Estudios originales
← vista completaPublicado el 7 de marzo de 2025 | http://doi.org/10.5867/medwave.2025.02.2986
Patrón psicosocial de la violencia interprofesional en el trabajo sanitario peruano: estudio de consenso Delphi mixto
Psychosocial pattern of interprofessional violence in Peruvian healthcare work: A mixed Delphi consensus study
Abstract
Introduction Studies on psychological violence in health care facilities have focused on the analysis of incidences in specific contexts. Nevertheless, consensus studies on the psychosocial factors of interprofessional violence related to interpersonal conflict and motivational demands are scarce. The aim of this study is to determine by Delphi consensus the psychosocial pattern of interprofessional violence in healthcare work for Peru and its geographical regions.
Methods A mixed Delphi consensus method was applied, bringing together professionals with experience and knowledge of psychological violence. The study was conducted in three stages and three rounds of Delphi consultation between May 2023 and June 2024. The integration of consensus at regional and national levels was carried out through Graph Network Analysis.
Results Up to the third stage of the study, 444 experts in 32 focus groups from 81 health care institutions participated. 70.5% of the participants were women and 27.6% worked in nursing and emergency departments. After the Delphi consensus analysis, we obtained a ranked list of six psychosocial factors of interprofessional violence for Peru and nine for the regions.
Conclusions According to the consensus, two of the main psychosocial factors of interprofessional violence in health establishments in the Costa and Forest regions are the devaluation of work and harassment by superiors towards subordinates that induce them to change jobs or resign. Excessive control by colleagues was the first hierarchy for the Sierra region. The differences between geographical regions in Peru and between studies in other countries reflect that the phenomenon of interprofessional violence is very specific and contextual; in the case of Peru the differences between regions may be due to health care facilities with different characteristics (e.g., rural vs. urban facilities).
Main messages
- This is the first study in the country that assess the risk factors of interprofessional psychological violence through expert consensus to guide a contextualized prevention.
- The results of the Delphi consensus analysis present a hierarchical list of 6 psychosocial factors of interprofessional violence for Peru and 9 for the regions.
- Limitations of this study are the possible confusion of the most important factor with; and the threatening of the external validity due to participants belonging to the same level of care, distributed in three geographical regions of the country including rural centers, with interventions addressed from the level of the analysis group, and the loss of 17% of participants due to attrition of interest.
Introduction
Psychosocial risk factors are determinants of health in the work context, as they can affect the worker’s physical, psychological, and social well-being [1,2,3,4]. Therefore, the intervention of these risks and their consequences promotes a culture of psychosocial safety at work [5,6,7,8].
Psychological violence is understood as intentional behavior in which workers are verbally assaulted, threatened, and/or humiliated during their working day [9,10,11]. This violence is often related to interpersonal conflicts and motivational demands [3,12,13].
In the healthcare sector, the agent exercising interprofessional psychological violence [14] ─ the subject of the present study ─ is a superior or a subordinate. Such subjects do so because of a lack of expectations, struggles of interests, communication problems, or perceptions of inequity and imbalance in the workplace [3,5,6,7]. Interprofessional psychological violence in the healthcare sector, in addition to burnout and emotional stress [15], leads to decreased quality of care and job satisfaction [5,6,16] and, consequently, organizational commitment [17]. These conditions constitute a stressful phenomenon in working life and an occupational public health problem [1,3,6,7].
Frame of reference
Karasek’s three-dimensional demand-control-support model of the psychosocial work environment [18,19] allows explaining psychological violence at work in healthcare professionals. In addition, it identifies areas for improvement in managing workloads and promoting a healthy work environment [18,19]. This model establishes the links between latent profiles and interpersonal stress in occupational health. It also postulates that well-being and occupational stress depend on the interaction between job demands and health professionals' control over their tasks [18,19]. In the healthcare context, demands are often high due to time pressure, high workload, and rigorous expectations of users. Meanwhile, low control manifests in limited autonomy for decision-making and highly standardized procedures that restrict personalized responsiveness. Thus, in an environment where demands exceed the available control, psychological violence may increase, deteriorating emotional stability [18,19].
Current studies on interprofessional psychosocial violence
Recent studies on the psychosocial characterization of violence between professionals and administrative staff in the health sector in developed countries such as Italy, the United States, Israel, the United Kingdom, India, Australia, China, and Spain are related to verbal aggression, generally due to role conflict followed by harassment and excessive control by superiors.
The violence between doctors and nurses by country and interprofessional group includes personal and professional discrediting, ignoring or isolating the colleague, punishing the professional for minimal errors, and assigning excessive tasks to be completed quickly [14,18,20,21,22,23,24,25]. In low- and middle-income countries such as Iran, Turkey, and Nepal, verbal aggression predominates, followed by humiliation and harassment of colleagues. This often results in resignation or displacement from the position [26,27]. Among nurses, the main characteristic is humiliation and sanctions for insignificant errors [28] (Annex 1a).
These psychosocial risks, as a cause of interprofessional violence, may be more frequent in situations where the professional team is not cohesive, lacks social support, and when staff turnover is high [14,23,29,30].
In the United States, a self-report survey with semi-structured interviews showed that 67.1% (51/76 nurses) in two American hospitals had experienced violence in the form of humiliation and contempt in the last month, and 23.7% (18/76) had experienced it in their entire career [24]. Psychological violence assessed by semi-structured interviews, biograms, and self-reports in health professionals in Chile was 39.1% [31,32].
In Peru, a country with a medium-sized economy made up of 24 departments and a constitutional province located in three geographical regions: coast, with an arid-temperate climate, highlands (rainy-cold), and rainforest (rainy-warm), and with three health systems: public, private and social security [33]; it is estimated that interprofessional psychological violence affects 36.2% (673 603/271 923 health workers) [33].
In the health sector of developed countries, some psychosocial interventions to reduce psychological violence within specific contexts have been studied in systematic reviews [14,21,29,31,34,35,36]. The only study using Delphi consensus characterization on psychosocial health and safety is by Mohd et al. [37]. Similarly, studies on the characterization of psychological violence in interprofessional care groups, including care and administrative staff, both in Latin America and Peru, are also limited [15,31,34].
Establishing a hierarchy according to the frequency of psychosocial risk factors in interprofessional psychological violence using an expert consensus is important to define the scope and extent of the problem since data on incidences and prevalences obtained through cross-sectional surveys are not sufficient to develop effective preventive interventions [21].
After analyzing these risk factors, it may be possible to implement appropriate psychosocial interventions in the country’s health institutions, promote interprofessional integration, and propose policies to prevent psychosocial health and safety at work [38].
Due to the need to reach a consensus on the factors involved in interprofessional psychological violence, several authors [39,40,41] point out the need to obtain expert opinion to identify the pattern of psychosocial risk factors involved, knowing that knowledge about these factors will guide how they can be prevented [23]. In addition, such studies will contribute to designing more effective interventions to reduce interprofessional psychological violence at work, according to the differences in the sociocultural contexts of the groups involved [42,43].
Therefore, the best possible characterization of the psychosocial pattern is essential to contribute to a coherent, effective, and contextualized response to interprofessional violence in the health sector. This contributes to the well-being of staff and the quality of the service provided.
This study aims to reach a consensus on the psychosocial pattern of interprofessional violence in healthcare work for each geographical region of Peru (Coast, Highlands, and Rainforest).
Methods
This is a qualitative study based on the mixed Delphi consensus method. This method was applied because of its advantages in terms of anonymity, controlled feedback, and facilitating bringing together participants from different geographical areas [39]. In our case, professionals with shared experience and knowledge of interprofessional psychological violence factors were brought together, which facilitated consensus in the health sector of the three Peruvian geographic regions.
The Delphi process developed in three stages (Figure 1) followed the ACCORD (Accurate Consensus Reporting Document) protocol of the Enhancing the QUAlity and Transparency Of Health Research Network (EQUATOR) [44]. The study was executed between May 2023 and June 2024.
ACCORD flow chart.
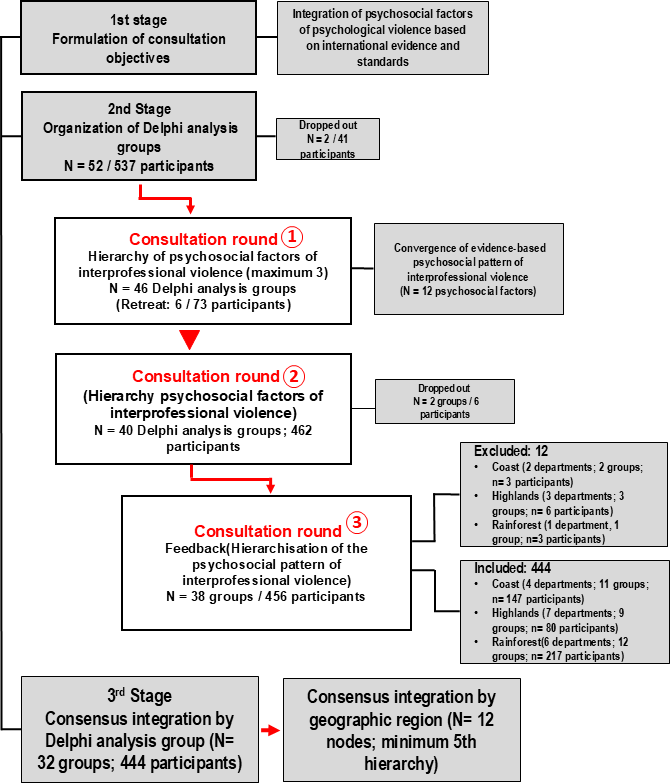
Source: Prepared by the authors of this study.
Data collection in the first stage was face-to-face, while in the second and third stages, it was online. In the second analysis stage, three rounds of Delphi consultation were developed. In the third stage, after organizing the hierarchies in a data matrix, the consensus was integrated at the Delphi analysis group level and then by geographic region (Figure 1).
Participants and procedures according to delphi consensus stages
First stage
Consultation objectives were formulated, the dimensions were explored, and the sources of information were defined. The profile and location of the participants were determined, and the group selection protocol was drawn up. Relevant aspects for selecting participants were that they had representative information, time, and interest and were close enough to contact potential members, choose them, invite them, and commit them to participate.
20/25 expert panelists contacted through WhatsApp Messenger (May 2023) accepted to participate, who were characterized by being:
-
Public health professionals with specialization in occupational health.
-
Members of occupational health and safety committees.
-
Professionals who had experienced or witnessed interprofessional violence.
-
Professionals with work experience of more than five years in the services with the highest psychosocial risk (emergency and admission of four public hospitals in Lima) [45].
These experts were provided with a comparative synoptic table of evidence based on several previously reviewed studies [10,13,17,46]. In addition, they were informed about the scope of the study, the ranking process, and the Delphi consensus. They were then asked to compile a list of psychosocial factors of interprofessional violence based on scientific evidence [10,13,17,46].
At the end of this stage (June 2023), a list of 12 psychosocial factors of interprofessional violence was drawn up (the first factor was coded F1 and the last factor F12), which served as a frame of reference for the following stages and rounds of Delphi consultation (Annex 1b).
Second stage
The judgmental sampling technique was used to select the participants.
Based on 22 901 health facilities of various types and at the national level, of which 49.9% corresponded to the coastal region, 37.6% to the highlands, and 12.5% to the rainforest region, 52 analysis groups were organized with an equal number of coordinators (July 2023 to April 2024). The coordinators invited experts by convenience through personal contact and WhatsApp Messenger, encouraging their participation. The criteria for inclusion of experts (from 2023 to April 2024) were:
-
Health professionals or administrative staff in the health sector of both genders.
-
Professionals who had experienced or witnessed interprofessional violence.
-
Professionals with more than three months of work experience.
-
Professionals from the three geographic regions of the country.
-
Professionals with voluntary participation up to the third round of the Delphi consultation.
The only criterion for including a health facility was that at least four participants were included [39,41]. The study included 177 health facilities (coast: 35.9%; 64/177), highlands (41%; 72/177), and rainforest (23.1%; 41/177). During this stage, four experts were kept as the minimum required per analysis group [39,41], and 46 groups participated (Figure 1).
The exclusion criteria for participants were:
-
Personnel with no experience or knowledge of interprofessional psychological violence.
-
Personnel in a probationary period (up to three months).
Twenty-one health facilities were excluded from the study.
In the first round of Delphi consultation of this stage (from September to November 2023), in each of the 46 analysis groups, the coordinators posed the following slogan to each expert:
"On a digital notepad, please write a list of three or more of the most frequent situations of psychological violence among health care professionals and health care workers. Situations that you have experienced or seen in your workplace during the last three months".
Then, each group coordinator analyzed the information received to integrate and regroup the psychosocial factors of interprofessional violence after merging duplicates and eliminating those factors with divergent opinions.
In the second round of consultation (December 2023 to January 2024), the coordinators produced an integrated list of 12 interprofessional violence factors in each of the 40 Delphi analysis groups (six groups desisted) and presented the experts with a two-column table (1: violence factors; 2: numbers) with the following instruction:
"In the table you see there are 12 factors of interprofessional psychological violence occurring in your workplace, and on the right side of each of them, there is a blank box. Please write in those boxes a number from 1 to 12 (no ties), number 1 = first most frequent factor and 12 = for the least frequent factor you have experienced or seen in your workplace during the past four months."
When a participant departed from the group’s opinion, the coordinators were invited to expand or reflect on their position.
In the third round of Delphi consultation (February to April 2024), each of the 38 analysis groups (two groups dropped out) presented the hierarchy matrices of the psychosocial factors for the knowledge and opinion of the experts. For the factors that were duplicated, triplicated, or even quadruplicated in the hierarchies, the experts were asked for a new hierarchy using the following slogan:
"The cause that most affects or the most important cause in interprofessional violence to intervene in the health center is ..."
The information received was then analyzed to present it in a round of feedback and carry out the final consultation round of consensus and disagreement.
Third stage (data analysis)
Based on the information from 32 Delphi analysis groups and 444 experts, the consensus on the psychosocial factors of interprofessional violence was determined at three levels: by analysis group, geographic region, and national level.
To establish the Delphi hierarchy at regional and national levels, the network analysis technique was applied using Gephi v.10.1.9 software [47]. Previously, a database was generated where the "nodes" were each of the 12 factors of interprofessional violence (F1 = first factor; F12 = last factor), and "edges" were each of the networks generated by the expert. Thus, each expert could choose from 1 to 12 factors (from the most frequent to the least frequent). The usefulness of Gephi was:
-
To determine the degree of predominance of a node concerning others (eigenvector centrality).
-
To assign several links per node, which made it possible to establish the hierarchy of each psychosocial factor.
-
Establish clusters of networks according to the degree of sophistication (modularity class).
-
Graphically visualize the interaction between the set of nodes and networks.
The criterion for considering consensus by psychosocial factor was to complete the ninth hierarchy (75%; 9/12). The remaining hierarchies were considered as discrepant factors [39,41].
The anonymized dataset, generated and analyzed during the present study, is deposited in the academic repository Figshare. DOI [https://doi.org/10.6084/m9.figshare.26110603.v1] (Annex 2).
Results
Description of participants
Participant’s characteristics are shown in Table 1. 70.5% (313/444) of the participants were female and worked in the nursing and emergency departments. 73.3% (137/313) had rotated out of their positions one to two times per year. The average age of the men was 39.9 years, and of the women, 38.1 years; 35.4% (157/444) of the experts were between 27 and 30 years old; and 3.4% (15/444) were 61 years old or older. Up to the final "integration" stage, 444 experts from 32 Delphi analysis groups from the three geographic regions of Peru participated. 48.9% (217/444) came from 12 focus groups from 6 departments in the Selva Region. In the coastal region, eight analysis groups (29.7% of participants; 132/444) were conducted in the Lima Department. Eighteen percent (80/444) of the experts were from 9 analysis groups from 7 departments in the Sierra Region (Table 2).
Consensus on the psychosocial pattern of interprofessional violence
At the national level
The six psychosocial factors of interprofessional violence, ranked according to the number of networks and the coefficient (EC: eigenvector centrality), are the factor devaluation of work experienced by the participant (F7: 190 networks; EC = 0.999), in the first place. Secondly, the work experience of the rest of the colleagues in the health facility is devalued (F8: 174 networks; EC = 998). Thirdly, harassment by the superior towards subordinates induces them to change positions or resign (F3: 150 networks; EC = 0.560). Fourth, excessive control by colleagues or superiors (F1: 156 networks; EC = 0.878). Fifthly, labeling as a negligent worker (e.g., blaming everything that goes wrong on a colleague; F9: 96 nets; EC = 0.461). In sixth place is role discrepancy between colleagues (F4: 90 networks; EC = 0.409).
Coastal region
There was consensus that the main psychosocial factor of interprofessional violence in the Coastal Region is the devaluation of work experienced by the participant and by the rest of the colleagues in the health facility (F7; F8), followed by the superior’s harassment of subordinates that induces them to change positions or resign (F3). According to the consultation, the psychosocial factors placed in the third and fourth hierarchy for interprofessional violence involve excessive control by superiors or colleagues (F1), with subsequent humiliation and verbal aggression (Table 3, Figure 2). Another violent factor considered important was the attitude of ignoring the worker in decision-making (F6). The eighth and ninth hierarchies refer to "labeling the worker as negligent" and work-professional hindrance (Table 3). The main factors in discrepancy were personal discrediting, intimidation, and role contradictions (Figure 2).
Network of psychosocial factors of interprofessional violence, Coastal region.
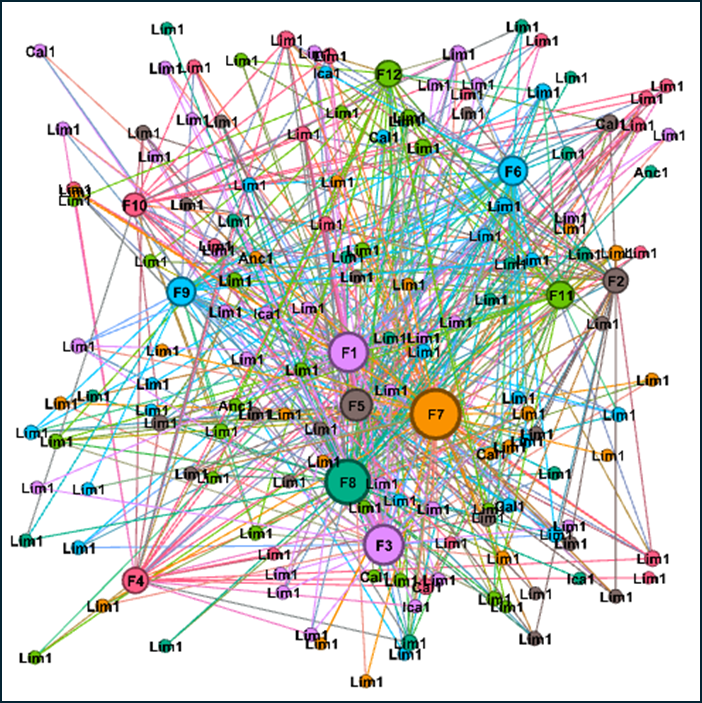
Source: Prepared by the authors of this study.
Highlands region
According to the experts consulted in the highlands region, the predominant psychosocial factors of consensus are excessive control exercised by superiors or colleagues (F1) and harassment by superiors towards subordinates that induce them to change positions or resign (F3) (Table 3). This is followed by role discrepancy (F4) and devaluation of staff work (F8). Factors in the fifth and sixth hierarchies involve rating the worker as negligent (F9) and consecutive bullying (F2). The psychosocial factors located in the seventh, eighth, and ninth hierarchies of interprofessional violence are devaluing the work of colleagues, hindering or limiting professional development opportunities, and humiliation with verbal aggression (Table 3).
On the other hand, the set of 1354 networks at the national level is classified into 17 clusters (evaluated using the modularity class coefficient), which measures the degree of sophistication of networks. Of the total number of clusters, nine are different, and eight have the same number of networks.
Rainforest region
There was consensus that "devaluation of work", experienced by both the consultation participant and the rest of the colleagues in the health facility, is the main psychosocial factor of interprofessional violence in the region. The following psychosocial factors are excessive control by colleagues or superiors and superior harassment of subordinates that induces them to change positions or resign (Table 3). Consensus psychosocial factors in the fifth and sixth hierarchies are labeling the worker as negligent and ignoring the worker in decision-making. Other factors are related to role contradictions, personal discrediting, humiliation, and verbal aggression toward the worker. The main factors in discrepancy were work-professional hindrance and intimidation.
Discussion
This study elaborated a hierarchical list of six psychosocial factors of interprofessional violence at the national level and nine factors for each geographic region. They show the consensus of experts on the most frequent pattern of interprofessional violence in the Peruvian health sector. From the national list, we found that "devaluation of the work of health professionals" is the most relevant factor in interprofessional violence, accounting for 26.8% (368/1371) of the total number of networks identified for each psychosocial factor. This is followed by "superior harassment of subordinates", "excessive control by colleagues or superiors", "labeling as a negligent worker", and "role discrepancy between colleagues".
Based on the experts' responses, we can infer at the national level that the precipitating factor for interprofessional violence [16,20] was role discrepancy and harassment for nurses, concurring in several studies [3,5,6,7,14,40].
This consensus of experts delimited by geographic region could respond to geographic (rural versus urban) and organizational causes. The analysis groups in rural areas (rainforest and highlands with contrasting climates) have greater limitations in human and financial resources compared to the coastal region.
In addition to contributing to the well-being of staff and the quality of service provided, consensus is important to ensure consistent and contextualized responses to interprofessional violence in the healthcare sector, as no single guideline is appropriate for all settings [30]. Furthermore, it provides evidence for proposing sustainable policies and intervention protocols to reduce interprofessional violence.
The consequences of interprofessional violence in the healthcare sector are wide-ranging. Among them are burnout and emotional stress [5,6,15,16,17]. This hostile environment can reduce the effectiveness of care, job satisfaction [5,6,16], and organizational commitment of staff [1,3,6,7,17,20].
This expert consensus finding that determines the national pattern of interprofessional violence up to the third hierarchy of factors converges with several studies from Italy, the United States, Israel, the United Kingdom, India, Australia, China, and Spain [14,18,20,21,22,23,24,25,29]. In these works, the most relevant factor in interprofessional violence is "devaluation of work with role discrepancy between colleagues", followed by "superior harassment of subordinates" and "excessive control by colleagues or superiors" (except between doctors and nurses). In the latter group, the common factor of interprofessional violence is "superior harassment of subordinates" and extends to middle and low-economic countries such as Iran, Turkey, and Nepal [26,27]. The last factor, "labeling as a negligent worker" (sixth hierarchy), is specific to Peru because the international antecedents did not include even this hierarchy.
The factors that differ in the hierarchies of other studies are "ignoring or isolating the colleague and punishing the professional for minimal errors", "assigning excessive tasks to be completed in a short time", and "verbal aggression with humiliation", which occurred only among physicians and nurses from different countries [14,18,20,21,22,23,24,25,26,27,29].
One of the reasons for the difference in hierarchies is that some studies involved, for example, only physicians and nurses [20], while others involved only nurses [20,28]. In contrast, healthcare and administrative staff were included in this study.
Particularly, in hospital centers in different developed countries [10,15,39,40,41], the most prevalent psychosocial factor of interprofessional violence was "harassment with role discrepancy".
The differences between our study and those of other countries reflect that interprofessional violence is very specific and contextual [13], showing that the hierarchy of factors by geographical region of Peru is relevant. This is because it involves healthcare centers with different characteristics.
Specifically, the second and third hierarchy of factors for the Sierra Region, "harassment followed by role discrepancy", correspond to higher risk factors in Chinese health centers [17] and American health institutions [10,13].
Theoretical perspective
From a theoretical perspective, the results of the consensus on the pattern of psychosocial factors for interprofessional violence are circumscribed in Karasek’s demand-control-support model of the psychosocial work environment [18,19]. This theoretical adherence for work environments of different types of health service, delimited by geographic region, has correspondence with the following theoretical presupposition: high levels of stress and low work well-being, where there are high work demands with low control of psychosocial factors, together with low socioemotional and organizational support.
The dimensionality of our results is based on five theoretical assumptions (Annex 1c). In summary, the consensus of the pattern of interprofessional violence based on Karasek’s model [18,19] explains that the interaction between job demands, control over one’s work, and social support are essential for understanding interprofessional violence in the health sector.
These factors predict a psychosocial environment that favors the emergence of interpersonal conflicts, especially when job demands are high, control is low, and social support among colleagues or superiors is insufficient. It is also aligned with high work demands characterized by high time pressure, intense workload, and high expectations from superiors. It also aligns with low autonomy for decision-making and low participation of subordinates.
In the face of the complex nature of interpersonal conflicts [10,24] and the dynamics of the hierarchy of interprofessional violence factors according to occupational groups, an environment of low socioemotional and organizational support is intensified, and complaints are underestimated. For example, in these cases, reporting is not considered for fear of retaliation from colleagues or superiors [24], stigma, and lack of effective sanctions for perpetrators [20].
We suggest a theoretical adjustment to identify common elements of variability and stability of interprofessional violence factors according to cultural and geographical differences. As an implication of the findings, we suggest exploring the interaction between contextual variables such as organizational culture and individual factors [29].
The main strength of our study is its broad participation of experts from different types of health facilities in the three Peruvian geographic regions, which have different health and work environments. These hierarchical patterns are important for developing intervention programs [30] to reduce interprofessional violence in a coherent and contextualized way in the country’s healthcare institutions. This is the first consensus study where a hierarchical list of nine psychosocial factors of interprofessional violence according to geographic regions was determined.
Limitations
The ranking of the factors duplicated or triplicated in the third Delphi round could be misleading as the "most important" factor. Therefore, to reinforce the base "most frequent" slogan, these were repeated before (twice) and after the third Delphi round. In addition, the number of participants per analysis group belonged to the same level of care of the health facility and was distributed in the country’s three geographic regions, including rural health centers. However, the interventions should be approached considering the hierarchy of factors at the level of the analysis group.
The sample size studied (32 groups/444 experts) exceeded the established minimum of three groups and four experts per Delphi analysis group) [39,41], which guarantees good results against self-reports with response biases [21]. Overall, 17.3% (93/537) of participants were lost due to attrition of interest for a study of three rounds of consultation spaced over nine months.
Conclusions
Our findings contribute to further characterization of interprofessional violence, which may create the basis for the generation of policies for assessment, intervention, and monitoring of psychosocial health in healthcare work, constituting the foundation for generating coherent and contextualized designs of intervention protocols. These protocols should involve local professionals and be differentiated by geographic region and work characteristics.
Specifically, to prevent interprofessional violence of harassment, it is suggested in the first instance to carry out interventions based on awareness-raising to denounce, complementing the legal accompaniment with emotional support and solidarity among the interprofessional team. In addition, it is essential to carry out a summary of interpersonal conflict management with the intervention of third parties.
Finally, we suggest developing comparative Delphi studies with departments not included in this study and other labor sectors.

