Estudios originales
← vista completaPublicado el 5 de mayo de 2025 | http://doi.org/10.5867/medwave.2025.04.3045
Influencia de las diferentes modalidades de tratamiento en la función sexual de supervivientes de cáncer de mama: estudio observacional ambispectivo
Influence of different treatment modalities on the sexual function of breast cancer survivors: An observational ambispective study
Abstract
Introduction Advances in treatment have improved the survival rates of patients diagnosed with breast cancer. However, the number of women experiencing long-term consequences has also increased, affecting their quality of life, including sexual function.
Objectives To evaluate the prevalence of sexual dysfunction as measured by the Female Sexual Function Index, its association with treatment modalities in Uruguayan breast cancer survivors, and to compare the questionnaire scores by age group (50 years or older versus under 50 years).
Methods This ambispective observational study included patients diagnosed with early-stage breast cancer (I to III) who had completed surgery, chemotherapy, and radiotherapy treatments at least 12 months before inclusion. Patients completed the Female Sexual Function Index questionnaire, and the data were analyzed using simple and multiple binary logistic models to assess the relationship between treatment modalities and sexual dysfunction. Additionally, differences in Female Sexual Function Index scores between age groups were analyzed.
Results A total of 149 patients were included; 67.1% underwent breast-conserving surgery, 68.5% received chemotherapy, 92.6% radiotherapy, and 95.3% hormone therapy. Sexual dysfunction, defined as a score ≤ 26.55 on the questionnaire, was present in 58.3% of patients. Multivariate analysis indicated a higher risk of sexual dysfunction in patients who underwent total mastectomy, were treated with chemotherapy, or used gonadotropin-releasing hormone agonists.
Conclusions Although this study highlights the impact of certain treatment modalities on sexual function, the results should be interpreted considering the characteristics of the population and potential biases. These findings can guide clinicians in planning treatments to improve the quality of life of sexually active breast cancer patients.
Main messages
- Sexual dysfunction is a common problem among breast cancer survivors, significantly affecting their quality of life.
- Given the lack of specific literature in the Uruguayan context, this study seeks to address the growing need to understand the impact of breast cancer treatments on women’s sex lives.
- As a prospective observational study that includes a comparison of various surgical modalities, as well as chemotherapy, radiotherapy, and hormone therapy, this work provides a comprehensive view of how each treatment affects sexual function.
- The findings of this study can guide clinicians in planning treatments and counselling sexually active patients, helping to improve their quality of life.
- Among other aspects, the applicability of the findings may be limited since the Female Sexual Function Index questionnaire used has not been validated specifically for the Uruguayan population; there may be reporting bias because the data on sexual dysfunction are based on self-reported responses; and we do not know if the comparisons that did not yield statistical significance were due to a lack of power of the test, as no prior calculation of sample size was performed.
Introduction
In 2022, breast cancer had a global incidence of 2 296 840 new cases and caused 666 103 deaths, being the second most common cancer in terms of incidence and the fourth in terms of mortality worldwide [1]. This disease not only represents a global challenge, but is also a prominent issue in Uruguay [2]. As treatment paradigms advance and survival rates improve, so does the number of women facing the long-term consequences of cancer treatments, directly impacting their quality of life during their survivorship. It has been reported that, following diagnosis and treatment for breast cancer, many survivors face sexual dysfunction [3,4,5]. This type of dysfunction poses challenges to psychosocial adaptation, especially considering the extensive recovery process, with possible repercussions on emotional health, body image perception, and self-confidence [6,7].
Breast cancer surgery can affect a patient’s sexual function. Recent studies indicate that women who opt for breast-conserving surgery do not experience significant differences in sexual function compared to women who do not undergo this surgery. However, those who undergo a mastectomy may face sexual problems after the operation [8,9,10,11]. Both interventions, conservative surgery and mastectomy, offer similar survival rates, allowing patients to decide which procedure they prefer [12,13]. There has been a notable increase in the number of unilateral and bilateral mastectomies to treat early-stage breast cancers in recent years [14].
Chemotherapy treatment includes the risk of ovarian failure and early menopause in premenopausal women, which can cause sexual dysfunction [3]. In addition, agents such as anthracyclines and taxanes can reduce physical function and sexual desire, along with fatigue, alopecia, gastrointestinal problems, and myelosuppression. Although many women improve after completing chemotherapy, some continue to experience persistent symptoms [15,16].
On the other hand, aromatase inhibitors have been reported to cause difficulties in sexual function that are sometimes difficult to overcome [15].
Although hormone therapy is crucial in the treatment, it can negatively affect the patients' sexual health. Between 30 and 40% of women treated with tamoxifen and more than 50% of those treated with aromatase inhibitors experience sexual dysfunction [17,18]. Both treatments can aggravate menopausal symptoms, increasing the frequency and severity of hot flashes. Aromatase inhibitors are associated with an increased risk of dyspareunia, while tamoxifen reduces sexual interest. These adverse effects are more common among younger patients, demonstrating that, despite their different profiles, both treatments can harm female sexual health [19,20].
Given the growing need to understand the impact of breast cancer treatments on women’s sex lives and considering the limited specific literature in the Uruguayan context, this research aims to evaluate the prevalence of sexual dysfunction in breast cancer survivors, its association with treatment modalities and differences between age groups (50 years or older versus . under 50 years). The hypothesis is that patients treated with chemotherapy and hormone therapy will have a higher prevalence of sexual dysfunction compared to those treated with surgery alone. Similarly, patients who have undergone a total mastectomy will experience more sexual dysfunction than those who have undergone breast-conserving surgery.
Methods
Study design and population
Ambispective observational study conducted between March and September 2024. It included patients over the age of 18 diagnosed with early-stage breast cancer (I to III) who had completed treatment with surgery, chemotherapy, and radiotherapy at least 12 months before inclusion and who had not relapsed. The population of interest consisted of patients treated at two referral centres: the Hospital de Clínicas and the Hospital Departamental de Soriano.
Inclusion and exclusion criteria
Inclusion criteria:
-
Confirmed diagnosis of stage I to III breast cancer.
-
Having completed primary treatments at least 12 months before evaluation.
-
Being sexually active in the last four weeks.
-
Consenting to participation by signing an informed consent form.
Exclusion criteria:
-
Patients who relapsed during the study period.
-
Those with a history of other pathologies that could significantly interfere with sexual function (for example, severe neurological or psychiatric disorders).
Sampling strategy: Consecutive sampling was used. All eligible patients were invited to participate during their follow-up consultations at the mentioned centres, aiming to minimise selection biases.
Description of the variables
Outcome variable
Sexual dysfunction was defined as a score of 26.55 or less on the Female Sexual Function Index questionnaire, indicating the presence of sexual dysfunction in the participant. This variable is the primary outcome of the study, enabling an assessment of the impact of treatment modalities on sexual function.
Predictor variables
The treatment modalities received were considered as exposure variables, as these are key factors that could influence the sexual function of the patients. These variables include:
-
Type of surgery (total mastectomy versus conservative surgery): The study investigates whether surgical intervention affects sexual function, given the potential impact of each type of surgery on body image and sexual health.
-
Use of chemotherapy: an exploration of whether chemotherapy treatments, by generating side effects, are associated with sexual dysfunction.
-
Use of radiotherapy: an examination of whether radiotherapy can be associated with sexual dysfunction.
-
Type of hormone therapy (tamoxifen, aromatase inhibitors, or gonadotropin-releasing hormone agonists): Hormone therapy is a fundamental treatment for breast cancer, but it has adverse effects. We evaluate whether these can impact sexual health.
Confounding variables
Confounding variables include age and stage of cancer. These variables were selected because they could be associated with both treatment modalities and sexual function.
The stage of the cancer was operationalised using the TNM (Tumour, Node, Metastases) classification for breast cancer, defined by the American Joint Committee on Cancer (AJCC) in the AJCC Cancer Staging Manual, 8th edition [21].
Procedures
The Female Sexual Function Index questionnaire is an internationally validated tool for evaluating female sexual function [22]. Furthermore, it has been specifically validated in women with breast cancer, demonstrating high acceptability, reliability, and validity in this population [23]. It measures six specific domains: desire, arousal, lubrication, orgasm, satisfaction, and pain, using 19 items. Each domain has an adjusted minimum and maximum score:
-
Desire: 1.2 to 6.0.
-
Arousal: 0 to 6.0.
-
Lubrication: 0 to 6.0.
-
Orgasm: 0 to 6.0.
-
Satisfaction: 0.8 to 6.0.
-
Pain: 0 to 6.0.
The total score is calculated by adding the scores for the domains, with a total range of 2 to 36. A score less than or equal to 26.55 indicates sexual dysfunction. The version used was adapted and validated for the Spanish-speaking population [24], but not specifically for the Uruguayan population.
The data on treatment modalities (surgery, chemotherapy, radiotherapy, and hormone therapy) were obtained retrospectively from medical records.
Statistical analysis
The analysis was conducted using R software (version 4.1.2). Qualitative variables were described using absolute frequencies and relative percentages. The Female Sexual Function Index score, designed initially as a semi-quantitative scale, was categorized using the validated cut-off point of equal to or less than 26.55 to indicate the presence of sexual dysfunction. This cut-off point allowed the participants to be classified into two groups: those with sexual dysfunction and those without sexual dysfunction. The sexual dysfunction variable, categorized into these two groups, was used as the primary outcome variable to assess the prevalence of sexual dysfunction in the study population.
The prevalence of sexual dysfunction was assessed with 95% confidence intervals. The relationship between the exposure variables (type of surgery, chemotherapy, radiotherapy, type of hormone therapy, and use of gonadotropin-releasing hormone agonists) and sexual dysfunction was analyzed using simple and multiple binary logistic models (odds ratio, 95% confidence interval). A p value < 0.05 was considered statistically significant.
Normality in the distribution of the scores for the dimensions of the Female Sexual Function Index questionnaire was evaluated using the Shapiro-Wilk test and graphically.
The differences in the scores on the Female Sexual Function Index questionnaire were compared according to the treatment modalities (mastectomy, conservative surgery, radiotherapy, chemotherapy, hormone therapy) and according to age, to evaluate how these variables could influence sexual dysfunction. The differences between the groups were assessed using the Mann-Whitney test.
No sensitivity analyses were performed in this study. No missing data were identified in the analyzed variables. No loss to follow-up was observed, as all patients included completed the questionnaire in its entirety.
This study was approved by the Research Ethics Committee of the Hospital de Clínicas Dr. Manuel Quintela on February 19, 2024, with approval number 163-23. All patients who participated signed an informed consent form before being included in the study.
Results
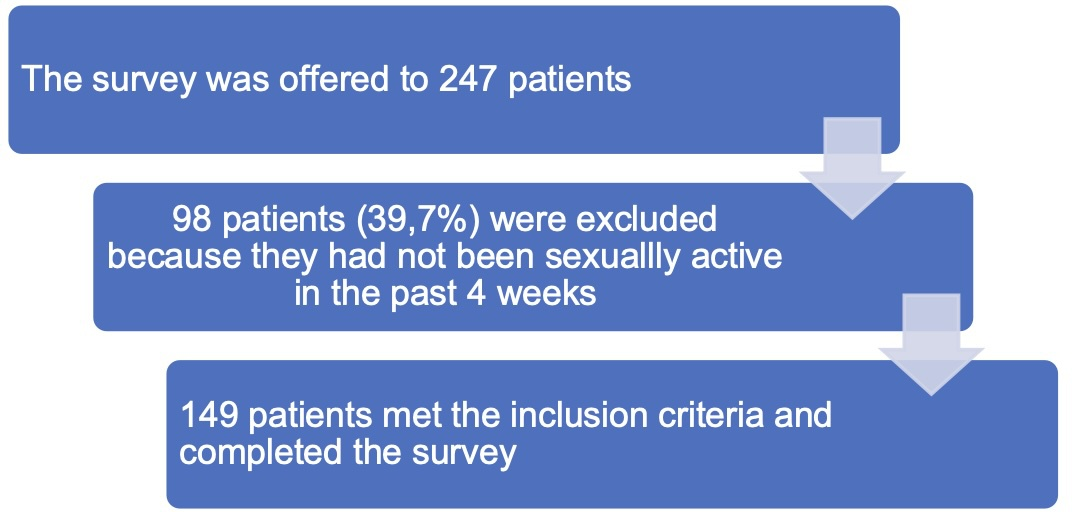
During the study period, the survey was offered to 247 initially eligible patients. Of these, 149 patients (60.3%) met the inclusion criteria and completed the survey. The remaining 98 patients (39.7%) were excluded because they did not meet the criterion of being sexually active in the last 4 weeks (Figure 1).
Flow chart.
The median age at the time of completing the survey was 58 years; the majority (108 patients, 72.5%) were over 50 years of age at the time of the survey. A large proportion of the patients included (112; 75.2%) had completed secondary education or tertiary education (Table 1).
In terms of stage, 54.4% (81 patients) were stage II. In terms of the treatments received, 67.1% (100) underwent conservative surgery, 31.5% (47) received chemotherapy, 89.9% (134) received adjuvant radiotherapy, and 92.6% (138) received adjuvant hormone therapy (Table 2).
The majority of patients treated with hormone therapy received tamoxifen as a single agent (45%; 67), 40.2% (60) with aromatase inhibitors as a single agent and the rest with gonadotropin-releasing hormone agonists (8 in combination with aromatase inhibitors and 7 with tamoxifen).
58.3% of the patients (74) presented sexual dysfunction (95% confidence interval; 49.2 to 66.8%) with a median score on the scale of 28.6 points in the group without dysfunction and 23.4 in the group with dysfunction. The domains of the survey that had the lowest scores were desire and arousal. (Table 3).
For patients aged 50 or younger, the median score was 30.1, while for those over 50, it was 24.7, indicating a significant difference (p < 0.001). Furthermore, patients over 50 years of age had significantly lower scores in all domains of the Female Sexual Function Index questionnaire compared to patients 50 years of age or younger (Table 4).
Patients who underwent a total mastectomy had three times higher odds of sexual dysfunction compared to those who underwent conservative surgery, this difference being statistically significant. In the adjusted analysis, patients who underwent a total mastectomy continued to show a significantly higher risk of sexual dysfunction compared to those who had a sectorial mastectomy. This confirms that this difference is significant and relevant (Table 5).
Table 5 Multivariate analysis of factors associated with sexual dysfunction among breast cancer survivors (n = 149).
In addition, it was observed that patients who underwent total mastectomy had significantly lower scores in all domains of the Female Sexual Function Index questionnaire compared to those who underwent conservative surgery (Table 6 ).
Patients treated with chemotherapy had a lower prevalence of sexual dysfunction in the crude analysis, a difference that persisted in the adjusted analysis (Table 5). On the other hand, radiotherapy treatment did not have a significant impact on the sexual function of breast cancer survivors.
In the crude analysis, sexual dysfunction was less frequent among patients treated with tamoxifen compared to those treated with aromatase inhibitors. This suggests that the risk of sexual dysfunction is lower for patients who received tamoxifen. However, this difference disappeared in the adjusted analysis, indicating that after adjusting for other variables, there was no significant difference between tamoxifen and aromatase inhibitors in terms of sexual dysfunction (Table 5).
The use of gonadotropin-releasing hormone agonists was associated with a significantly higher odds ratio for sexual dysfunction (odds ratio 5.6, 95% confidence interval 1.5 to 25.6). This indicates that patients using these agonists have more than five times the odds of experiencing sexual dysfunction compared to those who do not use them (Table 5). Furthermore, the use of agonists had a significant impact on the orgasm and pain domains (Table 7).
Table 7 FSFI scores of patients on treatment with gonadotropin-releasing hormone agonists versus those who do not receive it (n = 149).
Discussion
This study aimed to evaluate the prevalence of sexual dysfunction in breast cancer survivors and its association with the treatment modalities received, as well as to explore the differences in the Female Sexual Function Index questionnaire scores between age groups. The results showed that sexual dysfunction was significantly more prevalent in patients treated with total mastectomy compared to breast-conserving surgery, and in those who received hormone therapy with luteinizing hormone-releasing hormone agonists. In addition, patients over the age of 50 presented lower scores in all domains of the Female Sexual Function Index questionnaire compared to those under 50, highlighting the impact of menopause on sexual function. These findings underscore the importance of considering both treatment modalities and factors related to age and menopause in evaluating quality of life in this population.
Several studies show that the risk of developing sexual dysfunction is significantly higher among breast cancer survivors compared to the general population. One study found that breast cancer survivors are at a higher risk of developing sexual dysfunction compared to the general population (9.1% versus 6.9%) [3]. In this context, another study revealed that women diagnosed and treated for breast cancer were 3.9 times more likely to have sexual dysfunction compared to healthy women, with a prevalence of 74% in the exposed group compared to 39% in the unexposed group [25].
Sexual dysfunction includes alterations in sexual desire, arousal, orgasm, and satisfaction, which can lead to interpersonal difficulties and emotional distress. Systemic treatments for breast cancer such as chemotherapy and hormone therapy can induce menopause and reduce vaginal lubrication, which negatively impacts sexual arousal and desire. In addition, changes in body image resulting from different treatments can alter the perception of femininity and sexual identity, affecting sexual function [3,25].
Conclusions
Patients who underwent total mastectomy and were treated with gonadotropin-releasing hormone agonists or chemotherapy had an increased risk of sexual dysfunction. No significant associations were found with radiotherapy or with tamoxifen-based hormone therapy versus aromatase inhibitors.
Although these findings highlight the impact of certain treatment modalities on sexual function, they should be interpreted with caution due to possible biases related to the observational design of the study.
These results can guide clinicians in treatment planning and counseling of sexually active patients, promoting interventions that improve their quality of life.
This study evaluates the prevalence of sexual dysfunction in women diagnosed with breast cancer who had completed treatment with surgery, chemotherapy, and radiotherapy at least 12 months before inclusion. Two hundred and forty-seven patients were invited to participate; 39.7% of the invited patients (98) were not included because they were sexually inactive. This figure is consistent with other studies where 35% were sexually inactive [25,26].
58.3% of the patients (74) suffered from sexual dysfunction (confidence interval 49.2 to 66.8%) with a median score on the scale of 28.60 points. This figure is lower than that reported internationally by various studies that also used the Female Sexual Function Index questionnaire, where prevalences reach up to 75% [15,25,27,28]. However, when interpreting these data, it is important to consider that our study only included patients who had completed their surgery and chemotherapy treatment at least 12 months earlier. This criterion may have allowed for better recovery and adaptation, resulting in a lower prevalence of sexual dysfunction. The other studies do not specify this criterion, which suggests that they may have included more recent patients, with less recovery time and, therefore, a higher prevalence of sexual dysfunction [15,25,27,28].
Similar to what has been reported internationally, in our study, patients who underwent a mastectomy were more likely to experience sexual dysfunction compared to those who underwent breast-conserving surgery [10,15,25,29]. This is probably due to the impact of mastectomy on body image and the perception of sexuality. In contrast, conservative surgeries carry a lower risk of sexual dysfunction, although they are not free of impairments.
In addition, the results show that patients over the age of 50 have lower scores on the Female Sexual Function Index questionnaire compared to those under the age of 50, highlighting the impact of aging on sexual function. These findings underscore the importance of considering menopause-related hormonal changes as a relevant factor when assessing quality of life and sexual well-being in breast cancer survivors.
Radiotherapy treatment is part of the therapeutic plan for patients undergoing conservative surgery. It is also part of the therapeutic plan for patients undergoing total mastectomy with high-risk characteristics (including those in whom neoadjuvant chemotherapy was chosen instead of primary surgery). Although radiotherapy can cause locoregional sequelae (including persistent mastalgia, discomfort in the arms and shoulders, together with loss of flexibility, lymphedema [30,31,32], and any of these is associated with a reduction in sexual function), in our study it did not show a significant impact on the sexual function of breast cancer survivors.
Contrary to what has been reported internationally [3,15,16], the crude analysis showed that patients treated with chemotherapy had a lower prevalence of sexual dysfunction, and this difference was maintained in the adjusted analysis. The study’s selection criteria may explain this discrepancy, as the patients included had completed treatment at least 12 months before the evaluation, which could have allowed for better recovery from the acute side effects of chemotherapy, such as severe fatigue or hormonal changes. Furthermore, the high percentage of women aged 50 or over, many of them probably postmenopausal, in our sample could have reduced the hormonal impact of chemotherapy compared to premenopausal women, thus diminishing its influence on sexual function.
It was not possible to evaluate the impact of hormone therapy on the risk of developing sexual dysfunction, due to the low number of patients with hormone receptor-negative breast cancer. Although a higher prevalence of sexual dysfunction has been reported among patients treated with aromatase inhibitors compared to tamoxifen [18,19,21], in our study, no significant difference was observed between these treatments. However, the addition of a gonadotropin-releasing hormone agonist increased the chance of developing sexual dysfunction up to five times, which is consistent with what has already been reported [33].
Among the strengths of this study, we highlight that it is a prospective observational study that includes a comparison of various surgical modalities, as well as chemotherapy, radiotherapy, and hormone therapy, which provides a comprehensive view of how each treatment affects sexual function. This provides valuable data for improving the quality of care. In addition, patients who had been at least one year post-surgery were included, providing a long-term perspective on the effects of surgical interventions on sensuality and sexual function. Using the Female Sexual Function Index questionnaire, a validated and widely used tool, ensures the reliability and validity of the data collected on sexual dysfunction.
However, the study has some limitations. One of them is that no prior calculation of sample size was made, so we do not know if the comparisons that did not yield statistical significance were due to a lack of power of the test. Likewise, the data on sexual dysfunction is based on self-reported questionnaires, which can introduce reporting biases, as patients may have minimized or exaggerated their sexual problems for various personal or cultural reasons. Although the Female Sexual Function Index questionnaire used has been widely validated in multiple languages and adapted to Spanish, it has not been specifically validated for the Uruguayan population. This could limit the generalizability of the findings, as cultural differences in the perception and expression of sexual function may affect responses. On the other hand, sexual life before breast cancer diagnosis and treatment was not evaluated, so we do not know the impact of diagnosis and treatment on sexuality in the study population. Finally, the study was conducted in two healthcare institutions, which may introduce a representativeness bias when interpreting the results as applicable to the national population. It is possible that the characteristics of the patients and the treatments in these institutions do not fully reflect the realities of other regions of the country. Therefore, evaluating the disease’s characteristics in the rest of the country remains pending for future studies.
Our findings highlight that sexual dysfunction affects 58.3% of breast cancer survivors in our population, as assessed by the Female Sexual Function Index questionnaire, with a score equal to or less than 26.55 considered indicative of sexual dysfunction. This prevalence is in line with international studies, where the reported rates range between 50 and 75% in women with breast cancer [15,25,27,28]. Although sexual dysfunction is a widely recognized problem in this population, our results show that its impact varies according to the treatment modality. The adjusted analysis indicated significant associations between mastectomy and the use of gonadotropin-releasing hormone agonists with a higher prevalence of sexual dysfunction. These differences underscore the importance of personalizing therapeutic strategies, taking into account both oncological objectives and quality of life aspects.
Although this study provides relevant data, any generalization of the results should be interpreted with caution. The fact that the study was conducted in two specific hospitals may limit its applicability to other regions or healthcare contexts. Likewise, the inclusion criteria, which only considered patients who had completed treatment at least 12 months earlier, restrict the extrapolation of the results to other populations. However, these same criteria enable a more precise understanding of the long-term effects of the treatments, which will help guide clinical management in similar contexts.

