Estudios originales
← vista completaPublicado el 16 de abril de 2025 | http://doi.org/10.5867/medwave.2025.03.3042
Distribución sociodemográfica y espaciotemporal de la coinfección tuberculosis y virus de la inmunodeficiencia humana en tres cantones de Guayas, Ecuador: un estudio transversal.
Sociodemographic and spatiotemporal distribution of tuberculosis and human immunodeficiency virus co-infection in three cantons of Guayas, Ecuador: A cross-sectional study.
Abstract
Introduction Tuberculosis (TB) and human immunodeficiency virus (HIV) co-infection are major public health problems in Latin America and Africa. The province of Guayas in Ecuador has a high proportion of cases but there is limited information on their sociodemographic characteristics and spatial distribution. The aim of this study was to analyze the sociodemographic and spatiotemporal characteristics of TB/HIV coinfection patients in three cantons of the Guayas province, Ecuador, in 2018.
Methods A cross-sectional study was conducted using secondary data from the Ministry of Public Health of Ecuador. The study population was all adult patients with a diagnosis of TB/HIV co-infection residing in the three cantons of the three cantons. Data were analyzed to determine prevalence, incidence and mortality, as well as socio-demographic variables such as age, sex, educational level and housing conditions. Spatial distribution was assessed using QGIS software version 3.24 to identify high-prevalence areas.
Results A total of 379 cases of TB/HIV coinfection were identified, with a predominance of males (80.74%) and a mean age of 35 years. The prevalence was 1.24 per 100 000 inhabitants, with a case fatality rate of 15.57%. Individuals below the poverty line showed a stronger association with co-infection (PR=6.773, 95% CI: 4.985 to 9.202). Spatially, cases were concentrated in socioeconomically disadvantaged municipalities of Guayaquil.
Conclusions TB/HIV co-infection shows a clear association with social determinants, especially poverty and educational level. The heterogeneous spatial distribution among the three cantons and the high case fatality rate suggests the need to strengthen epidemiological surveillance and implement targeted interventions addressing social determinants in the most vulnerable areas.
Main messages
- TB/HIV coinfection represents a significant public health challenge in Ecuador, particularly in Guayas province, where limited information exists about its sociodemographic and spatial distribution patterns.
- This is the first comprehensive analysis of TB/HIV coinfection’s spatial distribution and social determinants in three major cantons of Guayas, providing evidence for targeted interventions in high-burden areas.
- The use of secondary data sources limited the validation of cases across different information systems and prevented the establishment of causal relationships due to the ecological study design.
- TB/HIV coinfection showed strong association with poverty (PR=6.773, 95% CI: 4.985-9.202) and concentrated in socioeconomically disadvantaged areas, with a prevalence of 1.24 per 100,000 inhabitants and a case fatality rate of 15.57%.
Introduction
Tuberculosis (TB) and human immunodeficiency virus (HIV) co-infection is a major public health problem worldwide [1]. Since the emergence of HIV in the 1980s, a synergistic interaction between the two diseases has been observed, whereby TB accelerates the progression of HIV infection to acquired immunodeficiency syndrome, while HIV weakens the immune system and facilitates the development of active TB [2,3]. This phenomenon is particularly prevalent in low- and middle-income countries, including regions of Africa and South America, where TB and HIV place a significant burden on health systems [4].
In 2020, the World Health Organization (WHO) estimates that there will be 29 000 cases of TB/HIV coinfection in the Americas, with an incidence rate of 2.9 per 100 000 population and 7830 deaths from TB in people living with HIV [5,6]. In Ecuador, the estimated incidence was 6.1 per 100 000 population [5]. Nationally, the province of Guayas, including the cantons of Guayaquil, Durán and Samborondón, accounts for approximately 50% of reported TB and HIV cases [7,8,9], making it a priority region for epidemiological intervention and analysis.
Sociodemographic and spatiotemporal analysis of TB/HIV coinfection allows the identification of geographical distribution patterns and associated risk factors that may contribute to the spread of these diseases [10]. Social determinants of health, such as poverty, education level and housing conditions, are critical factors that may influence the incidence and prevalence of co-infection [9,11,12,13].
In this context, the present study aimed to analyze the spatiotemporal characteristics of TB/HIV coinfection and socio-demographic factors in three cantons of the province of Guayas, Ecuador, in 2018.
Methods
Study design
A descriptive cross-sectional study of TB/HIV co-infection was conducted using secondary databases from the Ministry of Public Health of Ecuador. Data of clinical diagnoses and treatment were collected to include all patients diagnosed with TB/HIV coinfection in the cantons of Guayaquil, Durán and Samborondón in the province of Guayas, Ecuador, in 2018. The Automated Daily Record of Consultations and Ambulatory Care, the Automated Health Care Registry Platform provided patient follow-up information, the Needs Estimation Information System provided socioeconomic indicators, and SINFO-TB database provided primary source providing nominal TB/HIV coinfection case data. In addition, data on poverty and education levels were obtained from the 2010 census conducted by the National Institute of Statistics and Census of Ecuador (INEC) [14], and data on household overcrowding were extracted from the 2014 INEC Living Conditions Survey [15].
Eligibility criteria
The study included all confirmed cases of TB/HIV coinfection recorded in the databases in 2018, including patients of all ages, sexes and socioeconomic levels who were diagnosed with both TB and HIV. Cases without a laboratory-confirmed diagnosis of TB or HIV were excluded, as were duplicate cases or those with incomplete data in the databases used.
Variables and spatial analysis
Variables included age, sex, level of education, socioeconomic status, and household overcrowding. The level of education was categorized as basic education (0 to 10 years of schooling), high school (11 to 13 years), and tertiary education (>13 years), which includes university and other post-secondary education. Socioeconomic status was defined using the national poverty line, with households earning below US$84.72 per capita per month considered to be living in poverty. Household overcrowding was defined as having more than three persons per bedroom, following the criteria established by the INEC.
To geographically locate cases of co-infection, patients were geo-referenced at the parish level within the cantons of Guayaquil, Durán, and Samborondón in the province of Guayas, Ecuador.
Data analysis
Prevalence ratios were calculated using 2x2 contingency tables, comparing exposed vs unexposed groups for each sociodemographic factor. The 95% confidence intervals were computed using the log-binomial method in R version 4.2, with statistical significance assessed by Chi-square test (p<0.05). Population denominators came from 2010 census data and 2018 INEC projections. In addition, heat maps were generated to identify areas of high case concentration using QGIS version 3.24 geographic information system software.
Results
In 2018, a total of 379 TB/HIV coinfection cases were identified in the cantons of Guayaquil, Durán, and Samborondón in Guayas for this combined area with a total population of 3 067 272 inhabitants, the coinfection prevalence was 1.24 per 100 000 inhabitants, and the incidence of new cases was 1.11 per 100 000 inhabitants. The mortality rate associated with coinfection was 0.02 per 100 000 inhabitants, with a case fatality rate of 15.57%.
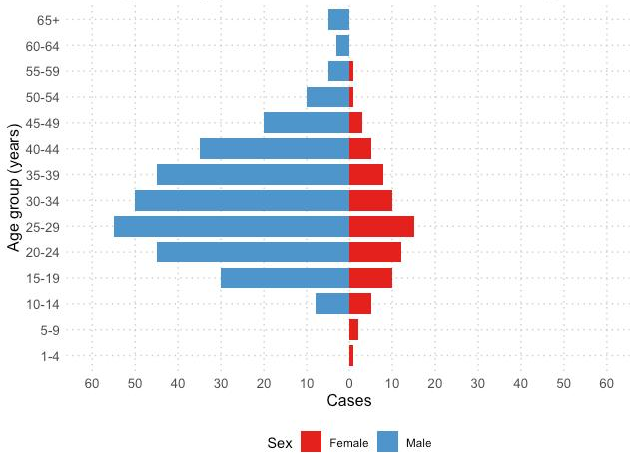
Regarding the sociodemographic analysis, 80.74% of the total coinfection cases were men (N = 306). The average age of patients was 35 years (SD: 11.38 years, range 4 to 74 years), with cases concentrated mainly in individuals aged 25 to 44 years (Figure 1). Of the affected patients, 52.4% lived below the poverty line, and those with only basic education represented 53.7% of the cases.
Population pyramid of TB/HIV co-infection cases by sex.
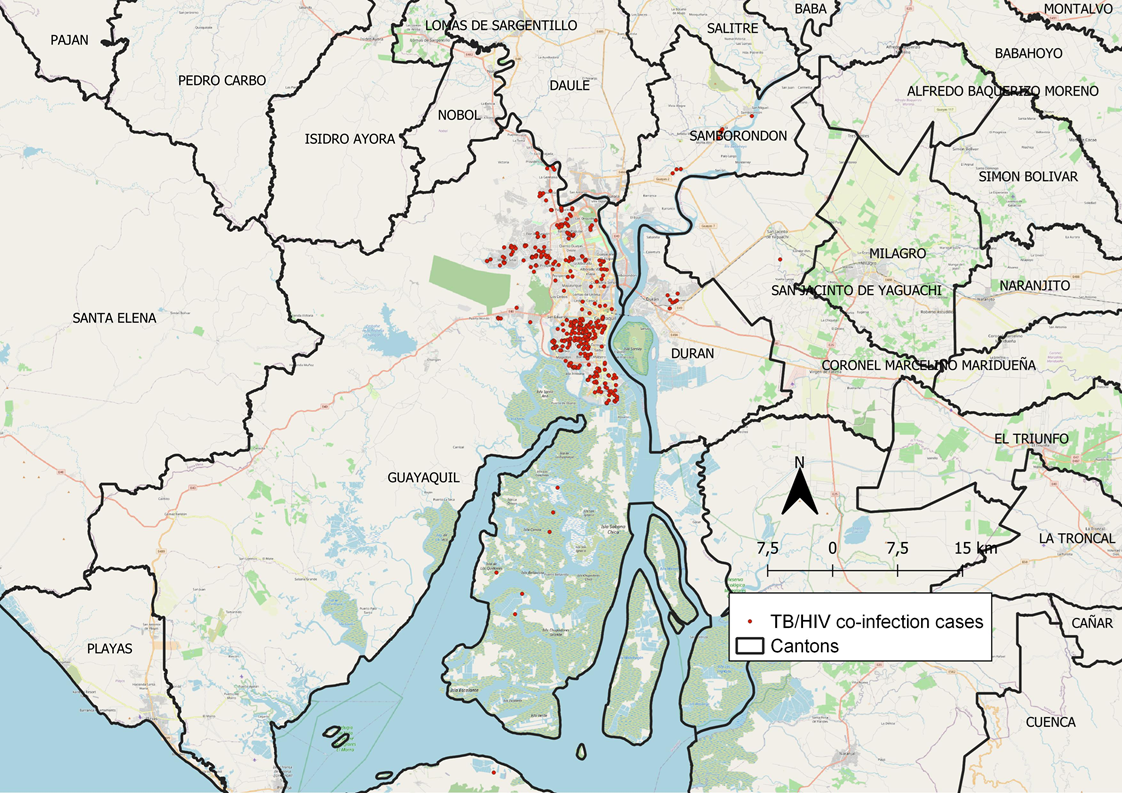
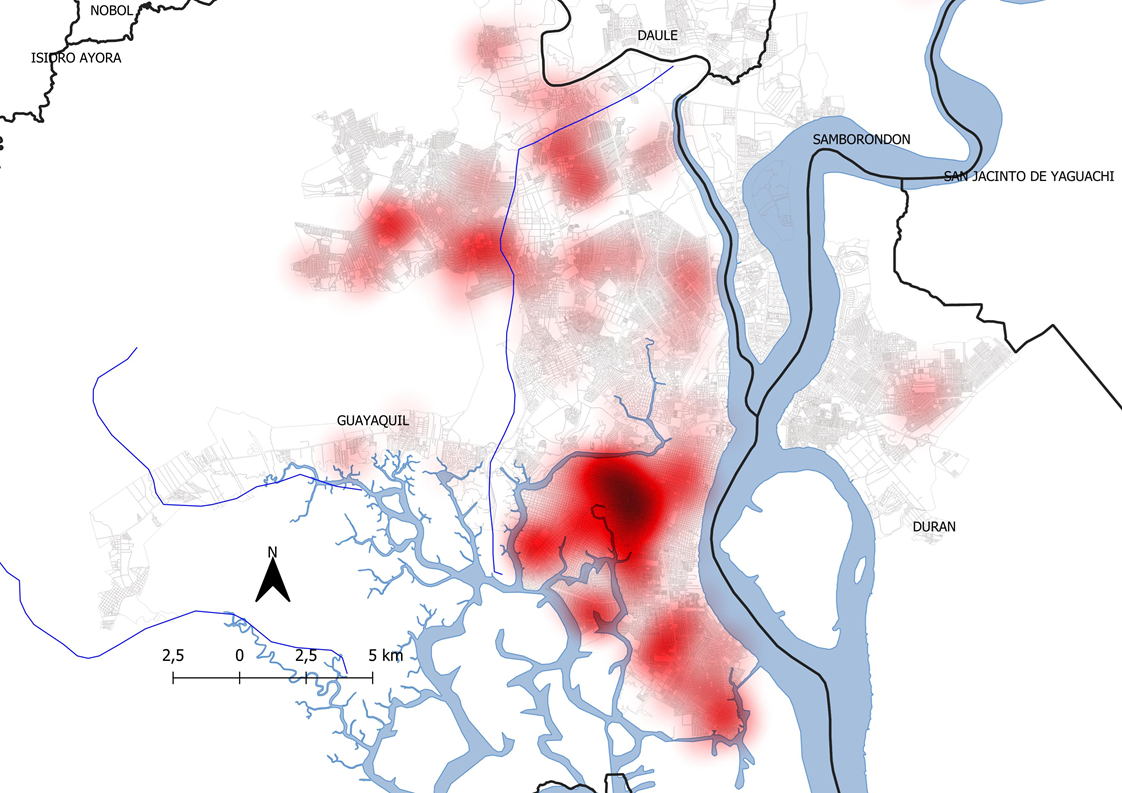
Geospatial analysis revealed an uneven distribution of cases across the three cantons (Figure 2). The distribution of cases reflected significant demographic and socioeconomic differences between the three cantons. Guayaquil, the largest canton with 2.67 million inhabitants and the main economic hub of the region, accounted for 354 cases (prevalence 1.32 per 100 000). In contrast, Durán and Samborondón, with populations of 300 488 and 94 983, respectively, each showed lower prevalence (0.63 per 100 000). Within Guayaquil, cases concentrated in socioeconomically disadvantaged urban parishes like Pascuales, Tarqui, Febres Cordero and Ximena, characterized by higher poverty rates and population density (Figure 3).
Georeferencing of TB/HIV cases in 2018 in the cantons of Guayaquil, Durán, and Samborondón.
Heat map of TB/HIV cases in 2018 in the Canton of Guayaquil.
The prevalence ratio analysis revealed several significant associations. Individuals living below the national poverty line (
Discussion
The prevalence of TB/HIV coinfection in our study (1.24 per 100 000 inhabitants) differs from patterns observed in other Latin American countries. When analyzing the proportion of HIV among TB patients, studies have reported variations from 4.8% in Peru to 17% in Colombia [5,9,16]. Brazil, Chile, and Argentina have reported intermediate proportions of HIV among TB patients of 9.4%, 8.7%, and 13.5%, respectively [17,18,19,20]. However, these prevalences are significantly lower than those documented in high-burden regions such as sub-Saharan Africa, where prevalence reaches 31% [21]. These differences could be attributed to various factors, including disparities in surveillance systems and diagnostic criteria between countries, differences in cross-screening strategies for TB/HIV, and potential underreporting in our context.
The predominance among males and concentration in young adults with a mean age of 35 aligns with the regional epidemiological profile described by other authors [21,22]. This distribution may be explained by behavioral factors and differential exposure to risk, though it could also reflect barriers to diagnosis in women, as suggested by previous studies [23].
The identified association between poverty and TB/HIV coinfection underscores the importance of social determinants, consistent with previous findings in Colombia, where social vulnerability was significantly associated with poorer outcomes [24]. Additionally, the geographical concentration of cases in socioeconomically vulnerable areas of Guayaquil reinforces this association and aligns with patterns observed in other major Latin American cities [25]. The heterogeneous spatial distribution, with high-prevalence clusters in specific parishes, further suggests a need for targeted interventions. This pattern, similar to that observed in São Paulo by Campoy et al. [25], highlights the importance of considering the local context in intervention planning.
Regarding educational level, individuals with higher education showed a lower association with TB/HIV coinfection prevalence. This finding supports the conclusion that education influences health knowledge, risk behaviors, and access to services [26]. Concerning overcrowding, our findings showed an apparent negative association, which contrasts with the existing literature. This paradoxical result likely reflects data quality limitations and information biases rather than a true negative association. Previous studies, such as those by Pelissari et al. and Silva et al., have consistently demonstrated that overcrowding increases the risk of TB transmission [27,28], amplifying TB risk 3.7-fold, an effect that is intensified in the presence of HIV [28].
This study has several limitations, including the use of secondary data with incomplete records for some socio-demographic variables and the inability to validate cases across different information systems. In addition, as an ecological study, it cannot establish causal relationships.
On the other hand, this study has several strengths with significant public health implications. First, our findings demonstrate that TB/HIV coinfection disproportionately affects socioeconomically vulnerable populations, suggesting that control strategies must explicitly address social determinants. Specifically, the strong association with poverty (PR=6.773) and education level indicates the need for integrated interventions that combine clinical management with social support programs.
Second, the spatial analysis revealed clear geographic patterns of disease concentration in specific urban areas, particularly in marginalized parishes of Guayaquil. This spatial clustering, with prevalence rates reaching 4.93 per 100 000 in areas like Pascuales, indicates the need for targeted interventions and strengthened healthcare capacity in these high-burden zones. The identification of these hotspots provides an evidence base for resource allocation and intervention planning.
Third, the observed case fatality rate of 15.57% highlights critical opportunities for improving patient outcomes. This relatively high mortality suggests gaps in early detection and integrated care pathways that need addressing through enhanced screening programs and better coordination between TB and HIV services.
However, several research gaps remain. Longitudinal studies are needed to evaluate the effectiveness of socially-focused interventions and to better understand healthcare access barriers in affected communities. Future research should also examine how social support programs could complement existing clinical interventions to improve treatment adherence and outcomes .
Conclusions
TB/HIV coinfection in the studied cantons of Guayas shows clear socioeconomic and spatial patterns. The prevalence of 1.24 per 100 000 inhabitants, with significant concentration in socioeconomically disadvantaged areas, highlights the role of social determinants in disease distribution. The strong association with poverty (PR=6.773) and lower educational levels emphasizes the need for integrated interventions that address both clinical and social aspects. The spatial analysis revealed hotspots in specific urban parishes of Guayaquil, providing evidence for targeted interventions. The relatively high case fatality rate (15.57%) suggests opportunities for improving early detection and treatment outcomes. These findings support the need for strengthened surveillance systems and territorially-focused interventions that consider social determinants, particularly in vulnerable areas. Future public health strategies should integrate social support programs with clinical interventions to effectively address this dual epidemic.

