Estudios originales
← vista completaPublicado el 23 de enero de 2025 | http://doi.org/10.5867/medwave.2025.01.2946
Resultados quirúrgicos, sobrevida y factores pronósticos de una cohorte de pacientes con cáncer pulmonar operados en el Hospital Clínico de la Universidad de Chile
Surgical outcomes, survival and prognostic factors in a cohort of lung cancer patients operated at the University of Chile Clinical Hospital
Abstract
Introduction Lung cancer is the leading cause of death by cancer worldwide and has a high lethality. The best treatment for patients with localized disease is anatomical surgical resection, granting good average survival in the long term. We did not find Chilean studies focusing on complications, long term survival or potential association with pathological or clinical factors. The aim of this work is to describe clinical characteristics, surgical complications and 5-to-10-year survival of a cohort of lung cancer patients operated in the Clinical Hospital of University of Chile and explore possible prognostic factors influencing in it.
Methods A 107 patient’s cohort of operated lung cancer patients in a single center from 2004 to 2015 was analyzed. We included patients with curative intent surgery performed in our hospital and excluded non- primary lung cancer histology or biopsies analyzed in other center. Clinical, perioperative and histopathologic data were collected. 5-10 year overall survival was determined and an exploratory analysis of prognostic factors on survival was performed.
Results We found 107 surgeries fulfilling criteria, with 27% morbidity and 5.6% and 6.5% mortality at 30 and 90 days, respectively. 5- and 10-year overall survival was 44.7% and 32.3%, respectively. Univariate analysis found that gender, age, histology, disease stage, loco-regional dissemination and postoperative complications were factors associated with survival. Multivariate analysis confirmed that gender, age, loco-regional dissemination and postoperative complications were independent factors associated with survival.
Conclusions Surgical results of a cohort of patients operated in a Chilean center show that 30 and 90-days mortality aligned with data reported worldwide. Overall survival in these selected patients is far better than reported in lung cancer patients. Risk factors that may be screened in preoperative analysis were found, which could change prognosis. Those findings suggest that improving preoperative evaluation could optimize patient selection to obtain better performance in surgical results and overall long-term survival.
Main messages
- Lung cancer is highly lethal in Chile and Latin America.
- Surgery is the best strategy to increase survival in early stages, but it has high morbimortality rates, and there are very few data on its results in Latin American countries.
- In this study, we show the long-term survival and clinical characteristics of a cohort of 107 lung cancer patients who were operated with curative intent.
- Some limitations of this work are the insufficient number of cases for some variables, a potential risk of bias due to the sample size of convenience sampling, and the possible underreporting of variables such as smoking.
Introduction
Lung cancer is the leading cause of death from lung cancer worldwide [1] and has a high lethality, which translated into a five-year survival of 10 to 20% for cases diagnosed in the period from 2010 to 2014 [2]. In Chile, as of 2018, it is the leading cause of cancer death, with a crude mortality rate of 18.4 per 100 000 population in 2021, displacing gastric cancer (crude rate of 15.4 for the same year) [2,3,4]. It is a consensus that one of the best alternatives for a patient with localized non-small cell lung cancer is surgical treatment. Generally, this involves anatomic lung resection (pneumonectomy, lobectomy, or segmentectomy) plus lymphadenectomy, eventually followed by chemotherapy or radiotherapy [4]. The morbimortality of this type of surgery, which is not free of complications both in the short and long term, has decreased notably in recent years, especially in developed countries. This is probably due to a better preoperative study and patient selection, the appearance of new surgical techniques, and the general improvement of anesthetic and postoperative care [5]. Surgery (when deemed appropriate for the patient) is considered the procedure of choice in stage 1 and 2 non-small cell lung cancer, being an exceptional option in stage 3 [4]. However, these surgical procedures should be preceded by an extensive clinical, functional, and imaging evaluation to determine the patient’s cardiopulmonary status and surgical resectability [6]. When the surgical risk outweighs the benefits, other ablative alternatives, such as exclusive radiotherapy (stereotactic or traditional) or a combination with systemic treatment (chemotherapy or targeted therapies), can be chosen [4].
Both surgery and immediate postoperative management are highly complex processes and are ideally performed by well-trined teams with the appropriate technological equipment [7]. In Chile, although there are few detailed studies, one performed in a cohort of patients confirmed with non-small cell lung cancer between 2007 and 2011 found that only 34% of patients were diagnosed in stages 1 and 2 [8], while another cohort between 2010 and 2019 did so in 13.7% of cases. In that cohort, resective surgery could be performed in only 14.7% of patients [9]. Lung cancer in 2019 began to be covered by the General Regime of Explicit Health Guarantees. This health regulatory instrument implemented in Chile in 2005 guarantees access, timeliness, quality, and financial protection in providing services for 85 prioritized health problems by 2024 [10].
To our knowledge, there are no published studies on complications and long-term survival after surgical treatment in Chilean health centers in patients operated on with curative intent. In this context, the present work aims to describe the clinical characteristics and perioperative complications, including 30 and 90-day mortality, and five and 10-year survival of a cohort of patients operated on at the Hospital Clínico de la Universidad de Chile (a university hospital in the Metropolitan Region). We also explore prognostic factors that may influence long-term survival in this cohort, specifically age, sex, histology, stage, level of regional spread, and the presence of postoperative complications.
Methods
The present study corresponded to a retrospective, observational cohort design. A cohort of 107 patients operated on for primary non-small cell lung cancer with curative intent between 2004 and 2015 in our institution was analyzed. The database analyzed corresponds to a registry of patients initiated in 2004, where 176 patients evaluated by the thoracic surgery team of our center were incorporated. Inclusion criteria were considered to be all patients operated on with curative intent, regardless of whether this could be completed. Exclusion criteria were: biopsy processed in another center where the pathologic stage and histologic variety could not be known (16 patients excluded); histology other than primary lung cancer (41 patients excluded); and those patients operated with non-curative objectives (12 patients excluded).
Clinical variables at diagnosis were recorded in the database: age (in years), sex (assigned at birth, male or female), comorbidities (self-reported hypertension, diabetes mellitus 2, coronary heart disease, chronic obstructive pulmonary disease, pulmonary fibrosis, and others), smoking, and clinical staging with brain, chest and abdominal CT scans. Smoking habit was quantified with the index of cigarette packs per year, which reports the number of packs of cigarettes smoked in a lifetime. An index of one implies one pack (20 cigarettes) per day for one year. Tumor staging was performed based on the 7th or 8th edition of the Tumor, Node, Metastases (TNM) system of the International Union Against Cancer [11]. The investigators retrospectively updated this to the 8th version [12] when appropriate. The date of surgery was also noted.
In addition, some operative variables were retrospectively recorded by electronic chart-based follow-up. These variables were the type of approach (thoracotomy or minimally invasive surgery), type of resection (lobectomy, pneumonectomy, segmentectomy, bilobectomy, sleeve lobectomy, wedge resection, unresected and other), type of lymph nodal resection (sampling, lobe-guided lymphadenectomy or mediastinal lymphadenectomy), operative time in minutes, complications according to severity (Clavien-Dindo classification), and hospital stay in days.
The histological types were determined according to the World Health Organization (WHO) 2021 classification [13], and the histological subtypes according to that proposed by the International Association for the Study of Lung Cancer (IASCL), the American Thoracic Society (ATS) and the European Respiratory Society (ERS) [14].
The date of death was determined using data from the Civil Registry and Identification Service, and 30- and 90-day mortality was also recorded. Overall survival was estimated from the date of surgery to August 31, 2020 (the date of completion of follow-up for this study) or to the date of death in the case of deceased patients. The specific cause of death was not recorded, as this information was not available from the Civil Registry and Identification Service.
Our primary response variable was the time between surgery and death or the last follow-up date. We performed an exploratory analysis of possible prognostic factors based on predictor variables of interest (sex, age, histology, regional dissemination, complications, and package index per year) according to clinical criteria, quality, and number of cases of the information recorded. Therefore, relevant clinical variables such as comorbidities had to be excluded from this analysis.
First, a descriptive univariate analysis of the absolute frequencies of the variables of interest was performed. Secondly, the survival curve was estimated using the Kaplan-Meier method, considering the period between the surgery date and the death or last follow-up. The comparison of different groups (tumor classification, metastasis dissemination, and histological types) was performed using the log-rank test. A Cox regression model was used to evaluate potential prognostic factors. The proportional hazards assumption was checked using graphical visualization and a proportional hazards test. The following prognostic variables were included in the univariate model: sex, age, histology (recategorized into adenocarcinoma, low-grade carcinoid, squamous and undifferentiated), stage, level of regional dissemination (N0, N1, and N2 or N3) and presence of complications (dichotomous variable yes/no). The Hosmer - Lemeshow screening criterion was applied (i.e., starting by fitting a model with all variables with significance level p < 0.25 in the univariate analysis) [15], in addition to expert clinical judgment.
Data processing and statistical analysis were performed with R studio version 4.0.2 and Stata v16 software.
This work was approved by the Scientific and Human Research Ethics Committee of the Hospital Clínico Universidad de Chile.
Results
A total of 107 patients underwent surgery at our institution between 2004 and 2015 who met the inclusion criteria: 52 men (48.6%) and 55 women (51.4%). The median age was 63 years (range 20 to 82 years). The most frequent comorbidities were arterial hypertension (24.2%), chronic obstructive pulmonary disease (13%), and type 2 diabetes mellitus (9.4%). Of the total number of patients, 13 (12.5%) had a previous diagnosis of another cancer, of which one was a previous lung cancer. In addition, 70 patients had a smoking habit (defined as more than 100 cigarettes in a lifetime; 65.4%), either active or quit. The clinical presentation of the patients was asymptomatic in 30.8% of cases. Of the symptomatic patients, 29.2% consulted for cough. The characterization of the patients is presented in Table 1.
The main surgical approach (Table 2) was thoracotomy, with 90 surgeries performed by this route (84.1%) and 17 with minimally invasive techniques (15.9%). Of these, three were converted to open surgery (17.6%). The first minimally invasive surgery was performed in 2012. Of the type of resections performed, 85 were lobectomies and bilobectomies (78.4%), eight pneumonectomies (7.5%), seven anatomic segmentectomies (6.5%), and nine others (8.4%). Of the total, 29 patients (27.1%) presented postoperative complications (Table 3), of which 11 were major (Clavien-Dindo type III: 5, IV: 6). A total of 7 patients were reoperated (6.5%). The median hospital stay was 8.6 days. Mortality at 30 days was 5.6% (6 patients), and at 90 days, 6.5% (7 patients). tables 2 and 3 detail the surgical aspects and postoperative evolution of the patients in the series.
Table 4 shows the clinical and pathological stages determined after surgery. Of the total number of patients, three were classified as stage 0 (2.8%), 37 as stage I (41.8%), 35 as stage II (32.7%), 31 as stage III (28.9%) and one as stage IV (0.9%). The most frequent histological types (Table 5) were adenocarcinoma (48.6%) and squamous carcinoma (31.8%). Details of the staging (clinical and pathological) and histology of the patients are presented in tables 4 and 5.
The overall survival of the cohort of operated patients was 44.7% (95% confidence interval: 36.2 to 55.3) at 5 years and 32.3% (95% confidence interval: 23.7 to 44.2) at 10 years (Figure 1).
Overall survival of lung cancer patients with surgical treatment.
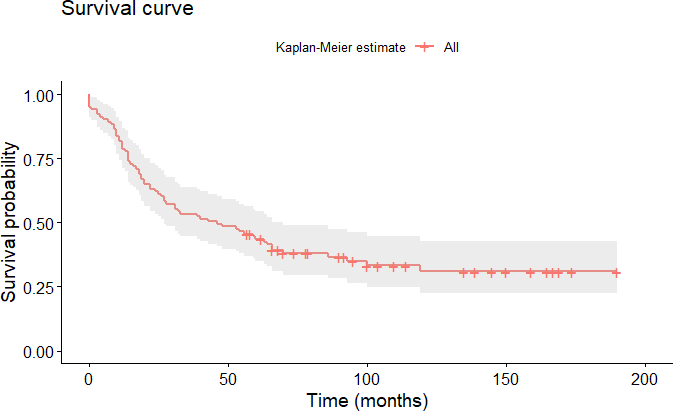
Source: Prepared by the authors based on the study results.
Significant differences were observed in the survival of patients according to their sex, as well as in the histologic variety, the pathologic stage of the tumors, and the presence of postoperative complications. According to the pathological stage at the time of surgery, overall survival at five years was 100% for patients in stage 0 (n = 3), 60.4% in stage I (n = 37), 37.7% in stage II (n = 35), 28.1% in stage III (n = 31) and 0% in stage IV (n = 1).
Figure 2 shows the survival curves by sex, histology, stage (excluding stage 0 and IV), and postoperative complications.
Overall survival of operated patients according to pathologic stage.
(
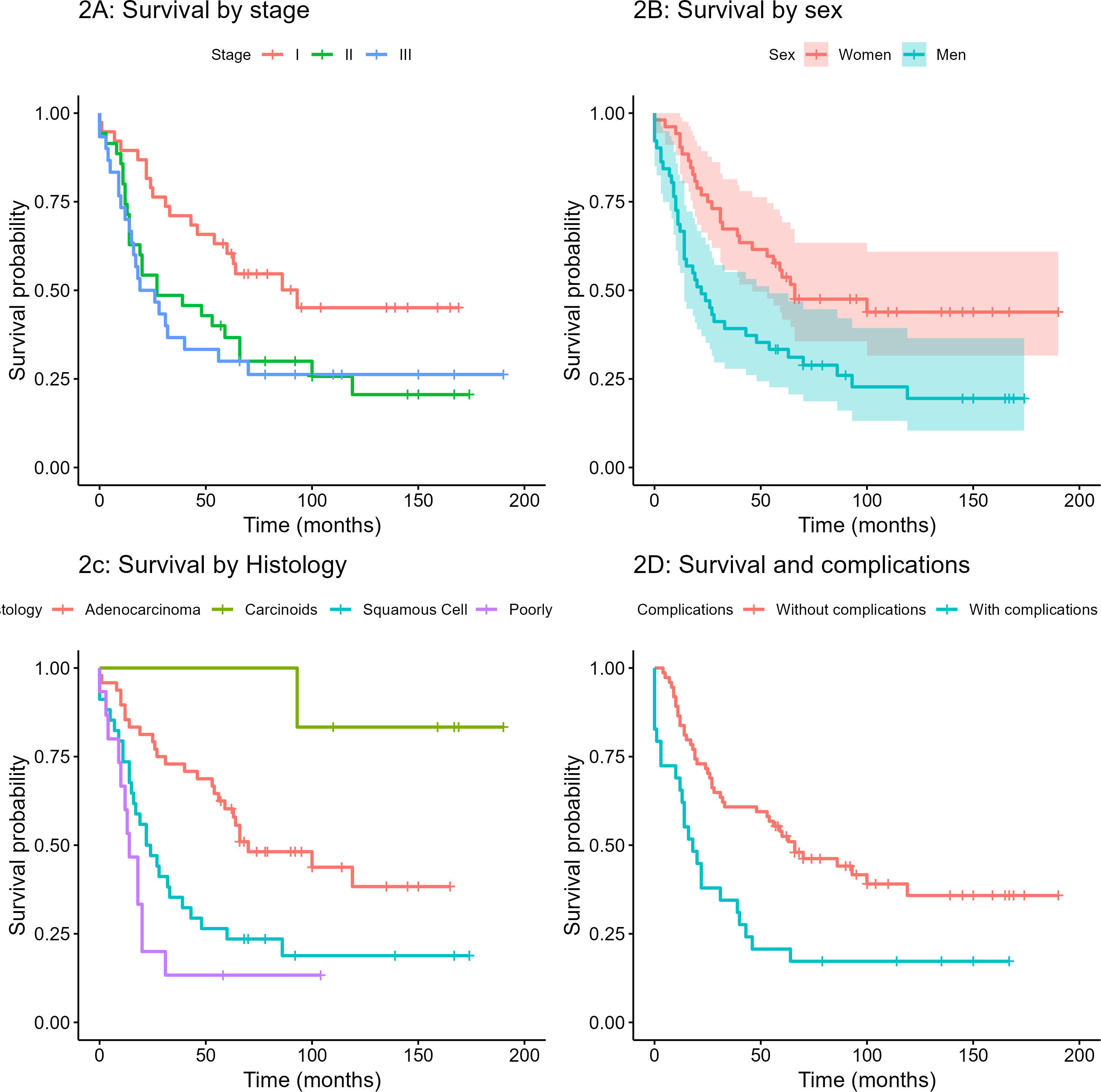
The univariate analysis (Table 6) found that, of the factors explored, those that could affect survival were sex, age, tumor histology, stage of disease, level of regional dissemination, and the presence of postoperative complications.
Multivariate analysis (Table 7) confirms that sex, age, regional dissemination level, and postoperative complications are independently associated with survival.
Discussion
In this work, we present the surgical results and long-term survival of a cohort of patients operated on for lung cancer with curative intent at the Hospital Clínico de la Universidad de Chile. Our findings allow us to report an overall survival of 44.7% at five years, as well as a 90-day mortality of 6.5% after surgery. In addition, we characterized the patients in relevant clinical and surgical aspects, including tobacco exposure, clinical presentation, hospital stay, complications, and perioperative mortality.
Surgery with curative intent for lung cancer, which most of the time involves a major lung resection, is a procedure with high morbimortality and prolonged postoperative stay. In our series, more than 90% of the surgeries were lobectomy or even major resection, and 90-day mortality exceeded 5% (similar to that described in other international series) [16,17], and major complications are seen in more than 25% of patients. Although an important component of morbidity and mortality is related to comorbidities [18], other factors are linked to the magnitude of lung resection and unexpected intraoperative (or early postoperative) complications [19]. Our study shows that the presence of complications is an independent factor that worsens the 5-year survival of the patients studied. For example, in the first years of this study, our center did not have the carbon monoxide diffusion test or the cardiopulmonary test. Both tests are widely used in preoperative evaluations [20]. Preoperative cardiopulmonary rehabilitation of patients was also not widely used, which could be a cause of the relatively high frequency of complications and postoperative mortality. This should motivate surgical teams to make a more meticulous selection of patients who undergo this type of surgery.
Concerning survival, in Chile, the existing cancer population registries have estimated survival rates in patients with lung cancer in the range of 5.5% at five years and 3.8% at 10 years in the period from 1998 to 2012 [21]. The superior survival rates observed in our study (although lower than in other international studies where five-year survival rates of up to 57.5% have been reported [22]) would be related to selecting patients with a better prognosis when operated with curative intent. Indeed, other studies in Chilean centers have documented survival rates of 46.1% at three years [8], including non-resective surgery. Other Chilean series have documented 5-year survival rates of 20.1% for non-small cell lung cancer [9]. In the latter series, survival showed a great improvement in patients who underwent surgery with curative intent (71%), although follow-up was calculated differently, and the patient groups were not comparable [9]. At the international level, there is also consistency in our results with other series of patients, although extrapolation is limited. For example, the potential negative association (the lower the level of dissemination, the longer the survival) between survival and the level of regional dissemination (hilar or mediastinal lymph nodes) in surgical outcomes has been reported previously [16], as has the association between male sex and certain histologies (non-adenocarcinoma) with worse prognosis [22]. Although the number of patients is too few (which manifests itself in wide confidence intervals) to make more conclusive analyses, the association is statistically significant in multivariate analysis and is clinically relevant. This is especially noticeable concerning the level of regional dissemination.
In the anatomo-pathological study of the samples, some new trends observed in international studies [23] are appreciated, such as the predominance of adenocarcinomas and the appearance of small tumors, even smaller than one centimeter, minimally invasive, or non-invasive. It is noteworthy that almost 40% of the operated patients were stage 1, which generally corresponds to imaging findings. This aligns with the intensive use of chest computed tomography in the study of cardiopulmonary diseases [24] and also highlights that more than 30% of patients were staged at stage 3, mostly due to lymphonodal involvement of the mediastinum. Lymphonodal involvement was the most relevant factor when assessing long-term survival, which aligns with what has been reported in the international literature [25].
As previously mentioned, it is relevant to highlight that at the time of surgery in the center in question, these patients did not have advanced non-invasive (positron emission tomography-computed tomography) or invasive (mediastinoscope or endobronchial ultrasound) methods of mediastinal evaluation. In recent years, staging with positron emission tomography-computed tomography as a minimum has become standard and the criteria for invasive staging [26]. This makes it necessary to highlight the importance of hospital cancer registries and their continuity over time to help evaluate the new strategies implemented and case management in hospitals [27].
Finally, it should be noted that most centers that manage lung cancer at the national level do not have methodologies for evaluating the mediastinum or specific instruments for measuring cardiopulmonary capacity. This is very relevant, given that the ministry guidelines included in the Universal Access with Explicit Health Guarantees plan for lung cancer are being updated [28].
Our study has several limitations:
-
Since the cause of death was not available, we report overall survival, which is not directly attributable to cancer.
-
The number of patients is low for some of the analysis categories, which had to be regrouped according to clinical criteria. For the same reason, some potential predictor variables were not included in the analysis, such as the presence of comorbidities.
-
In this study, we did not determine a sample size. We used convenience sampling [29] since it corresponds to all registered cases of patients who opted for curative surgery in this center. These patients may have definite characteristics that select them for such a procedure (for example, less associated comorbidity) and particular socioeconomic characteristics not registered that may motivate their care in our center, generating a potential selection bias of the patients studied. However, we intend to describe this cohort of patients rather than generalize the results.
-
Relevant variables such as the cigarette pack-year rate were inconsistent with what was expected (lower survival the higher the pack-year rate), so it was not included in the multivariate analysis. This could suggest an underreporting of smoking in our registry (for example, other reports indicate the presence of smoking in up to 86% of patients [8]).
Despite these limitations, the present study allows us to report the surgical results observed in a cohort of 107 patients operated on with curative intent with a follow-up of more than 10 years, findings not previously reported in our country. This may motivate similar studies, allowing us to account for differences in the evolution after surgery in different establishments and analyze changes over time in these characteristics. The progressive inclusion of diagnostic tests allows for a better selection of patients and improved surgical technique after the period analyzed. All these elements could modify post-surgical mortality and reduce its complications, increasing survival.
Conclusions
In summary, this work shows that surgical treatment of lung cancer in a Chilean university center is capable of achieving higher survival rates than those reported for patients with lung cancer in general, and this may be due to a selection of patients with better prognosis. Given the mortality at 30 and 90 days, a systematic cardiopulmonary function study and a more intensive staging (particularly for regional N2 dissemination) may improve discrimination of patients with a higher preoperative risk.
In this sense, it is essential that centers treating lung cancer in Chile (and, by extension, in other Latin American countries) incorporate technologies such as the carbon monoxide lung diffusion test, cardiopulmonary test, positron emission tomography-computed tomography, along with endobronchial ultrasound to optimize results and improve the use of resources.

