Estudios originales
← vista completaPublicado el 26 de junio de 2025 | http://doi.org/10.5867/medwave.2025.05.3037
Análisis descriptivo de alteraciones inmunológicas en el fallo reproductivo recurrente y resultados terapéuticos
Descriptive analysis of immunological abnormalities in recurrent reproductive failure and therapeutical outcomes
Abstract
Introduction Reproductive immunology has advanced significantly, recognizing the immune system as crucial in pregnancy development and facilitating the identification of abnormalities causing recurrent reproductive failure, as well as proposing targeted treatments for these patients.
Methods This is a descriptive, observational, and retrospective study conducted at the Reproductive Immunology Unit of the Hospital Clínico San Carlos in Madrid. Clinical and analytical data were analyzed for patients diagnosed with recurrent reproductive failure between 2019 and 2023. Data on treatments received as prophylaxis for pregnancy loss and their success rates were also collected. Finally, a comparative study of the two major subgroups in the cohort was performed.
Results A total of 277 patients were included. The most prevalent diagnosis was recurrent miscarriage (64.2%), followed by recurrent implantation failure (25.2%). Immunological and/or vascular abnormalities were detected in 88.8% of patients. The most prevalent immunological abnormality was the expansion of cytotoxic natural killer cells (49.5%), followed by HLA-C-KIR mismatch (39.1%) and the presence of antiphospholipid antibodies (38.5%). The comparative study between the recurrent miscarriage and the recurrent implantation failure subgroups revealed statistically significant differences regarding the presence of antinuclear antibodies (15.4% vs. 28.3%, p=0.03) and vitamin D deficiency (37.2 vs 60.0%, p=0.01). The most commonly used medications were low-dose acetylsalicylic acid, low-molecular-weight heparin, hydroxychloroquine, and/or prednisone, with an overall success rate of 97.3%. Neither moderate nor severe side effects were reported.
Conclusions Immunological studies to identify causes of recurrent reproductive failure are highly useful in cases where other etiologies have been excluded. Targeted therapies for addressing these abnormalities have demonstrated significant effectiveness.
Main messages
- A significant number of patients present recurrent reproductive failure, in which immunological alterations may play a fundamental role, both in implantation and pregnancy course.
- This study includes an exhaustive compilation of the clinical data of our patients, with a detailed analysis of clinical factors, therapeutic interventions, and follow-up.
- A high percentage of patients presented immunological alterations that could justify recurrent reproductive failure.
- To strengthen the validity of the observed prevalences, further studies are warranted as these results may be limited due to the single-center population included.
Introduction
Reproductive immunology has gained prominence in the last decade, evolving from the initial conception of pregnancy as a state of immune tolerance towards the fetus to a deeper understanding of the active involvement of the immune system in all stages of pregnancy, from implantation to delivery [1,2,3,4].
This advance has prompted significant changes in therapeutic approaches to immune-mediated recurrent reproductive failure [5,6].
Important roles in reproduction have been gradually identified for various components of the immune system, including natural killer cells and other cell lineages, such as macrophages, granulocytes, T lymphocytes, and plasma cells [7,8,9,10]. In addition, a complex network of interrelationships between these cells and the extravillous trophoblast, essential for gestation, has been described as the "immunological code of pregnancy" [11]. Inflammation, although essential in implantation and delivery, when dysregulated, can contribute to obstetric complications such as infertility, recurrent miscarriage, intrauterine growth retardation, or preeclampsia [2,12,13,14,15,16,17].
Recurrent reproductive failure understood as the inability to achieve full-term gestation, is mainly classified into two entities: recurrent miscarriages and recurrent implantation failure when pregnancy is not achieved after assisted reproductive techniques. Its prevalence in the general population is between 2 to 5% in cases of repeated miscarriages [18] and up to 10% in the case of recurrent implantation failure [19]. The causes are diverse, including genetic, anatomical, hematological, infectious, endocrinological, and immunological factors, among others [20]. Additional risk factors such as maternal age, body mass index, or harmful lifestyle habits (smoking, chronic alcohol consumption, or stress) also contribute [21]. Autoimmune diseases can cause recurrent reproductive failure both because of the systemic inflammation they generate and because of direct damage to placental tissue. This is the case of antiphospholipid syndrome [22]. Hormonal alterations characteristic of autoimmune thyroid diseases and nutritional alterations associated with celiac disease also contribute to gestational complications [23,24].
These factors underscore the complexity of clinical management in patients with autoimmune or alloimmune conditions during pregnancy. Likewise, they emphasize the importance of a multidisciplinary approach to optimize reproductive outcomes. The correct management of these immunological alterations is crucial for the development of pregnancy, and multiple studies with various treatments have been conducted.
The primary objective of this study is to characterize the prevalence of immunological alterations in patients diagnosed with recurrent reproductive failure who are attended to at the Reproductive Immunology Unit of the Hospital Clínico San Carlos in Madrid. In a complementary way, we aim to evaluate the therapeutic response to the treatments used, considering modulatory factors that may influence the gestational prognosis.
Methods
Study design and context
An observational, descriptive, and retrospective study was conducted on all patients consecutively attending the Reproductive Immunology Unit of Hospital Clínico San Carlos de Madrid, a level III hospital. The analysis spanned the period from the unit’s opening at the beginning of 2019 to the end of 2023.
Participants and sample size
All patients seen in the specialized unit between 2019 and 2023 were included in the study, totaling 277. All patients were referred from other services within the National Health System, originating from various hospitals across the country, according to the criteria established by their gynecologists.
Patients without gestational search at the time of consultation were excluded, as well as those whose diagnosis did not meet the criteria for recurrent reproductive failure (see below).
Sources of information and management
Data were obtained through a manual review of the hospital’s electronic medical records by the first author. The following data were collected: age, personal medical history, family history of autoimmune diseases, cardiovascular diseases (including thrombosis, stroke, myocardial infarction, and arrhythmias in individuals under 50 years of age), recurrent reproductive failure, smoking history, and body mass index. In addition, relevant gynecological-obstetric data were documented, such as age at menarche, regularity of menstrual cycles, number of abortions, fetal deaths, artificial inseminations, ovarian stimulation cycles, embryo transfers of own oocytes, and ovodonations.
At the analytical level, data were collected according to the protocols established in the consultation, including antinuclear antibodies (ANAs), anti-peroxidase antibodies (TPO), anti-thyroglobulin (TG), anti-tissue transglutaminase IgA (tTgA), antiphospholipid antibodies (at least one determination of anti-cardiolipin IgM and IgG, anti-B2glycoprotein IgM and IgG and lupus anticoagulant), activated partial thromboplastin time, D-dimer, fibrinogen, Homeostatic Model Assessment (HOMA) index, thyrotropin (TSH), vitamin B9, B12 and D, homocysteine, complement C3 and C4, monocytes and cytotoxic natural killer cells in peripheral blood (CD3-CD16+ CD56+), Human Leucocyte Antigen (HLA) typing for susceptibility to celiac disease (DQ2.2, DQ2.5, DQ8 and DQ7.5), HLA-C and Killer immunoglobulin-like receptor (KIR). KIR-HLA-C incongruence was established when the patient had a KIR AA or centromeric AA, and either parent had HLA-C2 [25]. The extraction of these data was performed manually.
Patients were classified by reproductive diagnosis into the following groups: recurrent miscarriages, recurrent implantation failure, infertility, and history of fetal death.
The diagnosis of recurrent miscarriage was made according to the criteria of the European Society of Human Reproduction and Embryology (ESHRE) [26], as the loss of two or more pregnancies, including non-visualized pregnancy losses. The diagnosis of recurrent implantation failure was defined as those patients who had received at least two failed transfers of good-quality embryos. The diagnosis of fetal death was established as of week 10 [27]. The inability to achieve natural gestation for at least 12 months was considered infertility. Finally, a so-called preventive group was included. This group included patients with a previous diagnosis of autoimmune diseases or previous severe obstetric alterations of probable immunologic origin.
Subsequently, data were collected regarding the gestational loss prophylaxis regimen indicated for each patient. At this stage, the success or failure of this intervention was evaluated, understood as the achievement of pregnancy and the birth of a healthy newborn (APGAR test greater than 7).
In cases where the initial treatment was unsuccessful, we assessed whether they received a second line of treatment and its success rate.
During pregnancy, incidences of preeclampsia, intrauterine growth retardation, and preterm delivery (less than 37 weeks of pregnancy) were also recorded.
This study was conducted following the Declaration of Helsinki. The Clinical Research Ethics Committee of the Hospital Clínico San Carlos approved the study protocol (FIS Project PI19/01450). All patients signed informed consent at the consultation to participate in the project, which includes data analysis for retrospective studies.
Laboratory material
The analytical studies of the patients were performed as routine samples. The tests included activated partial thromboplastin time, D-dimer, fibrinogen, HOMA index (fasting glucose per insulin / 405), TSH, vitamin B12, and 25(OH)D, homocysteine, and monocytes. All of them were performed in the clinical analysis laboratory. The determination of lupus anticoagulant was performed in the hematology laboratory.
Anti-peroxidase, anti-thyroglobulin, and anti-tissue transglutaminase IgA antibodies were determined by enzyme-linked immunoassay (Enzyme-Linked Immuno Sorbent Assay, ELISA; AESKU.GROUP, Wendelsheim, Germany). Antinuclear antibodies were performed by indirect immunofluorescence (IFI, AESKU.GROUP, Wendelsheim, Germany), and antiphospholipid antibodies by Luminex (Bio-rad laboratories, Hercules [CA], USA) or chemiluminescence (Werfen, Barcelona, Spain).
The cellular study of cytotoxic natural killer cells was performed by multiparametric flow cytometry (Becton-Dickinson, San Jose, CA, USA), with the MultiTEST™ CD3 fluorescein isothiocyanate (FITC)/CD16+CD56 phycoerythrin (PE)/CD45 peridininin chlorophyll protein (PerCP)/CD19 allophycocyanin (APC). For the HLA study, DNA was extracted from peripheral blood leukocytes using MagNa Pure Compact Nucleic Acid Isolation KIT (Roche®, Darmstadt, Germany). Subsequently, the samples were genotyped for HLA-C, HLA-DR, HLA-DQA, HLA-DQB, and KIR by PCR-SSOP (ThermoFisher, Waltham, USA).
All techniques were performed according to the manufacturer’s instructions.
Statistical analysis
Quantitative data are expressed as mean and standard deviation unless otherwise indicated. Qualitative data are expressed as percentages. Although the study is mainly descriptive, we proceeded to incorporate a cross-sectional analytical analysis to compare the prevalences of immunological alterations between the two major subgroups (repeat miscarriages and recurrent implantation failure). The aim was to identify differences in the prevalence of the variables studied without attempting to establish causal relationships. This study was carried out using the Chi-square test. The results were considered statistically significant for p < 0.05. Only the first and last authors had access to the database.
Results
The total number of patients included in the study was 277, with a mean age of 38 years (±3.6) and a range of 22 to 50 years.
The reason for consultation was recurrent miscarriages (n = 178), recurrent implantation failure (n = 70), history of fetal death (n = 7), infertility (n = 9) and preventive group (n = 13).
Within the repeat miscarriage group, the mean number of miscarriages prior to our consultation was 2.7 (±1.3), range 2 to 14. The mean number of transfers performed in the recurrent implantation failure group was 2.82 (±2.4), with a range of 2 to 14. A total of 8 patients in this group (11.4%) resorted to ovodonation, with a mean of 2.88 (±1.9), ranging from 1 to 7 (Table 1).
Among the patients in the preventive group, five had a previous diagnosis of antiphospholipid syndrome, one patient had a history of preeclampsia, three patients had autoimmune thrombocytopenia and the remaining four had a previous diagnosis of autoimmune disease (three with multiple sclerosis and one with psoriatic arthritis).
From the data collected in the initial anamnesis of the entire population, active smoking was found in 10.1% of the patients, with 14.4% being additional ex-smokers. The most prevalent medical history was hypothyroidism, observed in 83 patients (29.9%). A total of 70 patients had a previous diagnosis of autoimmunity (25.7%).
In reference to family history, 41 patients had first- or second-degree relatives with a diagnosis of recurrent reproductive failure (14.8%). A total of 74 patients (26.7%) had a family history of autoimmune disease. In addition, 84 patients (30.3%) had a family history of severe cardiovascular disease (thrombosis, stroke or acute myocardial infarction) under the age of 50 years.
The body mass index was outside the optimal range (18 to 25) in 31.4% of the cases, with values below 18 in 3.4%, between 25 and 30 in 21.1%, and over 30 in 6.8% of the patients.
The baseline immunological study revealed the following global alterations (Table 2).
A total of 88.8% of the patients referred for recurrent reproductive failure presented at least one alteration of immunologic/vascular origin. This figure increases to 96.0% if we include genetic susceptibility to celiac disease.
Vascular disorders as a whole (elevated homocysteine, D-dimer and/or fibrinogen) affected 28.7% of the population, with elevated fibrinogen being the most prevalent (27.1%).
Both hypocomplementemia and elevated levels are included as complement alterations. At the C3 level, elevated complement was the most frequently observed (87% elevated versus 13% decreased). At the C4 level, although increased levels were also the most prevalent alteration, the proportion was not as striking (63% versus 37%).
A total of six cases in which no alteration was detected tested positive for antiphospholipid antibodies during gestation.
The distribution of analytical alterations found by group is detailed in Table 3.
A statistical analysis was performed using the Chi-square test (altered versus not altered) between the laboratory variables analyzed in the majority groups (recurrent miscarriages and recurrent implantation failure). The analysis revealed statistically significant differences in the levels of antinuclear antibodies (15.4% versus 42.5%; p = 0.03) and vitamin D deficiency (60.0% versus 37.2%; p = 0.01), as shown in Figure 1. A non-statistically significant trend was also observed at the level of fibrinogen (23.7% versus 39.0% p = 0.07). These data can be seen in online supplementary table 1.
Main differential findings between the recurrent miscarriage and recurrent implantation failure groups.
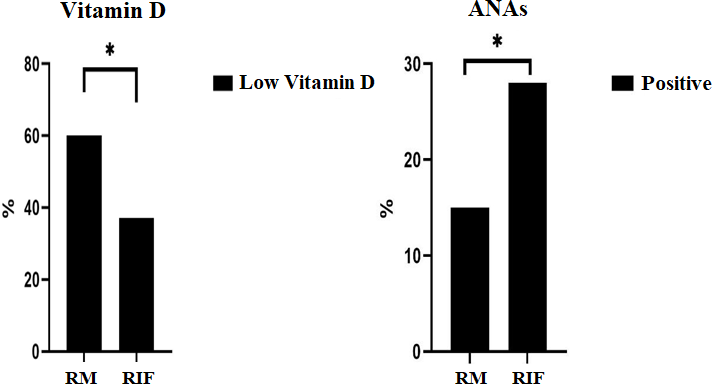
RM: recurrent miscarriages.
RIF: recurrent implantation failure.
Source: Prepared by the authors based on the results of the study.
For the prevention of gestational loss in these patients, the following drugs were used in prophylactic doses: acetylsalicylic acid, low-molecular-weight heparin, hydroxychloroquine, prednisone, lipid emulsion therapy, and intravenous gamma globulins. Levothyroxine was given depending on the alterations detected in the study and the patient’s clinical history.
The combination of acetylsalicylic acid plus low molecular weight heparin was the most frequently used, indicated in 31.8% of the patients. In second place, the combination of acetylsalicylic acid plus low molecular weight heparin plus hydroxychloroquine was used in 25.7% of cases. The combination of acetylsalicylic acid plus low molecular weight heparin plus prednisone was applied in 14.3% of cases. Finally, the combination of these four drugs (acetylsalicylic acid, low-molecular-weight heparin, hydroxychloroquine, and prednisone) was administered in 13.5% of cases.
Lipid emulsion therapy and intravenous gamma globulin therapy were used in 2.6% of cases, respectively. They were associated to a greater extent with the four drugs already mentioned.
All patients received vitamin supplements necessary for pregnancy, including vitamin D. Those with levels below 30 ng/mL received an additional supplement of 2,200 international units per day.
The gestational success rate, defined as a full-term pregnancy (greater than 37 weeks) with the birth of a live, healthy newborn in the first line of treatment, was 85.9% (240 live newborns). Of the 37 unsuccessful cases in that first line of treatment, 22 resorted to a second line of treatment, with a success rate of 68.1% (15 live newborns). The overall success rate, including both lines, was 97.3%.
Regarding the complications of these 255 pregnancies, 17 patients had a retrochorial hematoma in the first trimester. Three pregnancies had intrauterine growth retardation type 1 (two on treatment with acetylsalicylic acid plus low molecular weight heparin and one case with acetylsalicylic acid plus low molecular weight heparin plus hydroxychloroquine plus prednisone plus intravenous gamma globulins).
Two cases of preeclampsia were diagnosed (one patient received only low molecular weight heparin and the other acetylsalicylic acid plus low molecular weight heparin plus hydroxychloroquine). There were seven cases of prematurity, none before 32 weeks. During the puerperium, two patients presented with arthritis, while no other alterations were observed in the remaining patients.
At the neonatal level, some complications were observed. There was one case that required resuscitation due to APGAR less than 7 with good response and no subsequent objectifiable sequelae, one case of neonatal jaundice that was resolved with phototherapy, one case of heart murmur, and one neonatal admission due to dehydration.
Discussion
Our results show that 88% of the population with recurrent reproductive failure presented immunologic and/or vascular alterations, which reinforces the hypothesis of an immunologic component in this pathology. Expansion of cytotoxic natural killer cells was the most significant alteration, affecting 49.5% of patients, followed by maternal-fetal HLA-C-KIR incongruence (39.1%) and the presence of antiphospholipid antibodies (38.5%). All these factors have been previously related to implantation failure and recurrent gestational loss. A notable finding was the high prevalence of HLA alleles associated with celiac disease, detected in 78.6% of the patients, a figure notably higher than in the general population. This suggests a possible link between genetic susceptibility to autoimmunity and reproductive failure. This aspect deserves further exploration in future studies.
In terms of therapeutic response, a success rate of over 95% was observed when considering both first-line and second-line immune therapy. This data suggests a high degree of efficacy of the immunomodulatory strategies used. However, it is necessary to contextualize these results within the study’s limitations and to consider individual factors that may influence the response to treatment.
An increasing number of couples face reproductive problems, which may be caused by or associated with a variety of factors [28]. The exact prevalence of each of these factors is not fully elucidated since they may occur together. Some authors estimate that in up to 75% of cases, the cause is unknown [21], which makes it crucial to continue research to clarify these cases better and offer more targeted and effective treatments. In our patients, a high prevalence of immunological alterations is observed, in agreement with previous studies [1,16,24,29,30] that have described similar findings concerning obstetric pathologies. It is essential to note that the Gynecology and Obstetrics Service primarily referred patients. This, after ruling out other non-immunologic causes, which allows for initial screening.
In this study, we observed that almost half of the patients studied had elevated levels of cytotoxic natural killer cells in peripheral blood. This finding is consistent with previous studies that have linked the expansion of these cells to recurrent reproductive failure [9,13]. Killer lymphocytes represent the main maternal lymphoid component at the uterine level (about 70% during embryonic implantation) [31]. These cells perform important functions during the early stages of pregnancy, such as remodeling of the uterine spiral arteries and the secretion of molecules like angiopoietin 1 and 2, as well as vascular growth factors. All of these are essential for proper placentation and embryonic growth [32,33]. The expansion of these cytotoxic natural killer cells, both at the endometrial level and in peripheral blood, has been associated with recurrent reproductive failure and other obstetric syndromes [13,34].
On the other hand, uterine natural killer cells, through their stimulatory and inhibitory KIR receptors, interact directly with the embryonic trophoblast, which expresses the HLA-C molecule. Various combinations of the KIR receptor (molecularly classified as KIR AA or centromeric KIR AA), have also been described as an obstetric risk factor when interacting with an embryonic HLA-C2, which inhibits the proper activation and function of uterine natural killer cells [11,29]. Our findings reinforce the hypothesis that a mismatch in the interaction between maternal KIR receptors and embryonic HLA-C2 could play a key role in the pathophysiology of recurrent reproductive failure. The high prevalence of this mismatch in our sample suggests that the unfavorable KIR-HLA-C2 combination could interfere with maternal-fetal immune tolerance mechanisms. This would affect implantation and early embryonic development.
It is particularly striking that the presence of antiphospholipid antibodies considered the immunologic biomarker with the highest degree of evidence in the etiology of recurrent miscarriage, ranks third in prevalence within our sample. Although the involvement of antiphospholipid antibodies in recurrent gestational loss is well documented, their association with recurrent implantation failure and fetal death has also been reported in the literature [35,36,37].
The vascular component is also crucial for the correct development of pregnancy. About 30% of patients had elevated fibrinogen, homocysteine and/or D-dimer; known markers of cardiovascular risk, which have also been correlated with inflammation [36,38,39,40]. Other markers of inflammation, such as monocytes or elevated complement, were also detected. Excessive inflammation during pregnancy can have a deleterious effect and has been associated with implantation failure or miscarriage, preterm delivery, preeclampsia or neuropsychiatric disturbances in the newborn [2,15,41].
Vitamin D deficiency was detected in a significantly high percentage, especially in those patients with repeated miscarriages. It plays an immunomodulatory role, and its deficiency has been associated with alterations in the immune response, such as autoimmunity, inflammation, and vascular alterations [42]. In our study, this deficiency could be linked to some of the observed immune alterations. However, further studies are needed to confirm this association.
The comparative analysis performed between the recurrent miscarriage and recurrent implantation failure groups did not show statistically significant differences in most biomarkers. The exception was the presence of antinuclear antibodies and vitamin D deficiency, previously described in association with repeat abortions and recurrent implantation failure. Although both pathologies are distinct, they likely share alterations, as previously mentioned, since inflammation is detrimental in several phases of this process.
Regarding treatment, most patients received acetylsalicylic acid and low-molecular-weight heparin at prophylactic doses. Acetylsalicylic acid is a non-steroidal anti-inflammatory drug, with the capacity to inhibit thromboxanes, which gives it a useful antiplatelet capacity in prothrombotic states. Additionally, even at low doses, it exhibits an anti-inflammatory effect [43]. Low molecular weight heparin, in addition to its anticoagulant effect, also has some immunomodulatory capacity [44,45], which could justify its usefulness in cases not only of vascular but also immunological involvement.
Such therapy was mainly used in patients with a diagnosis of antiphospholipid syndrome or in those with a prothrombotic hemostatic disorder.
If such therapy was unsuccessful or if patients had other inflammatory or autoimmune disorders (except autoimmune hypothyroidism), hydroxychloroquine or prednisone was added at the practitioner’s discretion and according to the international consensus protocol for obstetric antiphospholipid syndrome [46].
The use of other drugs, such as lipid emulsion therapy or intravenous gamma globulins, was used in selected specific cases in which no response to conventional therapy had been obtained. These therapies were used with a high success rate, with more than 95% of cases classified as first- or second-line treatments and an excellent safety profile.
It should be noted that the prematurity rate was 2.7%, four points lower compared to the Spanish prevalence (6.7%) [47]. Similarly, the rate of preeclampsia was also found to be decreased, with only two cases (0.78% versus 2 to 10%) [48], as well as intrauterine growth retardation, in three patients (1.1% versus 10 to 15%) [49].
The results of this study have important clinical implications, both in the diagnosis and management of these patients. The high prevalence of immunologic alterations observed in our patients suggests their involvement in the pathophysiology of these pathologies. This reinforces the need to incorporate them systematically in the evaluation of these patients, especially when other known causes have been ruled out. Early identification of immunological alterations would enable more accurate risk stratification and the implementation of targeted therapeutic strategies, thereby optimizing reproductive outcomes. Our results support the effectiveness of the immunomodulatory treatments used, suggesting a more proactive approach in the detection and management of these disorders. This could significantly improve success rates in this group of patients. They also emphasize the importance of continuing to investigate the impact of various immunological profiles on reproduction, aiming to develop a more personalized and evidence-based approach to treating recurrent reproductive failure.
The study has several limitations that should be taken into account when interpreting the results. Because the patients included were referred by professionals external to the unit, these results may depend on the clinical indications and referral criteria of these professionals. This could introduce a selection bias by not representing the entire population with reproductive problems. Furthermore, the generalizability of the results is limited by the study’s nature, as it was conducted in a single, highly specialized center. Although the results are relevant to this particular unit, extrapolation of these results to other populations should be made with caution. Factors such as differences in patient referral, variability in immunologic assessment protocols, and genetic and environmental diversity could influence the prevalences observed in other clinical settings. Therefore, it will be essential to conduct multicenter studies with a larger design to corroborate these findings in different populations and clinical settings. This would contribute to greater external validity of the results. It would also allow the relevance of the immunological alterations identified in recurrent reproductive failure to be established with greater precision.
Conclusions
In this study, we observed a significant prevalence of immunological alterations in patients with recurrent reproductive failure, suggesting that alterations in the immune system may play a crucial role in its etiology. These results underscore the need for further investigation into the relationship between the immune system and obstetric complications in order to develop more personalized and evidence-based clinical approaches.
In addition, patients with immunological alterations who received immunomodulatory treatment experienced a high rate of gestational success with a favorable safety profile. These results support the need for further studies to optimize therapeutic strategies and define selection criteria for patients who may benefit from this approach.

