Estudios originales
← vista completaPublicado el 17 de marzo de 2025 | http://doi.org/10.5867/medwave.2025.02.2962
COVID-19 como factor de riesgo para el desarrollo de fibrosis pulmonar en un hospital de referencia de Lima, Perú
COVID-19 as a risk factor for the development of pulmonary fibrosis in a referral hospital in Lima, Peru
Abstract
Introduction The emergency caused by the COVID-19 pandemic has passed, but we must study the potential sequelae left in the population. Cases of pulmonary fibrosis have been reported after severe COVID-19. However, the association between these factors has not been widely studied in Latin American countries, one of the regions most affected by the pandemic.
Methods A case-control study was conducted to determine whether a history of hospitalization due to COVID-19 is a risk factor for developing pulmonary fibrosis. We compared patients with a radiological diagnosis of pulmonary fibrosis on high-resolution computed tomography (cases) with those without such findings (controls), conducted between March 2021 and June 2023 in a referral hospital in Lima, Peru.
Results Among the total number of patients evaluated, the median age was 72 years, with a predominance of females (58.2%). 7.5% of patients with pulmonary fibrosis had a history of hospitalization due to COVID-19, compared to 6.1% in the control group (OR 1.24; 95% CI 0.65 to 2.36). The stratified analysis revealed a significant odds ratio for the group of patients with arterial hypertension (OR 5.9; 95% CI 1.28 to 27.34). The median follow-up after hospitalization for COVID-19 was 315.5 days.
Conclusions Hospitalization due to COVID-19 was not a risk factor for developing pulmonary fibrosis one year after medical discharge, except in patients with hypertension. Evidence suggests that the prevalence of pulmonary fibrosis may decrease over time.
Main messages
- We address the history of severe COVID-19 as a risk factor for developing pulmonary fibrosis, a relationship that has been little studied in the region.
- Limitations include the sample size and the restriction to a single hospital, which may affect the generalization of the results.
- This study is a pioneer in addressing the issue of pulmonary fibrosis after COVID-19 in the Peruvian population, allowing an approximation of the pandemic’s impact beyond the acute onset of the disease.
Introduction
In December 2019, an outbreak of an acute respiratory disease began in China that would transform the history of humanity. This disease would become known as coronavirus disease 2019 (COVID-19). Since then, the number of cases worldwide has risen to more than 600 million, with more than six million deaths [1].
Diffuse parenchymal lung diseases comprise a diverse group of disorders. These include idiopathic pulmonary fibrosis and secondary pulmonary fibrosis related to occupational or environmental exposure to drugs, among others [2]. In a study conducted in the United States using data from the Veterans Health Administration’s electronic medical records system, the prevalence of idiopathic pulmonary fibrosis in 2019 was estimated to be 725 cases per 100 000 patients [3] Pulmonary fibrosis begins with acute injury to the lung parenchyma leading to chronic interstitial inflammation, then to fibroblast activation and proliferation. Finally, it progresses to the common end point of pulmonary fibrosis and tissue destruction [4]. The incorporation into the virus cell that causes COVID-19 results in a loss of the enzyme that converts angiotensin II on the cell surface. Therefore, it prevents the degradation of angiotensin II into angiotensin 1-7, which has vasodilatory/antiproliferative actions. This contributes to the lung damage and fibrosis associated with this disease [5].
An open lung biopsy or thoracoscopy is required to establish a definitive diagnosis of pulmonary fibrosis. However, lung biopsy’s role in the high-resolution computed tomography era remains controversial. This is because some suggest forgoing biopsy when the clinical and tomographic characteristics typical of interstitial lung disease are present [2]. These radiological characteristics, such as the usual interstitial pneumonia pattern, described by members of the Fleischner Society, whose histological findings coincide with those of pulmonary fibrosis [6]. In addition, these members support the idea that computed tomography would allow for diagnosing idiopathic pulmonary fibrosis without needing biopsy, when the usual interstitial pneumonia pattern is present [7].
The Spanish Society of General and Family Physicians defines the sequelae of COVID-19, frequently referred to as 'post-COVID', as when there is a history of severe disease, requiring hospitalization, followed by persistent symptoms due to structural damage from the complications suffered (sequelae). This spectrum of sequelae includes the development of fibrotic changes in the lung [8].
Pulmonary fibrosis is uncommon after viral pneumonias and has rarely been reported after H1N1 pneumonia. However, fibrotic changes have been reported in patients with acute respiratory distress syndrome and H7N9 influenza [9]. There have been reports of pulmonary fibrosis following severe cases of COVID-19 with no previous history [10]. However, the exact proportion of patients with COVID-19 who develop pulmonary fibrosis remains speculative, due to the scarcity of data on the course of this pathology in the post-pandemic context [11]. While some studies suggest that damage to lung tissue from COVID-19 could be quickly reversed [12], others indicate that such changes could persist for up to a year after medical discharge [13,14,15].
The follow-up of cohorts of COVID-19 survivors is being carried out in several centers to determine if the pulmonary fibrotic changes persist, gradually improve, or even worsen over time [16]. Currently in Peru, one of the countries most affected by the COVID-19 pandemic, there have been more than 4.4 million cases with more than 210 000 deaths [17]. It is estimated that 5% of all these cases have been admitted to intensive care units [18]. Although the number of cases has decreased, especially the most severe ones, it is necessary to address the sequelae that the public health system will have to deal with in the post-pandemic stage. Different institutions are already raising serious concerns about the high number of patients with pulmonary fibrosis, especially among those patients who had severe symptoms [19].
However, there are no published studies related to post-COVID-19 pulmonary fibrosis in Peru. Therefore, this study aimed to determine if a history of hospitalization (severe cases) for COVID-19 is a risk factor for developing pulmonary fibrosis in patients at a referral hospital in Lima, Peru.
Methods
A case-control study was conducted with patients whose high-resolution chest computed tomography scans were performed between March 2021 (one year after the pandemic onset) and June 2023 at a referral hospital in Lima, Peru. The establishment is part of the Social Health Insurance (EsSalud) network. The information was analyzed in August 2023.
The cases were the patients whose high-resolution chest computed tomography reports revealed a radiological pattern of usual interstitial pneumonia according to the Fleischner Society criteria [7], equivalent to a diagnosis of pulmonary fibrosis [6]. In the absence of lung biopsy results, these criteria were used and we will refer to the “cases” as those patients with a “radiological diagnosis of pulmonary fibrosis”. Previous studies have used this approach to describe the association between COVID-19 and pulmonary fibrosis [14,20]. The sample size was calculated following the recommendations for sample calculation in case-control studies by Pita-Fernández. Therefore, a 95% confidence level, 85% statistical power and an approximate prevalence of the exposure factor in the control group (moderate to severe COVID-19 in the population of Lima, Peru) of 8% were considered, with an expected odds ratio of 2.0 [21].
The controls were patients without radiological evidence of characteristic patterns on high-resolution computed tomography. They were randomly selected from the list of patients from the same period and the same healthcare center from which the cases were obtained. For the selection, a 1-to-1 pairing with the cases was carried out directly with the statistical software SPSS.
The exposure factor evaluated was a history of hospitalization for COVID-19, confirmed by molecular tests.
We included patients over 18 with a high-resolution computed tomography (HRCT) chest scan, duly reported by a radiologist. Patients without a digital medical record, with a high-resolution computed tomography scan of the chest performed during the acute phase of COVID-19 and those diagnosed with pulmonary fibrosis before hospital admission for COVID-19 were excluded. Approval was obtained from the ethics committee corresponding to the center where the patient data were accessed.
The patients were described according to age, gender, comorbidities, days and place of hospitalization, admission to the intensive care unit, radiological findings, and diagnoses in the control group, among other factors. The descriptions were made according to the presence or absence of a radiological diagnosis of pulmonary fibrosis (cases versus controls) and secondarily according to a history of hospitalization for COVID-19.
The Kolmogorov-Smirnov test was used to determine normality. The quantitative variables were expressed as median and interquartile range and analyzed using the Mann-Whitney U test. The qualitative variables were expressed as proportions and analyzed using the Chi-square and Fisher’s exact tests. The odds ratio with a 95% confidence interval was used to measure association.
A stratified analysis was carried out by age, gender and comorbidities, to identify possible confounding factors in the odds ratio of the association between a history of hospitalization for COVID-19 and the radiological diagnosis of pulmonary fibrosis. A statistically significant value was considered to be p < 0.05. Statistical analysis was performed using SPSS V27 statistical software and the Open Epi web tool.
The present study was developed following the standards and indications of the guidelines, The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [22].
This study reportedly involved human subjects and ensured compliance with international ethical standards. Approval was obtained from the corresponding Institutional Ethics Committee, identified as AUT. N° 046 -CE-GHNERM-GRPR-ESSALUD-2024. This committee evaluated and approved the research protocol, guaranteeing respect for the rights and safety of the participants. Proof of this approval will be provided if requested by the editorial committee.
Results
During the period studied, 46 474 records of high-resolution computed tomography studies were filtered according to the diagnosis of interstitial lung disease (code J84.9, of the International Classification of Diseases, 10th edition, ICD10), finding 393 records. After applying exclusion criteria, 293 patients were finally included (Figure 1). The same number of controls were randomly selected and matched for age and gender, from the population of patients with high-resolution computed tomography studies from the same health center and during the same period.
Flow chart of patient selection for the study.
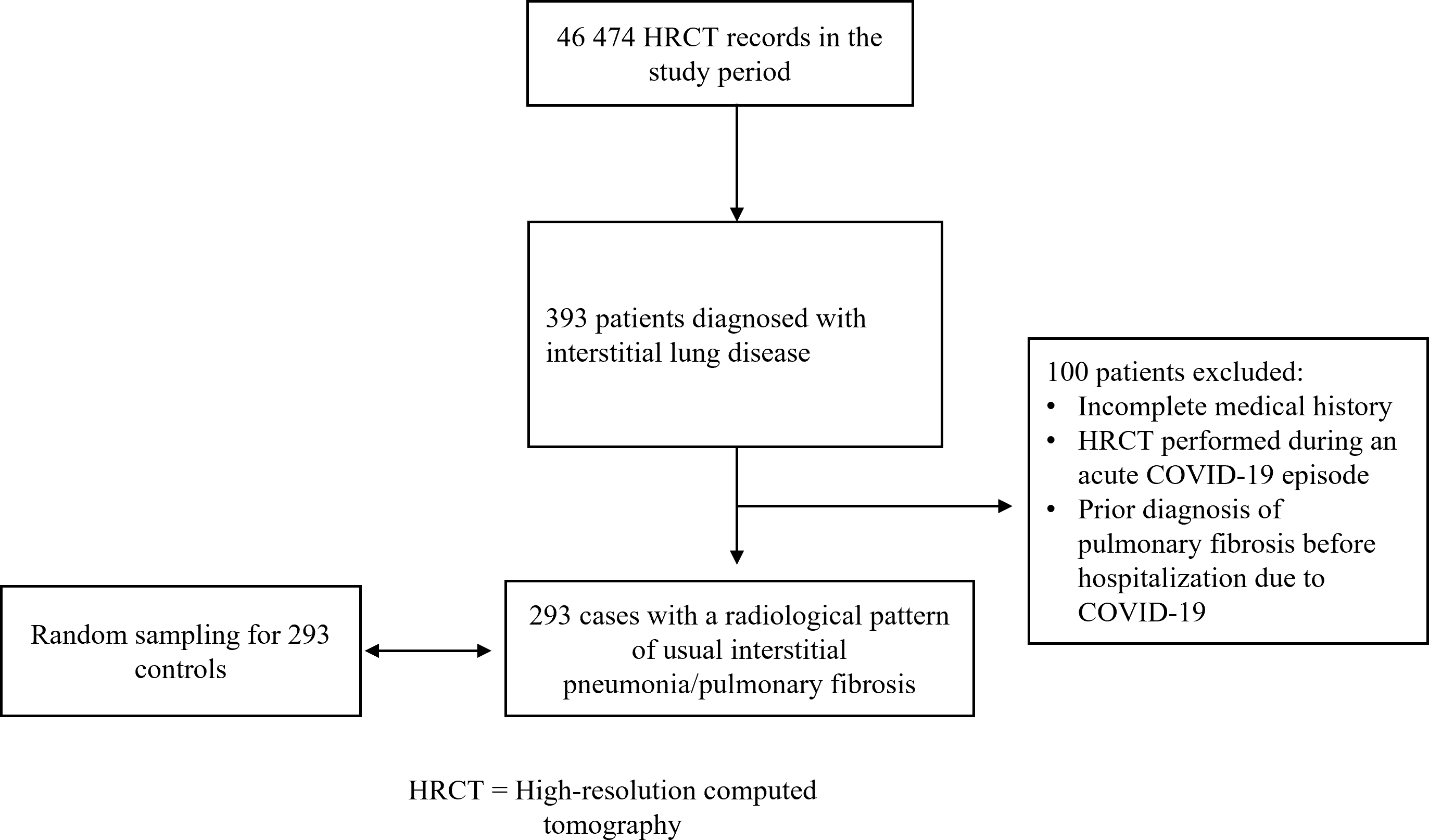
Source: Prepared by the authors based on the results of the study.
The odds of suffering from pulmonary fibrosis were 24% higher in patients hospitalized with COVID-19 compared to patients in the control group. However, this result was not statistically significant (OR 1.24; 95% CI 0.65 to 2.36) (tables 1 and 2).
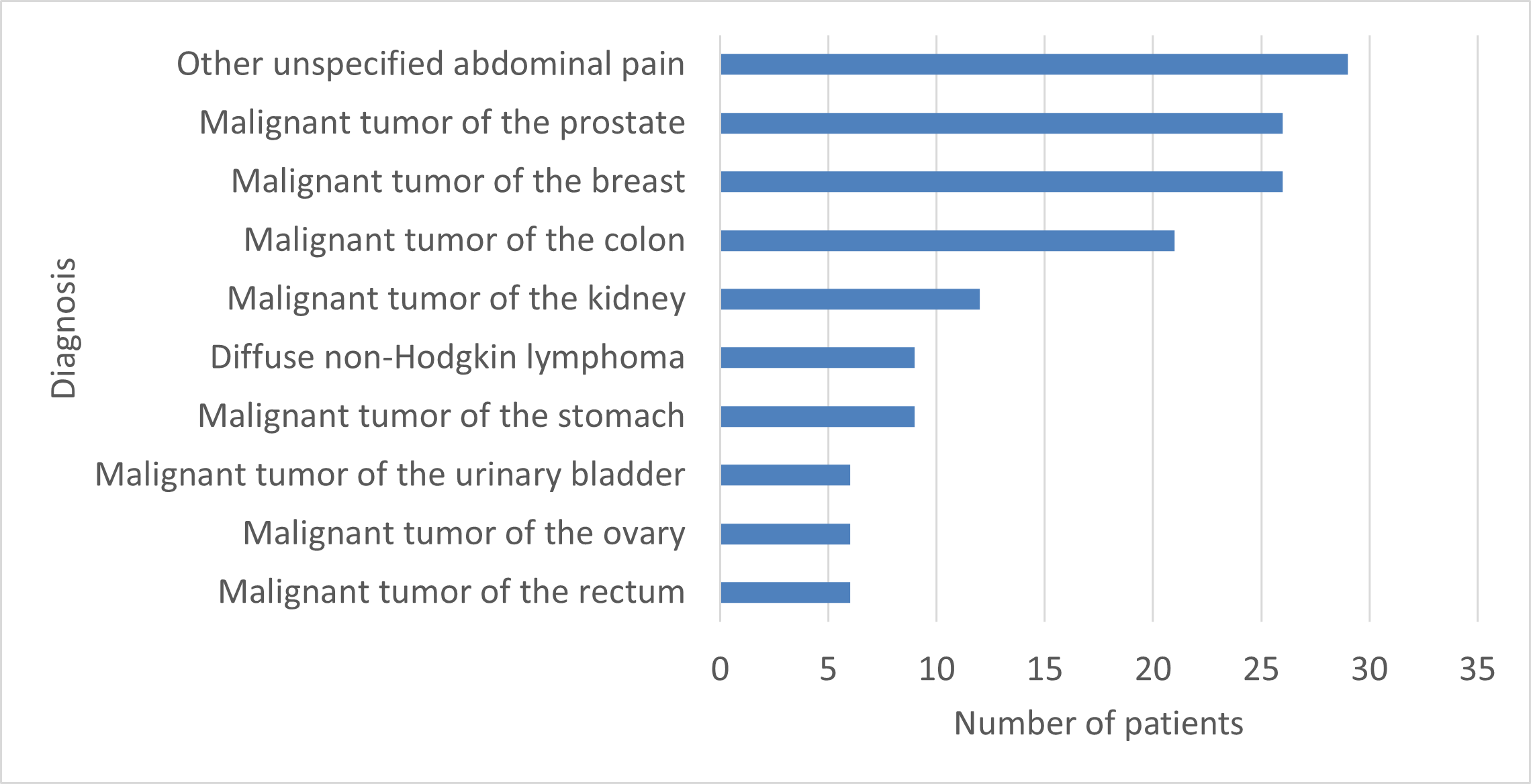
Table 2 presents the clinical-epidemiological characteristics of the total number of patients and compares cases and controls. The control group reported a higher frequency in the diagnosis of cancer of any location (< 0.001), since in many of these patients the indication for high-resolution computed tomography is in the context of the study of neoplastic diseases. The 10 most common diagnoses in the control group are shown in Figure 2.
Most common diagnoses in the control group
Source: Prepared by the authors.
 Full size
Full size A stratified analysis was carried out by age, gender and comorbidities to evaluate possible confounding or effect-modifying factors in the association between history of hospitalization for COVID-19 and radiological diagnosis of pulmonary fibrosis. In patients with a history of arterial hypertension (effect modifier), an OR of 5.9 (95% CI 1.28 to 27.34) was found, while in patients without arterial hypertension the OR was 0.17 (95% CI of 0.04 to 0.78). Therefore, although in general a history of hospitalization for COVID-19 was not observed to be a risk factor for developing pulmonary fibrosis, in the specific case of patients with arterial hypertension, the odds of pulmonary fibrosis were 490% higher in those with a history of hospitalization for COVID-19 compared to patients in the control group. Gender, age group over or under 65, history of diabetes mellitus, cancer of any site, hypothyroidism and chronic kidney disease were identified as effect modifiers. However, we found no statistically significant odds ratio in the cases.
Among patients with pulmonary fibrosis who had previously been hospitalized for COVID-19 (n = 22), the time between hospitalization and the high-resolution computed tomography scan that showed pulmonary fibrosis was 315.5 days as a median, with an interquartile range of 259.5 to 574 days. Details on the frequencies of the different radiological patterns in this group of patients are described in Table 3.
Discussion
This study evaluated the history of hospitalization for COVID-19 and the development of pulmonary fibrosis by comparing a group of patients with a radiological diagnosis of pulmonary fibrosis by high-resolution computed tomography and a control group. The analysis considered histories of hospitalization for COVID-19, finding no significant association between the two variables.
Pulmonary fibrosis and COVID-19
Najjar-Debbiny et al., in their 2023 nested case-control study, compared the findings of 1284 patients with pulmonary fibrosis from the original cohort with 12 840 matched controls. The analysis revealed that the odds ratio for pulmonary fibrosis was 1.80 (95% CI 1.47 to 2.19) in patients with COVID-19 compared to those without COVID-19 60 days after discharge from the physician [20]. Our analysis showed a similar odds ratio, although it did not reach statistical significance (OR 1.24; 95% CI 0.65 to 2.36). This disparity could be attributed to several factors, such as the difference in sample size. Najjar-Debbiny et al. handled a sample 4.3 times larger in terms of “cases”, increasing their statistical power. In addition, the analysis was performed closer to discharge for COVID-19 compared to our study (60 days versus 315.5 days) [20].
rted results up to 180 days, with an odds ratio of 1.35 (1.03 to 1.78), suggesting a possible reduction in risk with an extended follow-up period [20]. This hypothesis could be supported by the findings of Vijayakumar et al. in 2022, who, in their prospective cohort study with COVID-19 survivors evaluated by chest computed tomography, found unequivocal signs indicative of established fibrosis in 12% of their patients three months after medical discharge. In addition, they reported a statistically significant improvement in the overall extent of the recorded abnormalities and the extent of ground glass opacification and fibrous bands at the one-year follow-up, with no progression of the findings in any of the study participants [14]. Although our results did not consider the extent of the lesions, we also observed a trend towards reducing the number of lesions from the first year onwards. Similar findings have been reported in other studies, such as Wu et al. in 2021, who followed up 83 non-ventilated COVID-19 patients one year after medical discharge, finding progressive improvement in radiological abnormalities in most cases [23]. The evidence seems to indicate that the prevalence of lesions suggestive of pulmonary fibrosis varies according to the length of follow-up.
It has been reported that patients with specific comorbidities have a higher risk of complications from COVID-19 [24]. In our study, the stratified analysis showed that patients with arterial hypertension had a higher risk of developing pulmonary fibrosis after COVID-19 hospitalization. This finding is consistent with that reported by Zhao et al. in 2020, in patients from China. They observed a higher frequency of these comorbidities in patients with abnormal high-resolution computed tomography at three months after discharge for COVID-19 [13]. Likewise, Abdel-Hamid et al. in 2021 reported that older, male patients with a high body mass index more frequently developed residual lung lesions after COVID-19, including pulmonary fibrosis [25]. Interestingly, in our study, patients who were hospitalized for COVID-19 and required admission to the intensive care unit did not show a higher frequency of radiological changes indicative of pulmonary fibrosis. This differs from previous reports where a prolonged stay in the intensive care unit and the duration of mechanical ventilation represented risk factors for the development of pulmonary fibrosis [11]. This discrepancy could be attributed to the low number of patients analyzed with a history of hospitalization for COVID-19 in our sample, which may limit the finding of significant differences.
Strengths and limitations of the study
Although this study attempted to provide uniformity and clarity regarding the radiological pattern of pulmonary fibrosis, according to international criteria [6,7], the use of non-specific radiological terms and different radiological signs (such as parenchymal bands, traction bronchiectasis, and panelization) under the generic label of “fibrotic lesions” warrants scrutiny and more detailed and precise studies. Finally, the variability between observers when interpreting non-specific signs added a challenge when interpreting the results of high-resolution computed tomography.
On the other hand, the small number of patients with a history of COVID-19 in both groups (cases versus controls) limited the possibility of reaching more solid conclusions on the subject. However, it is worth noting that this study is a pioneer in addressing the issue of pulmonary fibrosis after COVID-19 in the Peruvian population, allowing an approximation to the impact of the pandemic beyond the acute onset of the disease.
Given the large proportion of the population affected during the pandemic and its particular impact in Peru [17], prospective studies with long-term follow-ups (beyond one year) are advisable, not only through imaging but also by lung biopsies as far as possible. This would make it possible to assess the actual prevalence of fibrotic lesions over time in survivors of severe cases of COVID-19.
Conclusions
The history of hospitalization for COVID-19 did not prove to be a risk factor for developing pulmonary fibrosis when considering the presence of high-resolution computed tomography patterns after an approximately one-year follow-up. However, the association was significant in the patients with arterial hypertension.
The evidence suggests that the prevalence of pulmonary fibrosis could decrease over time. The patients studied with pulmonary fibrosis presented similarities in age, gender, and comorbidities with previous studies carried out in the country and Latin America. However, the frequency of radiological lesions was higher compared to international registries.
Given the impact of the pandemic in Peru, prospective studies with long-term follow-ups are advisable. This will allow us to evaluate the true prevalence of fibrotic lesions over time in survivors of severe cases of COVID-19.

