Estudios originales
← vista completaPublicado el 9 de enero de 2025 | http://doi.org/10.5867/medwave.2025.01.3015
Factores de riesgo sociodemográficos, conductuales y clínicos asociados a la displasia cervical: estudio de casos y controles
Sociodemographic, behavioral, and clinical risk factors associated with cervical dysplasia: A case-control study
Abstract
Introduction Cervical dysplasia is a precursor lesion of cervical cancer, one of the leading causes of morbidity and mortality in women, especially in developing countries. This study aimed to identify the risk factors associated with the development of cervical dysplasia in women treated at the Santa María del Socorro Hospital in Ica, Peru, between 2017 and 2019.
Methods An observational case-control study was conducted with 92 cases of women with confirmed high-grade intraepithelial lesion and 184 controls with consecutive negative results in Pap smears. Sociodemographic, behavioral, and clinical data were collected. Bivariate and multivariate logistic regression analyses were performed to identify factors associated with precancerous cervical lesions.
Results The factors significantly associated with cervical dysplasia were age under 35 years (odds ratio: 1.2; 95% confidence interval: 0.1 to 0.7), having a partner (7.4; 2.3 to 23.5), body mass index ≥ 25 (12.9; 3.9 to 42.0), more than three sexual partners (71.4; 16.4 to 310.9), bacterial vaginosis (101.2; 12.2 to 838.2), grand multiparity (39.0; 7.1 to 225.4), rural origin (0.2; 0.1 to 0.8), use of injectables (0.2; 0.1 to 0.6), and intrauterine devide (0.04; 0.01 to 0.2).
Conclusions Identifying these risk factors is crucial for cervical cancer prevention. It is recommended to implement early detection programs targeted at women with risk factors, especially those under 35 years and with multiple sexual partners.
Main messages
- In Peru, cervical cancer is the most frequent neoplasm among women, representing an important burden for the country’s health system. Improving early detection and treatment is essential to reduce the morbidity and mortality associated with this disease.
- This study provides valuable information on the risk factors for cervical dysplasia in a Peruvian population, thus contributing to the knowledge base necessary for the development of more effective prevention and early detection strategies.
- Some of the limitations of this study are the limited sample size, the inability to establish direct causal relationships between the factors identified and the development of cervical dysplasia because it is a case-control study, and the selection and recall biases, among others.
Introduction
Cervical cancer is one of the leading causes of morbidity and mortality among women worldwide, especially in developing countries. Despite global efforts to prevent human papillomavirus infections, the incidence of this invasive cancer has increased by 29% between 2000 and 2022, from 471 000 to 660 000 affected women [1,2]. This disease remains a significant threat to women’s health, causing more than 350 000 deaths annually and ranking fourth in terms of female incidence and mortality [2]. In Peru, cervical cancer is the most frequent neoplasm among women, with an incidence rate of 11.8 per 100 000 inhabitants [3], representing a significant burden for the country’s health system. Late detection is a significant problem in the country, as most women with cervical cancer are detected in advanced stages. In this regard, in 2021, 1162 women with cervical cancer were reported [4], and in 2022, a mortality rate of 8.8 per 100 000 women was recorded [1,5]. These data highlight the importance of improving early detection and treatment of cervical cancer in Peru to reduce the morbidity and mortality associated with this disease.
Strategy 907090 [6] was implemented in Peru to reduce maternal and neonatal mortality, including preventing and detecting cervical cancer [7]. However, improving early detection and treatment in the latter pathology country is necessary to reduce the associated morbidity and mortality [8].
Human papillomavirus - especially serotypes 16 and 18 - is the main etiologic agent of cervical cancer [7,8] and is responsible for approximately 70% of infections [8]. Infection with this virus is transmitted mainly through sexual contact. In addition, it can cause abnormal changes in the cells of the cervix, known as cervical dysplasia. These precancerous lesions, which can be low or high grade have the potential to progress to invasive cancer if not detected and treated early [9,10,11,12,13,14,15].
Several studies have identified several factors that increase the risk of developing cervical dysplasia and cervical cancer. These factors include early sexual debut, multiparity, sexually transmitted infections, low educational level, and specific behaviors and socioeconomic conditions [7,11,12]. In the Peruvian context, it is estimated that about 10% of women aged 17 to 64 years have some degree of cervical dysplasia [12], underscoring the importance of addressing these risk factors effectively.
In this study, we focused on women with cervical dysplasia to better understand the factors contributing to its development and progression. The selection of these women was based on the availability of data in the medical records at Santa Maria del Socorro Hospital, as well as the need to investigate a population that is at high risk for developing cervical cancer. By studying women with cervical dysplasia, we can identify patterns and trends that can help develop more effective prevention and treatment strategies for this condition.
This study analyzed the sociodemographic, behavioral, and gynecological factors contributing to precancerous cervical lesions in women seen at Hospital Santa María del Socorro from 2017 to 2019. The main objective was to provide solid evidence to support the design of effective interventions and formulate public policies to reduce cervical cancer incidence and mortality in the region significantly. It is expected to find that certain factors, such as rural origin, multiple sexual partners, and multiparity, are significantly associated with an increased risk of cervical dysplasia. In addition, it is proposed that sexual behaviors, such as early sexual debut and sexually transmitted infections, increase the likelihood of developing precancerous lesions. This study is crucial to improve prevention and early detection programs, particularly in vulnerable populations.
Several sociodemographic, behavioral, and gynecologic factors were evaluated as possible risk factors for cervical dysplasia, including age, marital status, education level, background, body mass index, number of sexual partners, bacterial vaginosis, high multiparity, injectable use, and intrauterine device use. These factors were selected because of their potential relationship to cervical dysplasia.
Methods
This observational, analytical, retrospective case-control study was conducted at the Santa María del Socorro Hospital in Ica, Peru, from 2017 to 2019. The hospital, classified as a category II-1 institution, provides specialized 24-hour patient care services, including gynecology and obstetrics. The information used in this analysis was collected and reviewed exclusively from pre-pandemic COVID-19 medical records.
The study population consisted of women aged 17 to 64 years who had been seen in the hospital’s gynecology, obstetrics, and cervical cancer screening program. Those women with a confirmed diagnosis of high-grade squamous intraepithelial lesion (CIN II and CIN III classification), determined by Papanicolaou test results and verified according to the Bethesda System [16], were selected as cases.
Controls consisted of women with at least two consecutive negative Pap test results performed two years before the study. All participants with a complete medical history and valid Pap smear results were included. Women with incomplete diagnoses or poor and illegible medical records were excluded. Since the study was conducted retrospectively, only information available in existing medical records was used.
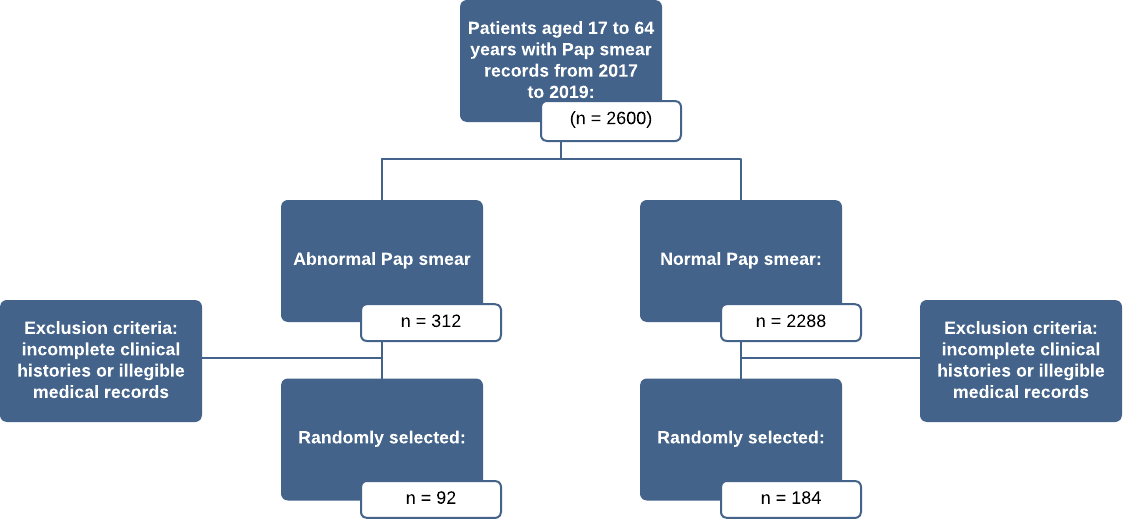
The selection process included a review of 2600 Papanicolaou records, of which 312 (12%) were identified as pathologic records and defined as cases. Of these, 92 cases were randomly selected for inclusion in the study. For the control group, 469 women who met the inclusion criteria were identified from among the 2288 nonpathologic records. That is, those who had at least two consecutive negative Pap smear records. From these, 184 controls were randomly selected, maintaining a ratio of two controls to each case to improve the accuracy of comparisons and to perform a robust analysis of risk associations. Random selection of cases and controls was key to minimizing bias and ensuring representation, ensuring the results were generalizable to the population of interest (Figure 1).
Risk factors associated with cervical dysplasia.
Source: Prepared by the authors based on the results of the study.
The main outcome was the presence of cervical dysplasia, defined as high-grade squamous intraepithelial lesions (CIN II and CIN III) confirmed by the Papanicolaou test, using the Bethesda System as diagnostic criteria. The independent variables included sociodemographic characteristics (age, marital status, educational level, geographic origin, and body mass index), behavioral factors (age of sexual debut, number of sexual partners, condom use), infectious factors (history of sexually transmitted infections and bacterial vaginosis), and reproductive factors (number of births and use of intrauterine devices). Potential confounding variables, such as age, educational level, geographic origin, marital status, and body mass index, were considered, and statistical analyses were adjusted to control for their influence on the relationship between risk factors and cervical dysplasia.
Data collection was performed through a retrospective review of the medical records of patients undergoing the Papanicolaou procedure at the Hospital Santa María del Socorro between 2017 and 2019. A panel of five experts validated a data collection form designed for this study to minimize errors. Data were collected systematically and standardized, ensuring consistency in measurement and collection procedures for both groups. Medical records were thoroughly reviewed to ensure the accuracy and completeness of information. A coding system was also implemented to maintain the confidentiality of the data, which was stored in a secure database.
In this study, measures were taken to mitigate possible effects and ensure the validity of the results. To minimize selection bias, all cases of cervical dysplasia diagnosed in the hospital during the study period were included, and controls were randomly selected from the population that met the inclusion criteria. The information message was controlled by a thorough review of medical records, checking for consistency of information from multiple sources. In addition, a standardized diagnostic criterion based on the Bethesda classification was confirmed by an expert pathologist, reducing detection bias.
Statistical analysis included Chi-square tests to evaluate associations between qualitative variables and Student’s t-test to compare quantitative variables. Odds ratios with 95% confidence intervals were calculated to measure the strength of associations. Subsequently, multiple logistic regression models were applied to adjust associations for possible confounding variables. These association adjustments were performed using variable selection procedures to identify the most relevant predictors, with an assessment of the fit using the Hosmer-Lemeshow test. Although the limitations of automatic variable selection methods are acknowledged, additional methods are taken to control the influence of key variables and minimize bias.
While it would have been useful to perform additional analyses to assess effect modification and control for confounding, particularly concerning the directionality of some adjusted odds ratios, this was not possible due to sample size and model complexity limitations. However, the results provide an overview of the associations between the variables studied and the presence of cervical dysplasia.
Multicollinearity was assessed by calculating the variance inflation factor, considering values greater than 10 indicative of significant collinearity. This led to the exclusion of age and educational level variables due to their high ranking with other variables. To minimize selection bias, all cases of cervical dysplasia were included, and controls were randomly selected. The quality of the medical records was verified by systematic reviews and confirmation of diagnoses by an expert pathologist, following standardized criteria according to the Bethesda classification.
The sample size was calculated using the statistical program Epi Info 7.2.3, considering a significance level of α = 0.05, a statistical power of 80% (1-β = 0.80), and a ratio of two controls per case. Having had more than three sexual partners was selected as an exposure factor because of its strong association with human papillomavirus infection, the leading etiological agent of cervical dysplasia, and because it is supported in the scientific literature [12]. The estimated proportion of exposure in controls (PC = 8.7%) was calculated from the data of this study. An odds ratio of 2.0 was considered the minimum magnitude of association we sought to detect with statistical precision for the sample size calculation. With these parameters, it was determined that a sample size of 92 cases and 184 controls was sufficient to evaluate the association between this exposure factor and the outcome, maintaining an adequate level of confidence and precision.
Statistical analysis was performed using SPSS version 26 software (IBM SPSS Statistics for Windows).
Results
The mean age for cases was 28.7 years (standard deviation = 7.6), while for controls it was 36.4 years (standard deviation 8.3).
Table 1 shows the sociodemographic and body mass index risk factors associated with cervical dysplasia in women seen in a Peruvian hospital between 2017 and 2019. Among the 92 cases in the study, 52.2% corresponded to women under 35, compared to 21.7% of controls in this age group. Women younger than 35 years have a significantly lower probability of developing cervical dysplasia compared to the group of women older than 35 years (crude odds ratio = 0.25; 95% confidence interval: 0.14 to 0.45; p < 0.001).
Regarding marital status, 68.5% of the cases and 31.5% of the controls were in a couple. Women in a couple had a significantly higher probability of developing cervical dysplasia compared to women without a partner (crude odds ratio = 5.2; 95% confidence interval: 2.5 to 11.1; p < 0.001).
Regarding body mass index, 64.1% of cases had a body mass index equal to or greater than 25, compared with 25% of controls. Women with a body mass index equal to or greater than 25 had a significantly higher probability of developing cervical dysplasia than women with an index between 18.5 and 24.9 (crude odds ratio = 5.4; 95% confidence interval: 3.0 to 9.6; p < 0.001).
Regarding origin, 27.2% of the cases came from rural areas, while only 14.7% of the controls shared this origin. Women coming from rural areas had a significantly higher probability of developing cervical dysplasia compared to women coming from urban areas (crude odds ratio = 2.2; 95% confidence interval: 1.1 to 4.2; p = 0.012).
The analysis in Table 2 shows that women who initiated their sexual life before the age of 17 years have a significantly higher probability of developing cervical dysplasia compared to women who initiated their sexual life at 17 years or older (crude odds ratio = 3.1; 95% confidence interval: 1.6 to 5.9). In addition, having more than three sexual partners (crude odds ratio = 29.8; 95% confidence interval: 16.4 to 310.9), a history of sexually transmitted infections in the past five years (crude odds ratio = 44.5; 95% confidence interval: 16.2 to 149.1) and the presence of bacterial vaginosis (crude odds ratio = 70; 95% confidence interval: 12.2 to 838.2) were found to be strongly associated with an increased likelihood of developing cervical dysplasia. On the other hand, using an intrauterine device is associated with a lower probability of developing cervical dysplasia (crude odds ratio = 0.3; 95% confidence interval: 0.01 to 0.2).
Multivariate analysis confirmed that age at first intercourse, number of sexual partners, history of sexually transmitted infections in the last five years, and the presence of bacterial vaginosis and number of deliveries were independent factors significantly associated with a higher probability of developing cervical dysplasia. In addition, the use of injectable contraceptive methods and intrauterine devices was significantly associated with a lower probability of developing cervical dysplasia.
Multivariate analysis showed that several factors were significantly linked to the likelihood of developing cervical dysplasia. Age, marital status, origin, body mass index, number of sexual partners, bacterial vaginosis, and number of deliveries were associated with a higher probability of cervical dysplasia. On the other hand, the use of injectable contraceptive methods and intrauterine devices was associated with a lower probability of developing cervical dysplasia.
In particular, having a partner was associated with a significantly higher probability of cervical dysplasia (adjusted odds ratio = 7.4; 95% confidence interval: 2.3 to 23.5). Rural origin was identified as a protective factor (adjusted odds ratio = 0.2; 95% confidence interval: 0.1 to 0.8). A body mass index equal to or greater than 25 was associated with a significant increase in the likelihood of cervical dysplasia (adjusted odds ratio = 12.9; 95% confidence interval: 3.9 to 42.0), as was having more than three sexual partners (adjusted odds ratio = 71.4; 95% confidence interval: 16.4 to 310.9). Having three or more deliveries was also associated with a significant increase in the likelihood of cervical dysplasia (adjusted Odds ratio = 39.0; 95% confidence interval: 7.1 to 225.4). Bacterial vaginosis was associated with an extremely high risk (adjusted Odds ratio = 101.2; 95% confidence interval: 12.2 to 838.2). In contrast, the use of injectables (adjusted Odds ratio = 0.2; 95% confidence interval: 0.1 to 0.6) and intrauterine devices (adjusted Odds ratio = 0.04; 95% confidence interval: 0.01 to 0.2) showed a significant protective effect against cervical dysplasia (Table 3).
Discussion
Early detection and treatment of precancerous cervical lesions are critical to prevent progression to cervical cancer. This study evaluated factors associated with precancerous cervical lesions in women treated at the Santa María del Socorro Hospital in Ica, Peru, identifying several significant predictors.
One of the most relevant findings was that women younger than 35 years had a higher probability of developing cervical dysplasia, in agreement with previous studies suggesting a higher prevalence of human papillomavirus infections in young women [7,17]. However, a higher prevalence of human papillomavirus has also been observed in women older than 57 years, possibly due to age-related alterations in the immune response [18]. Different mechanisms could explain this apparent discrepancy. In younger women, the high prevalence could be due to increased sexual activity and exposure to human papillomavirus, whereas in older women, decreased immunity due to aging could be a predisposing factor for the appearance of precancerous lesions [18,19].
Having a partner showed a significant association with an increased likelihood of cervical dysplasia (adjusted odds ratio = 7.4; 95% confidence interval: 2.3 to 23.5; p = 0.001). This result suggests that partnered women may have a higher risk of exposure to HPV, which could be related to earlier sexual debut and longer duration of HPV exposure in married women or women in stable relationships [20,21]. However, other studies have found that single status may also influence patterns of sexual behavior and exposure to HPV [8,11,21]. This highlights the complexity of this factor and the need to consider the sociocultural context in interpreting these results.
In contrast to what was expected, our study found that rural origin was associated with a lower probability of cervical dysplasia (adjusted odds ratio = 0.2; 95% confidence interval: 0.1 to 0.8; p = 0.024). This finding is contrary to that reported in previous studies, which suggest a higher probability of cervical dysplasia in rural areas due to lower access to health services [22,23]. This difference could be explained by recent changes in sexual behavior, improvements in education, and access to health services in rural Peru [24]. This result underscores the importance of considering sociodemographic and health infrastructure changes in analyzing risk factors for cervical dysplasia.
The association between high body mass index and the likelihood of cervical dysplasia has been the subject of several studies, yielding complex and sometimes seemingly contradictory results. Our investigation revealed a significant correlation between a body mass index equal to or greater than 25 and an increased likelihood of cervical dysplasia (adjusted odds ratio = 12.9; 95% confidence interval: 3.9 to 42; p < 0.001). This observation finds support in previous research, which suggests that both overweight (body mass index of 23 to 25 kilograms per square meter) and obesity (body mass index equal to or greater than 25 kilograms per square meter) may increase the likelihood of cervical cancer [25,26].
However, the relationship between body mass index and cervical health is not unidirectional. Paradoxically, some studies have documented that women with an abnormal BMI tend to undergo Pap smears less frequently compared to those who maintain an optimal BMI. This trend could at least partially explain the apparent correlation between obesity and increased risk of cervical cancer, as the lower frequency of screening in obese women could result in underdiagnosis of precancerous lesions.
It is important to note that although a lower frequency of screening has been observed in obese women, direct causality between obesity and cervical cancer development has not yet been definitively proven [26]. Nevertheless, this association highlights the need to pay special attention to screening strategies in women with high body mass index. In this regard, improvements in equipment and examination techniques that ensure adequate sampling and visualization in women with higher body mass could contribute significantly to reducing the incidence of cervical cancer in this population group.
The number of sexual partners emerged as one of the strongest associated factors, with women who reported more than three-lifetime sexual partners having a significantly increased likelihood of cervical dysplasia (adjusted odds ratio = 71.4; 95% confidence interval: 16.4 to 310.9; p < 0.001). This finding is consistent with numerous studies that have shown that a greater number of sexual partners increases exposure to human papillomavirus and, therefore, the likelihood of cervical dysplasia [8,10,22,27,28].
Bacterial vaginosis was identified as a significant factor for cervical dysplasia (adjusted odds ratio = 101.2; 95% confidence interval: 12.2 to 838.2; p < 0.001). Although the exact mechanism by which bacterial vaginosis may influence the acquisition of cervical human papillomavirus infection is still unknown, it is postulated that it may facilitate infection and persistence of this high-risk virus [29,30]. However, some studies have not found a significant association between bacterial vaginosis and human papillomavirus infection in cervical lesions [31,32]. The differences in the results of the studies could be explained by the presence of other confounding factors such as age, immunity, number of sexual partners, douching, use of pessaries, and smoking [33,34], which highlights the need for further research in this area.
The study also showed that being large multiparous (more than three deliveries) increases the likelihood of cervical dysplasia (adjusted odds ratio = 39; 95% confidence interval: 7.1 to 225.4; p = 0.006). This finding is consistent with the literature, which suggests that high parity may be associated with hormonal and physical changes that increase susceptibility to human papillomavirus infections [35,36].
Regarding contraceptive methods, the use of injectables and intrauterine devices were identified as protective factors against cervical dysplasia. These findings contrast with some studies suggesting that prolonged use of hormonal contraceptive methods may increase the risk of cervical cancer [37]. However, other studies have found similar results, indicating a protective effect of certain contraceptive methods [32,33].
Concerning the intrauterine device specifically, our results are in line with recent research suggesting a protective effect against cervical dysplasia and cervical cancer. A meta-analysis by Cortessis et al. [38] found that IUD use was associated with a significant reduction in the likelihood of cervical cancer (odds ratio = 0.64; 95% confidence interval: 0.53 to 0.77) [38]. Similarly, a prospective cohort study by Averbach et al. [39] observed that intrauterine device use was associated with a lower incidence of high-grade precancerous lesions (CIN II) (adjusted odds ratio = 0.38; 95% confidence interval: 0.16 to 0.88).
Several mechanisms have been proposed to explain this protective effect of the intrauterine device. These include the induction of a local inflammatory response that could increase cellular immunity against human papillomavirus, mechanical removal of cervical lesions during insertion or removal of the intrauterine device, and increased cellular exfoliation that could eliminate human papillomavirus-infected cells [40]. However, it is important to note that the causal relationship is not yet fully established, and further studies are required to confirm these findings.
Limitations
Although this study has several significant strengths, it has some important limitations. The limited sample size may affect the validity of the results, and there may be confounding variables not included in the model that may affect the results. In addition, being a case-control study, direct causal relationships between the identified factors and the development of cervical dysplasia cannot be established.
The selection of cases and controls from a single hospital may have introduced a selection bias, limiting the generalizability of the results to the entire population of Ica. The retrospective nature of the study may have generated recall bias in data collection, especially regarding information on past sexual behaviors.
Other limitations include the lack of information on some known risk factors for cervical cancer, such as smoking, diet, and genetic factors, as well as the absence of data on the duration of exposure to certain risk factors. Although sufficient to detect significant associations, the sample size may have been limited for detailed stratified analyses in some subgroups.
Additional analyses to assess effect modification and confounding in the analyses would be useful, especially concerning changes in the directionality of some adjusted odds ratios. However, these additional analyses were not performed due to sample size limitations and model complexity.
Despite these limitations, this study provides valuable information on risk factors for cervical dysplasia in a Peruvian population, thus contributing to the knowledge base needed to develop more effective prevention and early detection strategies. It is recommended that future studies address these limitations through prospective designs, with larger and more diverse samples and the inclusion of a broader set of potentially relevant variables.
Conclusions
This study comprehensively examines risk factors for cervical dysplasia in a Peruvian population and provides crucial evidence for the development of cervical cancer prevention strategies in Peru and possibly in other Latin American countries with similar contexts. The findings underscore the importance of several key factors in the development of precancerous cervical lesions, including young age (especially women younger than 35 years), marital status, number of sexual partners, presence of bacterial vaginosis, and high parity.
Our results have significant implications for both clinical practice and public health policy. They suggest the urgent need to implement early detection programs specifically targeting high-risk groups, including more intensive screening for young sexually active women and the promotion of more frequent Pap smears for those with multiple sexual partners. In addition, the study highlights the importance of developing comprehensive educational campaigns that address the prevention of sexually transmitted infections, the importance of monogamy or reducing the number of sexual partners, and the need for regular Pap smears.
These interventions must be adapted to the specific sociocultural context of the Ica region and other similar areas in Peru, considering factors such as rural background and local contraceptive practices. The protective association found with certain contraceptive methods merits further investigation and could have important implications for family planning policies.
Despite the inherent limitations of a case-control study, such as the impossibility of establishing direct causal relationships, our findings provide a solid basis for future research. Prospective, multicenter studies are recommended, which may provide a better understanding of the causal relationship between the identified factors and the development of cervical dysplasia over time. It would also be valuable to explore the interaction between these risk factors and the presence of specific types of high-risk human papillomavirus in the Peruvian population and further investigate the protective role of certain contraceptive methods.

