Estudios originales
← vista completaPublicado el 27 de diciembre de 2024 | http://doi.org/10.5867/medwave.2024.11.2961
Factores asociados a mortalidad materna en Ica, Perú: estudio de casos y controles pareados
Factors associated with maternal mortality in Ica, Peru: A matched case-control study
Abstract
Introduction Maternal mortality remains a significant challenge for public health globally, particularly in developing areas such as Ica, Peru. This study aims to analyze the risk factors contributing to maternal mortality in reference hospitals in Ica during the period of 2010 to 2020.
Methods A case-control study was conducted, including 49 cases of maternal deaths and 98 controls, applying multivariate logistic regression to analyze data collected from hospital records.
Results The absence of a partner (adjusted OR: 12.3; 95% CI: 2.6 to 58.8), history of anemia (adjusted OR: 5.8; 95% CI: 1.5 to 21.3), delays of more than two hours in accessing medical care (adjusted OR: 10.2; 95% CI: 2.0 to 51.1), and lack of knowledge of warning signs such as unrecognized vaginal bleeding by companions (adjusted OR: 7.4; 95% CI: 1.2 to 46.7) were associated with an increased risk of maternal mortality.
Conclusions The identification of these factors highlights the urgent need to develop comprehensive strategies that optimize access to maternal health services and strengthen education on warning signs. To reduce preventable maternal mortality, it is essential to collaborate between the Ministry of Health of Peru and regional governments, aiming to expand coverage and improve the quality of prenatal care. Additionally, awareness should be increased and transportation availability ensured 24 hours a day for women experiencing obstetric complications. The main limitation of this study is the generalization of results due to the regional focus and exclusive use of hospital data.
Main messages
- This study identifies critical risk factors for maternal mortality in Ica, Peru, such as absence of a partner, history of anemia, and delays in access to medical care.
- The main findings of this study provide a basis for designing interventions to reduce maternal mortality and improve maternal health policies and practices.
- This study highlights health disparities and specific challenges contributing to the global maternal mortality debate.
Introduction
Maternal mortality remains a critical public health problem worldwide, especially in developing countries such as Peru. Each year, approximately 295 000 women die due to complications related to pregnancy and childbirth, and the vast majority of these deaths occur in low- and middle-income countries [1,2].
The leading causes of maternal mortality are obstetric hemorrhage (27.1%), preeclampsia and eclampsia (14%), sepsis (10.7%), and complications of childbirth (9.6%) [3]. These deaths are mostly preventable with appropriate and timely health interventions [4]. The Global Strategy for Women’s, Children’s and Adolescents' Health (2016 to 2030) and the Sustainable Development Goals (SDGs) aim to reduce the maternal mortality ratio to less than 70 per 100 000 live births by 2030, highlighting the urgent need for effective interventions [1,5,6,7].
The maternal mortality ratio in low-income countries in 2020 was 430 per 100 000 live births, compared to 13 per 100 000 live births in high-income countries [8]. This disparity highlights global inequalities and inequities within countries, mainly affecting low-income women and those in rural areas [4,9]. In Peru, the increase in maternal deaths in 2020, 42.1% more than in 2019, underscores the need for urgent action [10].
The Ica region has seen a notable increase in maternal mortality in 2019 and 2020, especially during the COVID-19 pandemic in 2021 [11], highlighting the importance of investigating these factors in detail. This study analyzes the sociodemographic, obstetric, and knowledge factors that contribute to maternal mortality in the Ica region from 2010 to 2020 to provide evidence to support the design of effective interventions and public policies that can significantly reduce maternal mortality in the region.
Methods
The study used a matched case-control design in three referral hospitals in the province of Ica, Peru, from 2010 to 2020. This approach was carefully selected due to its efficacy in identifying risk factors, allowing a retrospective comparison between women who died from obstetric complications (considered as cases) and those who survived similar complications (defined as controls). Controls were matched to cases based on place of residence and year of hospital admission to minimize bias and ensure a valid comparison.
The study setting included the Hospital Regional de Ica, Hospital IV EsSalud Augusto Hernández Mendoza, and Hospital Santa María del Socorro. These hospitals served as referral centers in the Ica region, comprising five provinces: Chincha, Pisco, Ica, Palpa, and Nasca. The recruitment and data collection periods spanned from 2010 to 2020, in which all maternal deaths and severe obstetric complications treated at these centers were recorded. These hospitals provide medical services to the population of these areas, making them an ideal setting to investigate maternal mortality. This design is efficient and appropriate for the study’s objectives, but it also reduces bias and improves the results' validity.
In this study, participants were carefully selected to ensure the validity of the results. Forty-nine cases of maternal deaths were included out of a total of 72 reported by the epidemiological surveillance system of the regional health directorate of Ica. However, 23 cases were excluded due to incomplete medical records and referrals from other regions. For the controls, 98 women who survived severe obstetric complications in the same hospitals and during the same period were chosen for the cases recorded, maintaining a 2:1 ratio with the cases.
Specific ineligibility criteria were established for both groups. Women who died from accidental or incidental causes unrelated to pregnancy, those with incomplete medical histories, patients referred from hospitals in neighboring regions and those whose obstetric complications derived from elective surgical interventions unrelated to obstetric emergencies were excluded.
The selection of cases and controls was meticulously designed to ensure that any differences in outcomes were due to the risk factors studied and not to variations in medical care. Matching by place of residence and year helped to minimize selection bias by ensuring that the sociodemographic conditions of cases and controls were comparable.
In this study, the main dependent variable is maternal mortality, defined according to the criteria established by the World Health Organization (WHO) [12]. This variable constitutes the primary outcome of interest in the study.
The independent variables include a series of factors that could influence maternal mortality. These variables are classified into different categories to assess their impact on maternal mortality.
The mother’s age was classified into two groups: younger than 35 years and older than or equal to 35 years. The cohabitation relationship is analyzed, differentiating between women with a partner and without a partner, to investigate how social support might influence health outcomes. The educational level is classified into primary/secondary and tertiary to analyze how this factor might affect pregnancy management and the use of maternal health services.
The quality of prenatal care was assessed by the number of prenatal checkups, which is classified as a discrete variable due to its count nature. Controls are categorized into "adequate" (with eight or more visits) and "inadequate" (fewer than eight visits), following WHO recommendations [13].
The residence is classified as urban or rural to assess possible differences in pregnancy management and access to maternal health services. A delay in access to medical care is defined as a delay of more than two hours to receive care at a referral hospital after the onset of an obstetric complication. The place of delivery is recorded, i.e., whether it occurred in a health facility or outside of it.
In addition, referral to a higher-complexity hospital is assessed, defined as the referral of a patient from a lower-complexity clinic or facility to a higher-level hospital. This variable determines whether the patient can access specialized services and key resources. Referral to a higher complexity hospital is recorded as a dichotomous variable, with "yes" or "no" categories, depending on whether or not the patient was referred to a higher complexity hospital.
For the study, standardized methods of evaluation and comparability are applied to ensure accuracy and consistency in the results. Data were obtained from hospital records and structured interviews with family members and health personnel, using questionnaires explicitly designed for this purpose. These questionnaires were validated through a peer review process, which ensures their consistency and relevance for assessing factors associated with maternal mortality. In addition, clear criteria were defined for selecting cases and controls, and a standardized data coding and recording system was implemented to reinforce the quality and consistency of the information collected.
Data collection staff received specific training to mitigate potential bias, and a matched design was employed to minimize selection bias. Data from the interviews were cross-checked with hospital records to reduce reporting bias. The study sample was selected by nonprobability sampling, including cases and controls, adequately representing the population of interest in the region.
As for the treatment of quantitative variables, these were grouped into specific categories to facilitate statistical analysis, as in the case of the age variable, which was classified into those under 35 years of age and those 35 years of age or older. Multivariate logistic regression was used to evaluate the associations between the variables and maternal mortality, ensuring an adjusted and accurate analysis.
Data collection was implemented in two phases: in the first phase, an exhaustive review of medical records and hospital records was performed, identifying clinical characteristics, medical history, and obstetric complications of the patients, guided by a standardized protocol. In the second phase, structured interviews were conducted with relatives of the deceased and the health personnel who attended them to complement the information extracted from the medical records. These interviews, applied to both cases and controls, used a data collection instrument designed specifically for this type of study [14].
This questionnaire was validated through a rigorous review process by maternal health and epidemiology experts, ensuring its relevance, clarity, and accuracy for analyzing factors associated with maternal mortality. During the piloting phase, five experts evaluated each questionnaire item in terms of sufficiency, coherence, and relevance, following the methodology of Escobar-Pérez and Cuervo-Martínez [15]. Only those items that achieved a content validity index (CVI) equal to or higher than 0.78 were included in the final version.
Cohen’s Kappa index was calculated to measure agreement among experts, obtaining a value of 0.82 (95% CI: 0.76 to 0.88), representing substantial agreement according to the Landis and Koch scale [16]. Items that did not meet the required thresholds of validity or agreement were revised and adjusted or eliminated, resulting in a final instrument with high reliability adapted to the needs of the study.
Several critical factors were considered to control for confounding variables. The frequency of prenatal checkups was included because of its potential influence on the early detection of complications. In addition, maternal health conditions, including hypertension and gestational diabetes, were assessed for their significant impact on pregnancy. Current pregnancy management, which could influence pregnancy management and outcome, was also considered.
Regarding the selection of variables, the frequency of prenatal controls, maternal health conditions, and current pregnancy management were considered potential confounders. Potential interaction between key variables was assessed during the initial exploratory analysis. These variables were adjusted in multivariate logistic regression models to minimize bias and ensure the validity of observed associations.
Missing data management was addressed by listwise exclusion, eliminating cases with missing data on key variables for analysis. This approach was adopted due to the low amount of missing data, ensuring representative and robust results.
The study design used a matched case-control approach, with a ratio of two controls to each case to maximize statistical power. Matching was performed using a frequency approach, ensuring that the distribution of controls mirrored that of cases in age groups (<35 years and ≥35 years) and place of residence. This method controlled for possible confounding due to these variables, ensuring valid comparisons.
For the collection of data on "warning sign knowledge," multiple strategies were implemented to minimize reporting bias. Interview staff were trained to ask questions neutrally, and standardized questionnaires were used to ensure consistency. In addition, responses were cross-checked against medical records when possible, and interviews were conducted in multiple sessions to allow for reflection and accuracy of responses. These measures helped to improve the quality and reliability of the data, although the results should be interpreted with caution due to the indirect nature of the information source.
Key study variables were defined and operationalized, including frequency of prenatal controls, maternal health conditions, and current pregnancy management. These variables were detailed to ensure accuracy and clarity in the presentation of results.
Several strategies were implemented to address potential sources of bias in the study. Appropriate case-control matching was used to mitigate selection bias, ensuring no significant differences in key variables such as age and place of residence. This approach allowed for more valid comparisons between the groups studied.
Thorough data verification was done by triangulation of multiple sources to reduce reporting bias. This included reviewing hospital records and conducting interviews to ensure the consistency and accuracy of the information collected.
In terms of controlling for confounding variables, three potentially confounding variables were identified and adjusted for in multivariate logistic regression models: frequency of prenatal checkups, maternal health conditions (including hypertension and gestational diabetes), and current pregnancy management.
Current pregnancy management was assessed by considering factors such as delayed access to medical care, place of delivery, referral to higher-complexity hospitals, and access to medications. These factors were carefully adjusted in the analyses to minimize bias and ensure the validity of the associations observed in the study.
This study considered age as a possible effect modifier in the observed associations. Although a comprehensive analysis of effect modifiers was not performed, the importance of exploring these interactions in future work is recognized. Age may influence susceptibility to certain risks due to biological or behavioral changes. To address this, an interaction analysis between age and risk factors could be conducted, which could uncover crucial differences in the effects of risk factors among various population groups. This could facilitate the design of more effective and personalized interventions.
Regarding the categorization of variables, the study employed clinical and statistical criteria to optimize the interpretation and comparison of the results. Sociodemographic, obstetric, and knowledge variables were categorized as follows: age was divided into two categories, under 35 years and 35 years or older, to reflect important differences in the risk of maternal mortality. Cohabitation relationship was coded into two categories, "with a partner" and "without a partner". These categorizations allowed a more precise analysis and highlighted the most relevant associations between the variables and maternal mortality.
Results
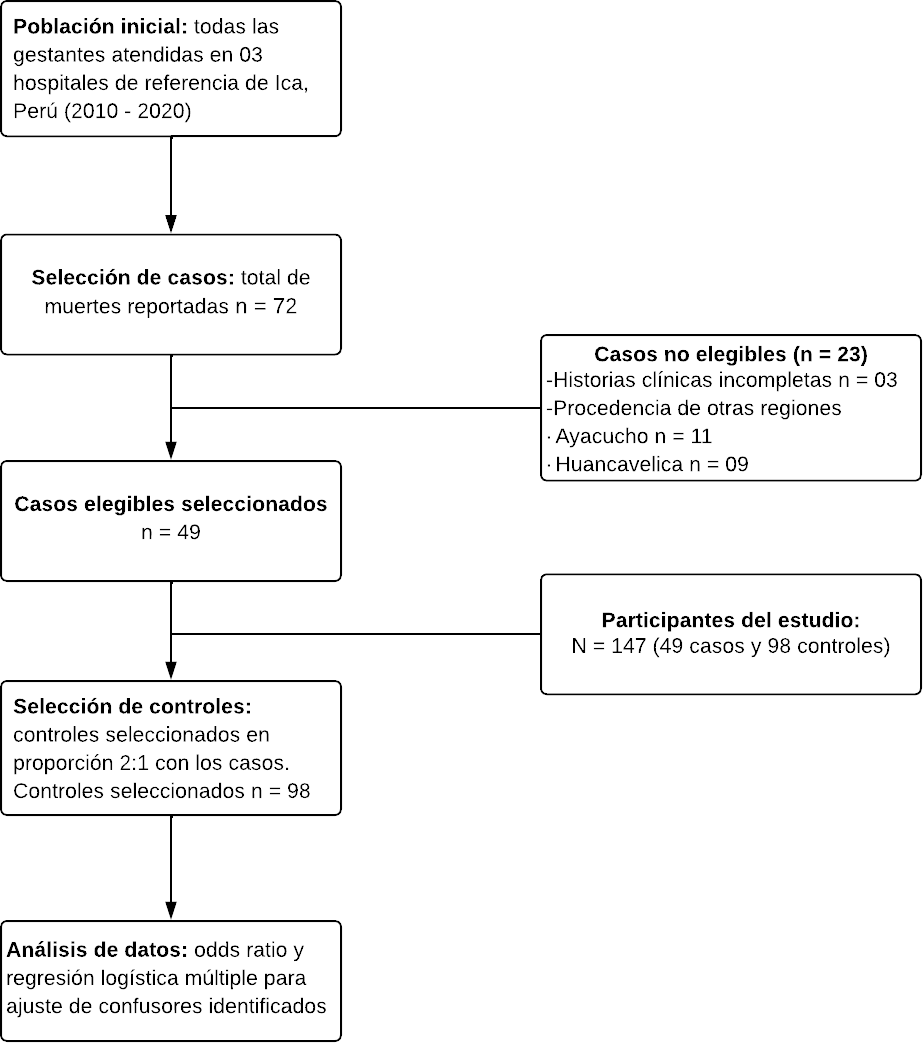
Between 2010 and 2020, the Ica region registered 72 maternal deaths, of which 49 cases were included in this study along with 98 controls, maintaining a ratio of one case for every two controls. Of the 23 excluded cases, three did not have a complete medical history, while 20 corresponded to patients referred from provincial hospitals in neighboring regions (11 from Ayacucho and nine from Huancavelica) who arrived in critical condition for specialized management (Figure 1).
Flow diagram of the case and control selection process in the maternal mortality study in Ica, Peru (2010-2020).
Analysis of the sociodemographic characteristics of the population studied (Table 1) revealed that 67% of the women were younger than 35, with the majority (61%) between 20 and 34. Regarding marital status, 56% (81 women) were single or without a partner. Regarding origin, most were from the provinces of Ica (42.9%), Pisco (22.4%), Chincha (20.4%), Nasca (10.2%) and Palpa (4.1%). It is important to note that the percentages presented for the causes of maternal mortality were calculated concerning the total maternal deaths within each subgroup (direct and indirect).
Table 2 shows the sociodemographic factors associated with maternal mortality in the referral hospitals of the Ica region during the period 2010-2020. Bivariate analysis indicated that the absence of a partner was significantly associated with an increased risk of maternal mortality, presenting an odds ratio (OR) of 4.8, with a 95% confidence interval (95% CI) of 2.3 to 10.2 and a p-value of less than 0.001. No significant associations were found between maternal mortality and age or educational level variables.
As shown in Table 3, a history of anemia was significantly associated with an increased risk of maternal mortality, with an odds ratio of 3.0, a 95% confidence interval of 1.4 to 6.3, and a p-value of 0.003. Other obstetric antecedents, such as parity and inter-gestational period, did not significantly correlate with maternal mortality.
Table 4 shows that uterine atony is associated with a significantly increased risk of maternal mortality, with an OR of 3.5 (95% CI: 1.4 to 8.6, p = 0.005). On the other hand, cesarean section is associated with a lower risk of mortality compared to vaginal delivery (OR: 0.1, 95% CI: 0.07 to 0.39, p < 0.001), suggesting a protective effect. Other pregnancy complications, such as anemia and preeclampsia, did not show significant associations with maternal mortality in the bivariate analysis.
Table 5 reveals that delay in reaching the referral hospital (>2 hours) was strongly associated with an increased risk of maternal mortality (OR: 13.0, 95% CI: 4.8 to 36.5, p < 0.001). Likewise, lack of medication access also showed a significant association (OR: 5.1, 95% CI: 2.4 to 10.8, p < 0.001).
Tables 6 and 7 present the association between knowledge of warning signs and maternal mortality in referral hospitals in the Ica region between 2010 and 2020. The results reveal interesting patterns for both pregnant women and their companions.
Table 6 shows that recognition of vaginal bleeding as an alarm sign by the pregnant woman was associated with an increased risk of maternal mortality (OR: 2.9, 95% CI: 1.3 to 5.9, p = 0.005). Additionally, recognition of headache as a warning sign was associated with a lower risk of maternal mortality (OR: 0.4, 95% CI: 0.2 to 0.9, p = 0.03). Notably, recognition of decreased fetal movements showed a strong association with a lower risk of maternal mortality (OR: 0.1, 95% CI: 0.0 to 0.4, p < 0.001).
Table 7 which focuses on companion knowledge, shows that failure to recognize bleeding as a warning sign was significantly associated with an increased risk of maternal mortality (OR: 2.9, 95% CI: 1.5 to 6.1, p = 0.002). Likewise, the attendant’s non-recognition of fever as a warning sign was associated with a significantly increased risk (OR: 5.4, 95% CI: 2.1 to 13.8, p < 0.001). Similar to what was observed in pregnant women, non-recognition of decreased fetal movements by the companion was also associated with a significantly increased risk of maternal mortality (OR: 12.9, 95% CI: 4.2 to 39.5, p < 0.001).
Table 8 provides a detailed analysis of the factors associated with maternal mortality in the referral hospitals of the Ica region during the period 2010-2020. A multivariate logistic regression model was used to identify both significant risk factors and variables that did not reach statistical significance. The inclusion of the latter variables allows a more complete understanding of the underlying dynamics and their possible impact on the results.
The multivariate analysis was adjusted for possible confounding factors, such as age, educational level, and access to prenatal care. The selection of variables for adjustment was based on their theoretical relevance and the bivariate analysis results, using a threshold of p < 0.20 for initial inclusion. Variables that showed a p-value < 0.05 were retained in the final model.
Discussion
The discussion on maternal mortality is a critical topic in the field of public health, highlighting the importance of identifying and effectively addressing its risk factors. According to the World Health Organization (WHO), most maternal deaths are preventable [17]. Knowledge about the prevention and management of risk factors associated with maternal mortality is essential to prevent and treat obstetric complications. This knowledge provides health solutions that address human rights, gender, and social equality [[18,19]].
This study highlights key factors associated with maternal mortality in Ica, Peru, emphasizing the influence of the absence of a partner, history of anemia, delays in accessing medical care, and lack of knowledge of warning signs on mortality risk, as detailed in Table 8. These findings reinforce the need for interventions aimed at improving the availability and quality of maternal care services, as well as educational programs for women of childbearing age and their communities. The correlation between these factors and maternal mortality highlights the importance of comprehensive approaches that include social support, adequate nutrition, accessible health infrastructure, and health education. This analysis contributes to the understanding of the complexities behind maternal mortality in the region, providing a starting point for policies and strategies focused on reducing these preventable deaths.
The study revealed that pregnant women without a partner are 4.8 times more likely to experience maternal death compared to those with a partner. This finding is consistent with the literature suggesting that lack of partner support may exacerbate risks during pregnancy and childbirth. However, it is important to consider that this association may be influenced by various underlying factors not fully captured in the statistical analysis. In a review study conducted in 37 low- and middle-income countries in Africa, autonomy in health decision-making in 38% of women without a partner was found to rank with a 1.19-fold increased odds of dying (AOR = 1.19; 95% CI: 1.15 to 1.24) [20,21]. The absence of support from a partner may restrict rapid and effective decision-making about their health, especially in emergencies.
A study in Tunisia revealed that women without a partner are vulnerable due to discrimination, social stigmatization, and abusive treatment during childbirth in health institutions [21]. This real or perceived poor quality of care is directly and indirectly associated with adverse maternal and neonatal outcomes [22].
To address these challenges, it is essential to implement strategies that mitigate the risks associated with the lack of a partner during pregnancy, such as education and awareness programs targeting both pregnant women and their communities to improve recognition of warning signs and the importance of seeking timely medical care. It is also important to strengthen community support networks that can provide emotional and practical assistance to pregnant women without partners. In addition, it is necessary to implement policies that ensure respectful and non-discriminatory treatment in health institutions and to ensure that all women, regardless of their marital status, have access to quality health services, including prenatal and emergency care.
The present study highlights the significant association between a history of moderate to severe anemia and an increased odds of maternal mortality, showing a threefold increased odds compared to those without a history of anemia. Similar studies in China [23] and in a multilevel analysis study in 29 countries in Latin America, Africa, the Western Pacific, the Eastern Mediterranean, and Southeast Asia [24] also found an association between severe anemia and maternal mortality, where the odds of maternal death were twice as high in those with severe anemia compared to those without severe anemia. The existing literature often does not differentiate between pre-existing anemia and gestational anemia, which underscores the importance of this study in filling that gap.
Anemia is a worldwide priority public health and nutrition problem [25]. It affects 33% of the world’s population and 38% of pregnant women, reportedly [26]. Anemia reduces hemoglobin concentration, which limits the body’s ability to carry oxygen, compromising the mother’s physiological reserve and increasing her susceptibility to obstetric complications.
The scarce literature on pregestational anemia underscores the seriousness of its consequences. Timely diagnosis and effective preventive management are crucial to address pre-existing anemia. This emphasizes the importance of implementing comprehensive public health policies that treat anemia during pregnancy and prioritize its prevention and management before conception.
Maternal mortality is closely related to anemia, which in turn is influenced by nutritional, socioeconomic, and health factors. Previous studies have found a strong association between severe anemia during pregnancy and an increased risk of maternal mortality [27,28,29,30,31].
Intervention and prevention are critical. Iron and folic acid supplementation programs and improvements in prenatal care have significantly reduced anemia and its maternal complications [25,27,27,28,30]. This emphasizes the need for public health policies focused on treating anemia and addressing its underlying determinants.
Delays in arrival at healthcare facilities significantly predict maternal mortality in our study and in research conducted globally [31,32,33,34]. Multicenter studies in low- and middle-income countries have identified that prolonged time from the onset of an obstetric complication to receipt of appropriate treatment is associated with worse maternal outcomes [32].
The distance and travel time to referral hospitals are considerable in our study region. Referral hospitals in the Ica region are centralized in the city of Ica, meaning patients must travel from the north of the region to reach a referral hospital within 90 to 120 minutes. In addition, to get from the southern end of the region to the city of Ica, the trip takes 3 hours or more. This may affect current pregnancy management, as women may experience delays in prenatal care and the detection of obstetric complications [35].
These extended travel times between home and health facilities increase the likelihood that the woman’s health status will be poor on admission to the referral hospital. Lack of transportation and distance are significant barriers to effective management of the current pregnancy, which may contribute to maternal mortality [34,36].
Other studies have highlighted how cultural perceptions and socioeconomic barriers complement geographic challenges, delaying care-seeking. This finding suggests that interventions should be holistic, addressing physical as well as socioeconomic and cultural barriers.
Delay due to failure to transfer the complicated patient is associated with populations facing unequal or inadequate surgical care delivery, chronically underserved populations, or those in acute crises, contributing significantly to maternal mortality [36].
The identification of vaginal bleeding as a dangerous sign by the pregnant woman and its association with a significant increase in the likelihood of maternal death, as observed in this study and others conducted in Mali [37] and northern Nigeria [38], suggests that the magnitude of bleeding was considerable to be recognized as an adverse event. This recognition by the patient or her relatives is crucial, as vaginal bleeding may be an indicator of serious obstetric conditions that require immediate medical attention.
However, the fact that recognition of bleeding increases the likelihood of maternal death indicates that there may be other contributing factors that influence this outcome beyond the severity of the bleeding. One such factor may be a delay in seeking medical care. Barriers to accessing adequate and timely health services may include lack of knowledge about the severity of symptoms, distance to health facilities, lack of transportation, and socioeconomic and cultural factors that limit women’s ability to seek help [37,38].
In addition, once the patient arrives at the health center, there may be additional delays in receiving appropriate care due to limited availability of trained staff, insufficient equipment, or overburdened health systems [37]. The medical literature suggests that prenatal education that includes information about warning signs during pregnancy and the importance of seeking immediate medical care may improve maternal outcomes [38].
Therefore, while recognition of vaginal bleeding as an alarm sign is essential, it is also critical to address systemic and educational barriers that may delay seeking medical care and ultimately affect maternal outcomes.
Maternal mortality remains a serious global public health problem, highlighting the need to identify and address its risk factors effectively. Among these, timely recognition of warning signs is critical. This study reveals that hemorrhage not recognized as a warning sign by the attendant significantly increases the risk of maternal mortality, increasing the risk of fatal outcomes by 7.4 times. This finding underscores the critical need for education and awareness among healthcare professionals and those accompanying pregnant women.
Previous literature has emphasized the importance of knowledge and early recognition of warning signs during pregnancy and postpartum to reduce maternal mortality [37,38]. In particular, low husband involvement and lack of recognition of critical signs such as hemorrhage highlight a significant gap in education and communication that needs to be addressed [37,38]. This is crucial, as a delay in recognizing the seriousness of the situation may contribute to the identified "three delays" in maternal health care: delay in deciding to seek care, delay in getting to a health facility, and delay in receiving appropriate care once there [34,38].
In addition, research suggests that companion and community training could be crucial for cases of postpartum hemorrhage [38]. This highlights the need for public health policies and education programs focusing on the general population. Community education should include information on warning signs and the importance of seeking immediate medical attention, thus improving the responsiveness to obstetric emergencies.
Moving toward reducing maternal mortality requires a collective commitment to generate significant changes in health systems and community education, ensuring that all women have access to quality and timely care.
Limitations
This study has several limitations that should be considered when interpreting the results. The study sample was based on maternal mortality cases registered in a given period, which could generate a selection bias and limit the generalizability of the results to other populations or contexts. Data collection was based on interviews with family members and others, which could generate limitations regarding the quality and accuracy of the information collected. Although an attempt was made to control for some confounding variables, it may be possible that not all relevant variables affecting the relationship between the variables studied and maternal mortality were considered. In addition, the measurement of some variables, such as the cohabitation relationship, could be subjective and susceptible to measurement errors. Finally, the study did not establish causality between the variables studied and maternal mortality, which limits the interpretation of the results. These limitations suggest that the results should be interpreted cautiously and that future research should attempt to address these limitations to gain a complete understanding of maternal mortality.
Conclusions
This study highlights critical factors contributing to maternal mortality in Ica, Peru, such as the absence of a partner, a history of anemia, delays in access to medical care, and lack of knowledge of warning signs. These findings underscore the need for comprehensive strategies to improve access to health services and health education. Implementing targeted interventions and strengthening support networks can play a key role in reducing maternal mortality.
Close collaboration between the Peruvian Ministry of Health and regional governments is essential to reduce preventable maternal mortality. This collaboration should focus on increasing the coverage and quality of prenatal care, improving maternal health awareness, providing accessible 24-hour transportation for patients with obstetric complications, and ensuring that provincial hospitals are prepared to diagnose and manage pregnancy-related complications rapidly.
In addition, more research is needed to identify other underlying factors that could contribute to preventing maternal mortality. This will enable the development of more effective and targeted strategies. A multifaceted approach, including education, infrastructure, and training of health personnel, is essential to create a safe maternal environment and move toward the goal of eliminating preventable maternal mortality in the region and beyond.

