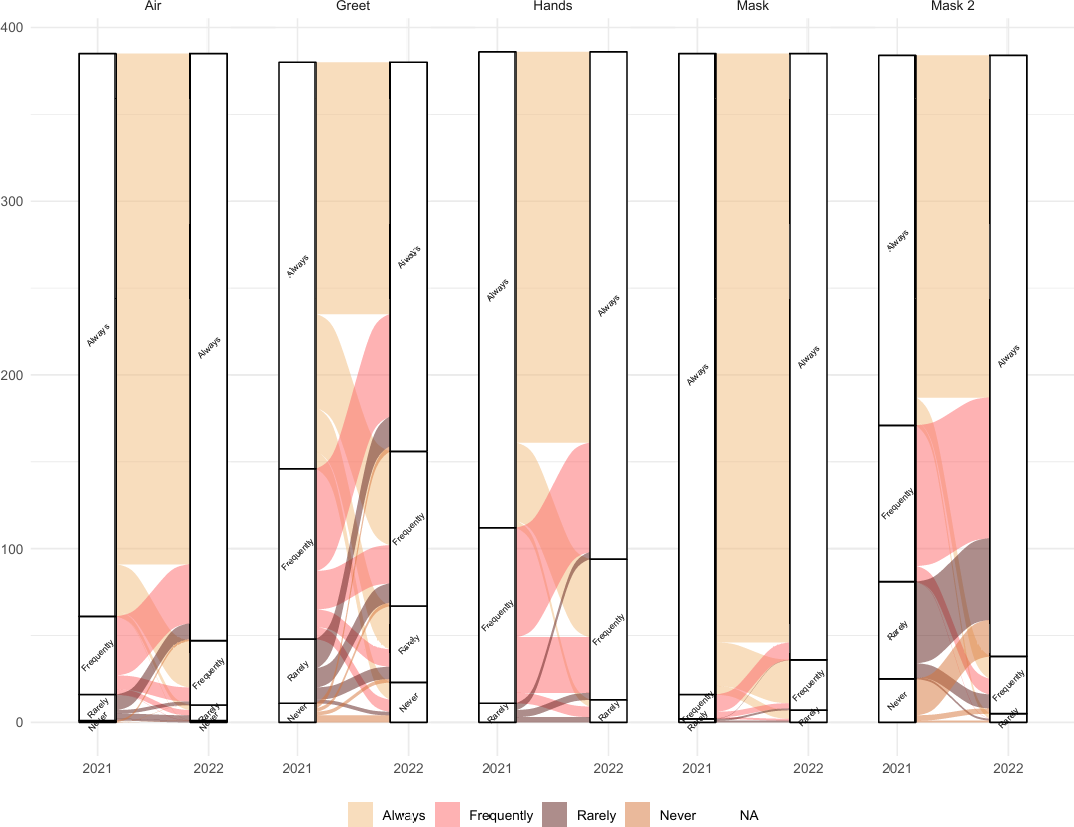
Source: Prepared by the authors based on the results of the study.
From left to right, ventilation of closed spaces (Air) also maintained a high adherence, with a noticeable shift from 'always' to 'frequently' and an increasing number of participants moving from 'frequently' or 'rarely' to 'always'. On the other hand, greeting behaviors (Greet) exhibit the most heterogeneous changes. While there’s a general trend toward reducing physical greetings, the shift across categories is minimal, suggesting a gradual change in social greeting habits over the two periods. Handwashing habits (Hands) show that an important number of individuals who previously washed 'always' shifted to 'frequently'. However, a significant portion of the 'frequently' group either maintained their habit or elevated it to 'always'. Notably, a few individuals who 'rarely' washed hands in 2021, transitioned to 'always' in 2022. The pattern for mask use (Mask) with non-household members is interesting, as only a small fraction reduced their usage, while a substantial number increased their usage across all levels, with some going from 'never' to 'always'. Finally, mask-wearing in public spaces (Mask 2) is observed to be the most consistently adopted measure with negligible transitions between the two years.
The result of the score for the five questions repeated each year of the study showed that 46.1% of the participants improved preventive practices, 29% maintained them and 24.9% decreased their adherence. The Wilcoxon signed-rank test showed a change in preventive practices, with a statistically significant increase in the score (z = -5.17; p-value < 0.00) from 2021 to 2022 (data not shown). The bivariate analysis between the study variables and preventive practices score showed significant differences by cities in 2021, given that the city of Coquimbo-La Serena presented a lower median score for preventive practices. In the 2022 evaluation, the score improved, equaling Talca. Similarly, in the 2021 assessment, men were observed with a lower median score, which subsequently increased and equaled that of women. For both years, it was observed that the age groups of 7 to 19 and 20 to 29 years presented lower scores in contrast to the other ages. In 2022, the age groups under 30 to 49 years old increased the score. However, in those over 50 years old, no changes in the median were observed. In 2021, a higher score was observed in people who had overweight and obese Body Mass Index, nonetheless, the difference was marginal (p-value = 0.06). That situation was not present in 2022 where the score was equal. In both years a higher score was observed in those with some comorbidity. Likewise, differences were observed depending on the dose of vaccine administration for each round. For both years, having one or two more doses of vaccines administered the score of non-pharmacological measures was higher. Additionally, unvaccinated individuals increase their scores for 2022. For further details, see Table 3.
The results of the multiple linear regression model are presented in Table 4. Gender predicted preventive practices in 2021 (95% CI: 0.27 to 1.13), but in 2022 was marginal (95% CI: -0.00 to 0.70). In the year 2021, the Body Mass Index of overweight/obesity was 0.52 higher than the Body Mass Index normal (95% CI: 0.06 to 0.98). In 2022, the factor that explained the preventive practices score was age 30 to 49 years, which showed a 0.66 higher score compared to the 7 to 19 years age group (95% CI: 0.00 to 1.32).
Discussion
The score of adherence to recommended non-pharmacological measures against SARS-CoV-2 increased from 2021 to 2022. Being a woman, overweight and obese was associated with a higher score in 2021. In 2022, being a young adult (30 to 49 years) was predictive of the use of non-pharmacological measures. The proportion of COVID-19 cases isolated by the health authority decreased from 94.3% in 2021 to 81.8% in 2022. There was a high contactability for a contact of confirmed COVID-19 cases and cases in both years, except for contact in 2022, where the reduction was 60.3%, because of changes in the follow-up strategies for contact tracing due to the high incidence rate at that time.
In our study, 46.1% of participants improved their adherence to non-pharmacological measures during the pandemic period, while 29% maintained them. A study conducted in Thailand found that, upon the implementation of vaccination, adherence improved by 12 to 18% in social activity avoidance, physical distancing, and hand washing (in 2021 and 2022), which is lower than in our study. Moreover, the proportion of individuals who maintained preventive measures was 70 to 90%, higher than in our study [22]. Another study in Israel showed that mask usage was maintained at 75.7%, and social distancing at 48.8%. However, the proportion showing improvement was only 3.2% for mask use and 4.3% for social distancing [23]. Unlike the studies mentioned above, our study did not specifically hypothesize changes in adherence due to vaccination, as the first measurement of preventive behavior was conducted in 2021 when basal scheme coverage was at 80%. In 2022, coverage of the basal scheme exceeded 90%, and 60% of the population received one or two boosters [24]. Thus, we observed that despite the increase in vaccination coverage, adherence to preventive measures was higher, similar to findings reported in the Wright et al. study in the United Kingdom [25].
On the one hand, several studies have indicated that non-pharmacological measures reduced the incidence of COVID-19 [26,27]. In contrast, between the two periods in which we measured adherence to non-pharmacological measures, the incidence of COVID-19 reported by the Chilean Ministry of Health increased [28,29,30]. This increase could be attributed to the arrival of the Omicron variant in Chile in December 2021, noted for its rapid transmissibility and mutational capacity. Therefore, associated with a potential for immune escape [31] which triggered Omicron to quickly become the dominant circulating variant [32]. In this context, the increased risk perception among the Chilean population may have contributed to greater adherence to the preventive behaviors reported in this study, especially since the study was conducted during a new epidemic wave.
Mask use in public places was the behavior with the highest adherence in both 2021 (95.9%) and 2022 (89.9%). Indeed, some studies have found that mask use is the measure with the highest adherence [8,15]. One study reported a mask use proportion of 81.9% between 2020-2022 and also noted an increase in the likelihood of its use when mandatory [33]. Although it was the measure with the highest adherence, we observed a slight decrease in the proportion of use by 2022, differing from Petherick et al., who reported an increase in adherence to mask-wearing over time. However, their study was conducted in the first year of the pandemic when awareness was higher [17]. Additionally, when analyzing the relationship between preventive measures and having contracted COVID-19, ventilating the home was the only measure that showed a statistically significant association, but only in 2022. Those who ventilated less frequently had a higher proportion of the disease [17]. This reinforces the notion that air is the main mode of transmission of this disease, making this behavior effective in preventing COVID-19 [34]. Avoiding greetings with handshakes, kisses, or hugs remained with low adherence compared to the other measures asked at both times of the survey, which may be due to cultural practices in Chile. A study in Ethiopia showed a similar proportion to the second wave of our study (53.8%) [35].
In 2021, women were the key explainers of the score for non-pharmacological measures, exhibiting higher adherence than men. Regarding the adoption of protective masks and attitudes towards respiratory epidemics, a pre-COVID-19 study found that women were more inclined to adopt non-pharmacological measures such as wearing masks, washing hands, and avoiding public transportation [13]. Gender, followed by age, had a strong association with mask use [36]. Studies from various countries have demonstrated that men adhere less to preventive behavior, being less likely to use face masks, wash their hands, and more likely to breach rules of physical distancing and isolation [37]. In our study, during the first measurement, adults (over 30 years of age) had the best score; in the second measurement, all age groups under 50 years improved their score, with the best score observed in adults aged 30 to 49 years. This change in preventive behavior has been indicated in other studies as well [37]. This could be attributed to the fact that this demographic is more likely to be working and commuting, hence more aware of the importance of health precautions.
In the bivariate analysis, we found significant differences between cities. In 2021, Coquimbo presented a lower score than Talca. This may be due to structural determinants of health such as poverty; La Serena/Coquimbo has an 11.8% income poverty rate, while Talca has 8% [38]. These factors could affect the ability to purchase masks and necessitate working outside the home. Additionally, having comorbidity was significantly associated with higher adherence to non-pharmacological measures, likely due to an increased perception of disease risk [39], similar to a U.S. study showing that adults with comorbidities were more likely to adhere to preventive measures [11]. Lastly, those who complied with the administration of more vaccine doses were always more adherent to preventive measures, demonstrating a coherent attitude towards prevention [40,41]. A high proportion of COVID-19 cases and contacts were followed up in both 2021 and 2022 by the health authority. Although it was lower in 2022, probably due to the two to three times higher frequency of COVID-19 cases [28,29,30], prioritizing cases follow-up over contacts [42]. In January 2022, the Chilean Minister of Health delegated the responsibility for contact tracing to individuals with COVID-19 [43].
The limitations of this study include that preventive behaviors were self-reported and may be affected by recall and social desirability bias, although interviewers were trained to minimize it. This study was not intended to measure risk perception which could have changed due to Omicron variant circulation and new risk communications strategies implemented by the new health authorities in 2022. Additionally, weight and height were self-reported, which may lead to a sub or under-estimation of obesity because people tend to have a distorted self-perception of their body [44]. This misclassification is non-differential, and the estimates may be biased to null values [45]. The strength of this research is that it includes a population-based sample with an adequate response rate (63%). Therefore, the study findings generalized to territories with similar characteristics. The same individuals were studied cross-sectionally at two different times allowing for the follow-up of participants under fluctuating epidemic conditions.
Conclusions
Public health measures intended to minimize the spread of infectious diseases are essential, even in the presence of vaccination. Regarding our hypothesis, we conclude that adherence to non-pharmacological measures did not decrease as the pandemic progressed and vaccination rates increased. Despite high vaccination coverage, we found greater adherence in two measurement moments during the pandemic. Mask-wearing was the most utilized measure, characterized by high acceptability and relatively low cost compared to vaccines. Health authorities should improve adherence among the whole population, not only those most at risk, with special priority given to those less likely to adhere. Encouraging men and young people to adhere to preventive measures should be emphasized in risk communication strategies. Simultaneously, it is necessary to continue researching to better understand the factors that predict and enhance adherence to preventive behaviors.

