Estudios originales
← vista completaPublicado el 23 de diciembre de 2024 | http://doi.org/10.5867/medwave.2024.11.3004
Acceso a medicamentos y satisfacción con la atención recibida en usuarios de establecimientos de salud: estudio transversal de una encuesta poblacional peruana
Access to medicines and patient satisfaction in healthcare facilities: A cross-sectional study of a Peruvian population-based survey
Abstract
Introduction Shortage of medicines in Peruvian healthcare facilities is a significant public health issue that may affect patient satisfaction.
Objective To estimate the association between access to medicines and the level of satisfaction with the received care from users of healthcare facilities in Peru during 2016.
Methods An analytical cross-sectional study was conducted using data from the 2016 National Survey of User Satisfaction in Health (ENSUSALUD). Access to medicines at the healthcare facilities' pharmacy and patient satisfaction were measured using self-report questions. Crude and adjusted ordinal logistic regression models were used to estimate Odds ratios with 95% confidence intervals. The complex sample design of the 2016 National Health User Satisfaction Survey was considered in all calculations.
Results Data from 10 386 healthcare facility users were included. After receiving medical care, 19.6% had partial access to medications, 6.8% had no access, and 6% were dissatisfied with the care received. Users with partial access to drugs had 87% higher odds of dissatisfaction (Odds ratio: 1.87; 95% confidence interval: 1.56 to 2.23), while users without access to medications had 51% higher odds of dissatisfaction (OR: 1.51; 95% CI: 1.06 to 2.16), compared to users with full access to drugs, adjusted for confounding variables.
Conclusions Patients with limited access to medicine at pharmacies in Peruvian healthcare facilities reported higher dissatisfaction with the care received.
Main messages
- In Peru, poor access to medicines may influence patient satisfaction.
- This is one of the first investigations to show that access to medicines could be an important predictor of user satisfaction.
- Limitations are the age of the data and the difficulty in inferring causality in a cross-sectional study.
Introduction
The World Health Organization (WHO) states that fair access to medicines benefits the community’s health and economic indicators. Good quality medicines, vaccines, and medical devices are necessary for the proper functioning of healthcare systems [1]. However, shortages and stock-outs of essential medicines have increased worldwide in recent years, primarily affecting the supply of antibiotics and chemotherapeutics [2]. The reasons for these shortages can be grouped into four groups: market, supply chain, manufacturing, and political issues [3]. Drug shortages can compromise treatment adherence and lead to unnecessary use of second or third-generation drugs, resulting in increased drug resistance and limited therapeutic options [2].
In Peru, there are primarily four healthcare systems: the State, through the Ministry of Health, offers subsidized individualized healthcare services to the uninsured population through Comprehensive Health Insurance; the Social Security Health System offers healthcare services to the salaried population and their families in its own facilities; the military, the police and their families receive healthcare through the Armed Forces and National Police healthcare facilities; and finally, private establishments (clinics, medical centers, polyclinics, medical and dental offices, etc.) [4,5]
The Peruvian healthcare system, particularly the Ministry of Health hospitals, has several deficiencies hindering high-quality patient care. For example, there is a shortage of essential drugs, such as antihypertensives, antidiabetics, antibiotics, immunomodulators, and oncological drugs [6]. Behind the shortages is the lack of management capacity, which results in poor budget execution for drug procurement. This leads to an oversupply of some drugs and a shortage of others. This is compounded by the deterioration of medicines due to non-compliance with good storage practices [6,7]. Consequently, users have to purchase these drugs in private pharmacies and drugstores to the detriment of their finances [7]. It is estimated that 63% of these private purchases come from public healthcare facilities: 39% from the Ministry of Health, 20% from the Social Security Health System, and 4% from the Armed Forces and National Police [8].
Patient satisfaction is an important indicator used to assess healthcare service quality [9,10]. This indicator has been measured by “satisfaction surveys” implemented by healthcare facilities worldwide. These surveys allow healthcare providers to identify service factors that need to be improved. Higher satisfaction favors adherence to treatment and its monitoring through follow-up appointments [9]. Satisfaction is a complex and dynamic concept; its associated factors depend on the hospital environment, which is variable and modifies satisfaction. In addition, the type of hospital (public, private, or specialized) and the countries' geographical regions also significantly influence patient satisfaction [11].
Access to healthcare and medicines has significant public health implications for developing countries such as Peru since they improve the population’s quality of life [12]. Low satisfaction levels may mean people do not access healthcare facilities on time when they get sick, increasing the risk of future complications. To our knowledge, this is one of the few studies that assesses access to medicines as a significant predictor of patient satisfaction.
Therefore, this study aimed to estimate the association between access to medications and the level of satisfaction with the care received by users of healthcare facilities in Peru during 2016. In addition, the differences in this possible association between healthcare systems were evaluated.
Methods
Design and population
We conducted a cross-sectional analytical correlational study of secondary data from the National Survey of User Satisfaction in Health (ENSUSALUD) 2016. The population consisted of users who attended any healthcare facilities in Peru in 2016.
Context
The National Institute of Statistics and Informatics and the National Superintendence of Health conducted the National Health User Satisfaction Survey 2016. Questionnaire No. 1, “aimed at outpatient users,” was used to meet the study’s objective. Its purpose was to provide information on users' perceptions and experiences regarding the medical care received in 184 healthcare facilities of the Ministry of Health, the Social Security Health System, the Armed Forces and National Police, and private facilities [13].
The 2016 National Health User Satisfaction Survey sampling was probabilistic, two-stage, stratified, and independent of each department. The sample size was calculated according to the 2015 National Health User Satisfaction Survey results. That instrument found that 26.3% of users were unsatisfied with the service. For this purpose, the formula for determining the sample size in finite populations was used. The levels of inference were national and regional. More information on the methodology of the 2016 National Health User Satisfaction Survey can be found in its final report [13].
Selection criteria
This analysis included data from patients aged 18 years or older who were prescribed medication during medical consultations. Users with incomplete or inconsistent data were excluded.
Variables
Access to medications was measured by asking, “At this facility’s pharmacy, were you given the medications you were prescribed?” The response alternatives were “all, most, some, and none.” This variable assumed three categories: total access (all), partial access (most and some), and no access to medicines (none). This method of measuring this variable has been used in similar studies [14,15].
Satisfaction with the received service was measured with the question, “Regarding the service received today at this facility, how would you rate your level of satisfaction?” whose response alternatives were “very satisfied, satisfied, neither satisfied/nor dissatisfied, dissatisfied and very dissatisfied”. This variable assumed three categories: satisfied (very satisfied, satisfied), indifferent (neither satisfied/nor dissatisfied), and dissatisfied (dissatisfied and very dissatisfied). As in the previous case, the method of measuring this variable has already been used in studies of this type [16,17].
We included sociodemographic exposure variables such as sex (male and female), age groups (18 to 29, 30 to 44, 45 to 59, and 60 years and older), educational level (no education/primary, primary, secondary and higher), origin (coastal region, highland region, jungle region, and metropolitan Lima), healthcare system (Ministry of Health, Social Security Health System, Armed Forces and National Police and private facilities).
We also included confounding variables recognized according to the review of previous studies, such as the usual language “What is the language in which you communicate at home?” (Spanish, Quechua or other) [18], chronic disease “Do you suffer from a chronic disease or discomfort? “ (no and yes) [19], medical explanation 'did the physician explain you about your illness, problem or health condition?” (yes and no) [20], scheduled appointment 'was the appointment or appointment for this health care given to you today?” (no and yes) [21] and waiting time (difference in hours from entering the healthcare facilities to entering the doctor’s office) [16]. In addition, the healthcare system was considered an effect modifier since the main association is evaluated according to these systems.
Statistical analysis
The database was downloaded from the National Superintendence of Health website and imported into the STATA Standard Edition version 18 statistical program. According to their normal distribution, quantitative data were presented as means and standard error. The bivariate analysis evaluated differences in satisfaction levels with the Chi-square and Wald tests. In the multivariate analysis, ordinal logistic regression was performed to evaluate the magnitude of the association between access to medicines and level of satisfaction (satisfied, indifferent, and dissatisfied). Odds ratios with their 95% confidence intervals were calculated. Two models were developed based on statistical criteria: a crude model, whose variables with a P value < 0.25 (in any category) were included in the adjusted model. The multicollinearity in the fitted model was assessed with the manual calculation of the variance inflation factor, whose value greater than five was considered to indicate multicollinearity. All results were weighted according to the strata, expansion factors, and design effect from the complex sampling of the National Health User Satisfaction Survey 2016 [13]. Also, the “svy” command of STATA’s “survey data analysis” module was used. A P value < 0.05 was accepted as statistically significant. Additionally, according to healthcare systems, a “forest plot” was used to visualize the magnitude of the association between access to medicines (access and non-access) and patient satisfaction.
Ethics
An institutional ethics committee reviewed and exempted the project from evaluation, given that the analyzed information came from a public database.
Results
The database contains information on 13 814 users. A total of 3428 were excluded because they did not meet the inclusion criteria (2589 people who were not prescribed medication during the consultation, 434 did not complete the procedure, 398 were under 18 years of age, and 7 had inconsistent data in the variable “educational level”), leaving 10 386 users for the final analysis.
Most of the users were women (59.5%), belonged to the 30 to 44 age group (27.0%), had a higher level of education (44.2%), came from Metropolitan Lima (44.2%), and attended a public healthcare facility (43.3%). Likewise, 97.3% spoke Spanish as their native language, 56.7% suffered from a chronic disease, 94.4% reported that the physician explained their disease or health condition, and 51.8% indicated that the appointment was given to them on the same day. The average waiting time was 1.5 (standard error: 0.024) hours. A total of 73.6% had full access to medications, 19.6% had partial access to medications, and 6.8% had no access (Table 1). Also, 74% (n = 7454) felt satisfied, 20% (n = 2167) felt indifferent, and 6% felt dissatisfied with the received care.
Table 1 shows that the percentages of dissatisfaction with the received service increased in line with the lack of access to medicines, going from 4.5% in users who received all their medicines to 10.3% in those who did not receive any of them.
In the crude model, users with partial access to medications had 2.07 times the odds of dissatisfaction (regarding feeling satisfied and indifferent) with the received service (OR 2.07; 95% CI 1.75 to 2.44), and users without access to medicines had 45% higher odds of dissatisfaction (concerning feeling satisfied and indifferent) with the received service (OR 1.45; 95% CI: 1.01 to 2.07), compared to users who had full access to medicines in the pharmacies of healthcare facilities in Peru (Table 2).
In the model adjusted for sex, age group, educational level, origin, health institution, chronic disease, medical explanation, scheduled appointment, and waiting time, users with partial access to medications had 87% higher odds of dissatisfaction (concerning feeling satisfied and indifferent) with the service received (OR: 1.87; 95% CI: 1.56 to 2.23). In turn, users without access to medicines had 51% higher odds of dissatisfaction (regarding feeling satisfied and indifferent) with the service received (OR: 1.51, 95% CI: 1.06 to 2.16) compared to users who had full access to medicines in Peruvian pharmacies (Table 2). No multicollinearity was found among the variables in the adjusted model (VIF ≈ 3).
When stratified by the healthcare system, it was found that the highest percentages of access to medicines were in the Social Security Health System (87.2%). The lowest was in the public sector (59.6%), while the percentages of satisfaction were highest in private facilities (91.4%), and the lowest was in public facilities (66.5%). It should be noted that only in the Social Security Health System facilities were the percentages of access to medicines higher than the percentages of satisfaction (Figure 1). In the stratified analysis of the adjusted model, lack of access to medicines was associated with greater patient dissatisfaction, but only in public (OR: 1.99; 95% CI: 1.62 to 2.45) and in social security facilities (OR: 1.48; 95% CI: 1.06 to 2.07) (Figure 2).
Percentages of access to medicines and patient satisfaction with the received care by the healthcare system.
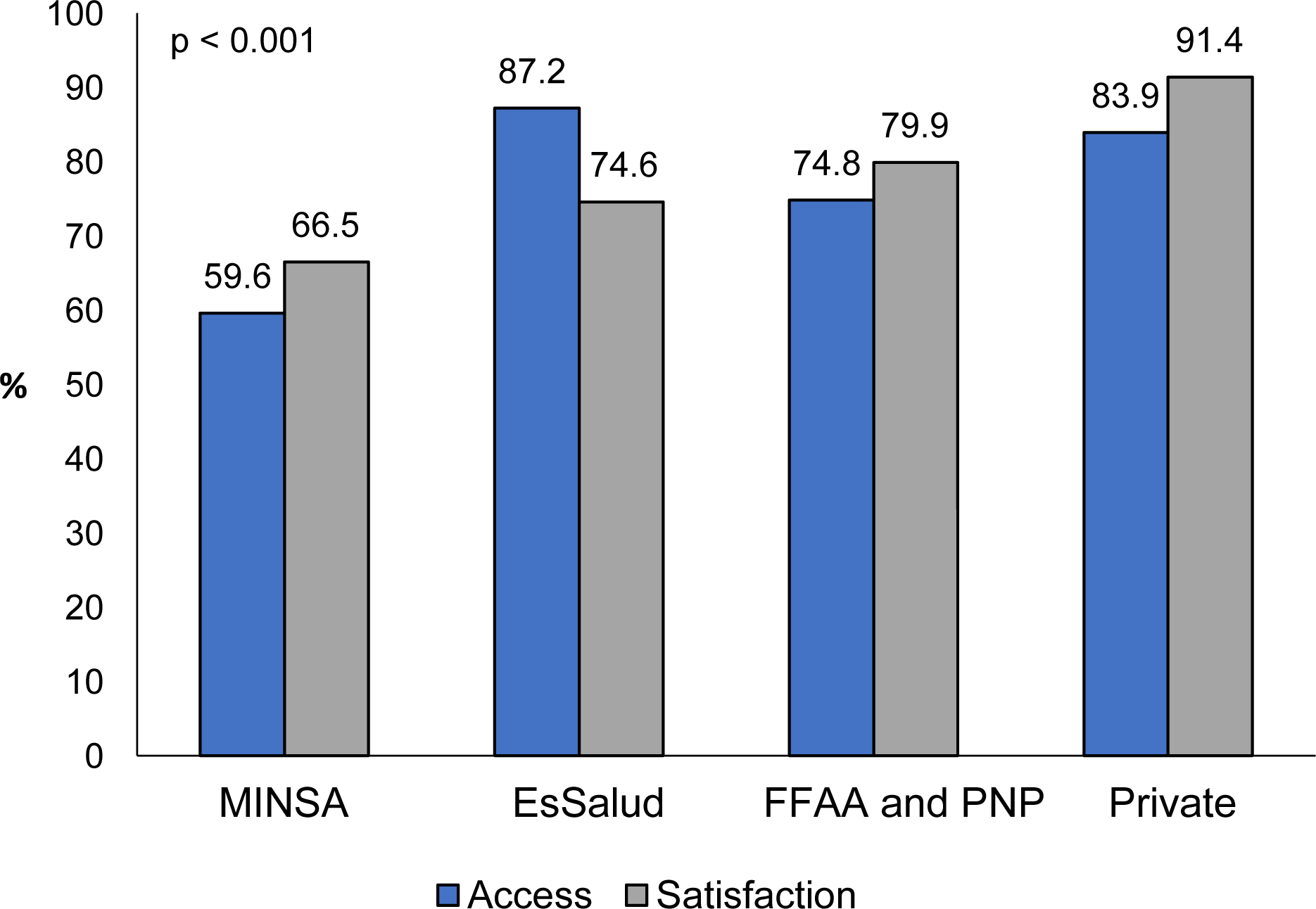
Source: Prepared by the authors based on the results of the study.
Association between access to medicines and satisfaction with the service received (adjusted model), stratified by healthcare system.
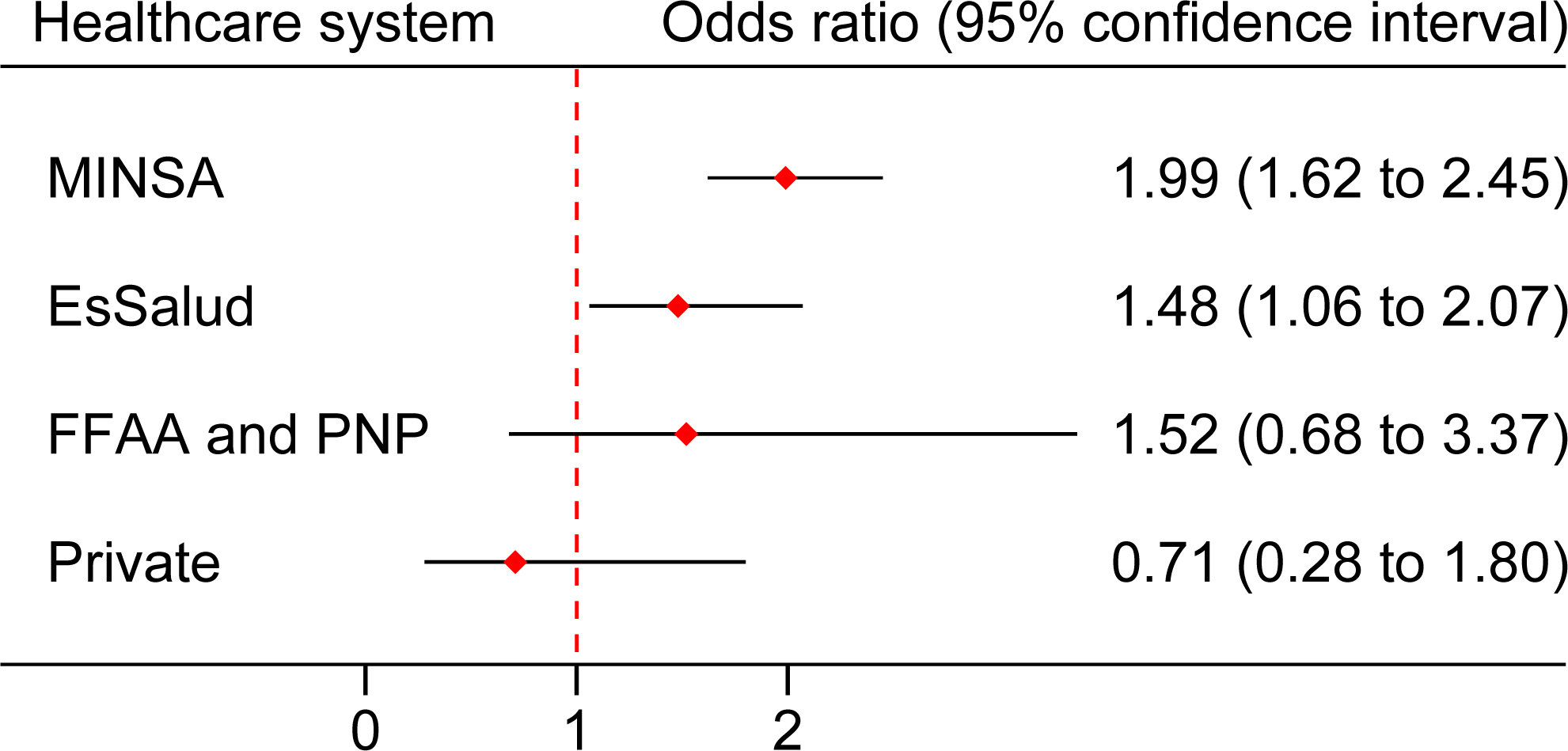
MINSA: Ministry of Health, EsSalud: Social Health Insurance, FFAA, and PNP: Armed Forces and Police Health System.
Source: Prepared by the authors based on the results of the study.
Discussion
A quarter of the users had incomplete or no access to medicines at pharmacies. Also, 6% were dissatisfied with the service they received. Users with partial or no access to medicines were more likely to be dissatisfied with the service received. This association was only present in the Ministry of Health and the Social Security Health System facilities.
A study that analyzed household surveys in three Central American countries (Nicaragua, Honduras, and Guatemala) found similar figures for lack of access to medicines among people with chronic diseases. It is important to mention that in these countries, most medicines are obtained from the private sector [22]. Similarly, a study that evaluated access to medicines in a representative sample of primary care services in Brazilian cities, with data obtained through patient interviews, reported total access to medicines of 59.8%, partial access of 35.9%, and no access of 4.3% [23]. In addition, an Argentine study that included 485 users of the public healthcare system of La Rioja reported that 24.1% had difficulty accessing their medication [24]. All these studies show similar proportions of lack of medication access in several Latin American countries. As a result, it can be inferred that this is an emerging problem that affects the regional healthcare systems.
In general, most users were satisfied with the care they received and only 6% were dissatisfied. This result is consistent with previous studies. For example, an analysis in 14 206 adults who participated in the National Household Survey on Living Conditions and Poverty 2018 found 74.3% satisfaction with the service received (good and very good) when they attended any public healthcare facility [25,26].
The main finding of this study shows that users with partial or no access to medicines were more likely to have greater dissatisfaction with the received service. In this regard, similar research conducted on 580 people in Brazil found that the availability of medicines in the pharmacy significantly influenced higher satisfaction scores, mainly in private facilities [27]. It has been described that the absence of medications, especially essential ones, can lead to underutilization and dissatisfaction with the care received, adding to distrust in public healthcare facilities [28]. It is important to mention that there is the possibility of reverse causality. This means that users who feel dissatisfied with the care received may decide not to take the medications prescribed by the physician. To illustrate this, a study of 4879 adults in the United States who participated in a telephone survey assessing the use of healthcare services found that users who were dissatisfied with the physician’s care were more likely not to purchase the prescription [29].
The lowest percentages, both in terms of access and satisfaction, were found in MOH facilities. The lack of essential drugs may explain this result. On the other hand, it is striking that in the Social Security Health System, the percentages of access to medicines are higher than the percentages of satisfaction with the care received. This finding suggests the existence of other factors that influence user satisfaction. The main reasons are the poor quality of care, longer time to access an appointment (almost twice as long as in the Ministry of Health), and lack of trust in the institution [30].
Lack of access to medicines was associated with greater dissatisfaction with the care received, but only in public and social health facilities. The magnitude of the association observed in Ministry of Health facilities suggests that lack of medicines is an important predictor of user dissatisfaction. While in the Social Security Health System, other factors could explain greater dissatisfaction due to the lower magnitude of the association. This is despite the fact that it is the institution with the greatest access to medicines. These exploratory findings should be corroborated with primary studies designed to evaluate the factors associated with patient satisfaction, individually in the Ministry of Health or in the Social Security Health System, since the differences between the two systems are evident.
Public health implications
Drug shortages in public healthcare facilities can lead to higher out-of-pocket costs for users when they turn to private pharmacies or apothecaries, especially among patients suffering from multiple diseases [31]. In addition, some users may have access to cheap but lower quality or even counterfeit drugs. This could increase the risk of adverse drug reactions due to the use of undeclared or toxic substances [32]. Another problem is the possibility of changing or altering medical treatment, including administering incomplete doses of antibiotics, which can lead to antimicrobial resistance [33,34]. The lack of availability of medications may lead people to resort to the services of quacks or homeopaths, risking health due to the lack of scientific evidence to support these treatments, along with delaying or avoiding conventional medical therapies [35]. Limited or no access to medicines can cause great patient dissatisfaction. This, in turn, can lead to treatment noncompliance and abandonment of medical follow-up, increasing the risk of future complications [36].
Strengths and limitations
For this work, the following limitations should be recognized. First, possible interviewer or recall biases could have increased or decreased the prevalence of access to medicines and satisfaction levels in the users interviewed. Second, residual confounding may exist because some variables related to satisfaction levels were unavailable in the 2016 National Health User Satisfaction Survey, so they were not included in the analysis. Third, the age of the data could lead to results that are not applicable today, especially after the COVID-19 pandemic. However, to our knowledge, no similar studies exist in the Peruvian context. Fourth, due to the cross-sectional design of the survey, causality between the study variables cannot be assumed.
As a strength, it should be recognized that this is one of the first studies to demonstrate that access to medicines could be an important predictor of user satisfaction. For this reason, future studies should include this variable, especially if they are carried out in countries with deficient health systems, such as Peru. Another strength of the study is that the National Health User Satisfaction Survey is a population-based survey. Consequently, the results are representative of all Peruvian healthcare facilities users.
Conclusions
In Peru, the lack of medicines in pharmacies harms user satisfaction. The likelihood of greater dissatisfaction is greater among users who do not receive or partially receive their medicine. These results show the need to improve access to medicines in the low-income population, who are treated in public or social security facilities. This is to achieve adequate levels of satisfaction that promote continuous care and adherence to treatment and avoid relapses or future complications.
It is recommended that these results be corroborated with primary studies that evaluate the impact of the lack of drugs on various outcomes, such as overall patient satisfaction, according to type of health insurance or others.
Metadata

