Estudios originales
← vista completaPublicado el 6 de agosto de 2025 | http://doi.org/10.5867/medwave.2025.07.3088
Tiempo desde la llegada a Chile hasta el diagnóstico de tuberculosis en migrantes atendidos en centros de atención primaria de dos comunas de la Región Metropolitana
Time from arrival in Chile to tuberculosis diagnosis in migrants treated at primary care centers in two Metropolitan Region municipalities, Chile
Abstract
Introduction In Chile, the number of migrants affected by tuberculosis has experienced a significant increase from 7.1% in 2014 to 29.7% in 2023, ranking as the first group at risk. The objective was to estimate the time to diagnosis of tuberculosis from arrival in Chile in a series of migrants undergoing treatment between January 2021 and March 2022.
Methods We analyzed a cohort of migrants over 18 years of age with a diagnosis of tuberculosis treated in the communes of Recoleta and Independencia. Those who agreed to participate and signed the informed consent form were included. Cases with non-tuberculous mycobacteria and residents outside the Metropolitan Region were excluded. Sociodemographic, clinical, and arrival dates, as well as symptoms and diagnoses, were recorded. Proportional hazards models in STATA v.18 were used to analyze times according to independent variables. A p value < 0.05 was considered significant.
Results The median time to diagnosis was 93.5 months, varying by subgroup. The recent migration subgroup without Chilean documentation had a hazard ratio of 13.1, which indicates that, at any time after arrival, these individuals have a 13-fold increased risk of tuberculosis diagnosis compared to the reference subgroup (traditional migration with Chilean identity documents). This hazard ratio is reduced by 2.4 times when these types of migrants have documentation from Chile (95% confidence interval: 1.2 to 4.5).
Conclusions There is a wide range of time from arrival in Chile to the diagnosis of tuberculosis. Factors such as the type of migration and the type of identity document have an impact on the development of this disease. It is necessary to expedite the legal administrative process for migrants and implement timely screening policies, along with follow-up and improved access to healthcare, to reduce exposure and risk of tuberculosis.
Main messages
- Tuberculosis is an infectious disease, responsible for the death of 1.6 million people in 2022. The WHO considers migrants as a key population in the follow-up of tuberculosis in its latent and active manifestations.
- This is the first study in Chile that analyzes the time since migrants arrive in the country and are diagnosed with tuberculosis.
- Limitations were the size and restriction of the sample to only two areas of Santiago during the COVID-19 pandemic, which restricts the extrapolation of the results.
Introduction
Migration is a growing phenomenon that influences the health and development of both migrant and host communities, although it generally does not pose a significant threat to the health of this population [1]. However, some subgroups of migrants are particularly vulnerable to infectious diseases, including tuberculosis [2].
This is an infectious disease caused by Mycobacterium tuberculosis, which is transmitted by coughing, talking, or sneezing. Although a vaccine against Bacillus Calmette-Guérin (BCG) exists, which prevents severe primary forms in newborns and infants, its efficacy in preventing pulmonary tuberculosis is very limited [3]. According to the World Health Organization (WHO), in 2022, 10.6 million people developed the disease, and 1.6 million lost their lives due to it [4].
WHO considers migrants as a key population in the follow-up of both latent and active tuberculosis [4]. It is estimated that migrants are about 10 times more at risk of developing tuberculosis, especially within the first few years after arrival in the host country [5].
The incidence rate of tuberculosis in the country of origin is the most crucial predictor of tuberculosis incidence in migrants, according to some authors [2,6]. However, factors such as social determinants in the country of origin, conditions of the migration journey, discrimination, adversity in the receiving country, and multiple trips for various reasons often significantly increase the risk of tuberculosis during the migration process [2,5,7].
On the other hand, Chile has established itself as one of the main destinations for intraregional south-south migration, driven by its economic and political stability. The proportion of migrants in the country increased from 3.5% in 2015 to 9.6% in 2023 [8]. Since 2019, an increase in inflows through unauthorized border crossings has also been observed [9]. Of the total migrant population, 56.8% reside in the Metropolitan Region and 38% come from Venezuela [8]. This growth has posed significant challenges in terms of social integration and access to public services, leading to substantial delays in migration regularization processes that can negatively impact timely access to healthcare [10]. In this context, tuberculosis represents an emerging problem, as conditions of social vulnerability and administrative barriers may delay timely diagnosis and treatment, favoring the transmission and development of active forms of this disease [5,6].
According to the National Tuberculosis Program, cases in the migrant population increased from 7.1 in 2014 [11] to 29.7% by 2023, becoming the first group at risk, above people living with HIV and elderly people [12]. Moreover, at the time of writing this paper, there are no published studies that account for when migrants become ill with tuberculosis in the country. In this context, the objective of this study was to estimate the time from arrival in the national territory to the diagnosis of tuberculosis. To this end, two specific objectives were established:
-
To characterize the migrant population diagnosed with tuberculosis.
-
To identify the factors associated with the time of presentation of tuberculosis.
Methods
Study design and sample
The present study was based on a retrospective observational cohort. We analyzed a cohort of migrant patients aged 18 years or older, with tuberculosis diagnosis confirmed by smear microscopy, culture and/or Xpert rapid molecular test (PCR) for the first time in Chile, and who were seen between January 2021 and March 2022 in the primary healthcare centers of the Recoleta and Independencia communes, Metropolitan Region, Chile. Both urban communes are home to a significant number of immigrant population [8].
The inclusion criteria were all patients born in a country other than Chile, regardless of their migratory status, who agreed to participate voluntarily after being informed and signing the informed consent form. Cases diagnosed with nontuberculous mycobacteria and residents outside the Metropolitan Region at the time of the study were excluded.
Data collection
All participants completed a structured survey. In addition to the questions systematized by the National Tuberculosis Program, the survey collected sociodemographic information, morbid antecedents, date of arrival in Chile, onset of symptoms, and diagnosis of tuberculosis. Clinical records were reviewed to verify each of these dates. The survey lasted an average of 15 minutes and was conducted during supervised treatment at the healthcare centers.
Variables
The dependent variable was the time from arrival in Chile to the diagnosis of tuberculosis, measured in months. The independent variables analyzed were age, sex, type of migration, overcrowding, healthcare provision, comorbidities, vulnerable migratory path, perception of stressful life events, type of identity document, history of diabetes mellitus, and consumption of alcohol, tobacco, and drugs. Age was collected in years completed at the time of diagnosis. The variable country of origin was regrouped into the variable “type of migration”, which was divided into two categories. While the traditional migration category consisted of foreigners born in the bordering countries of Peru, Bolivia, and Argentina, the recent migration comprised people born in Venezuela, Haiti, the Dominican Republic, and Colombia.
Overcrowding was defined as the presence of three or more people per bedroom. Health insurance was classified as a public health system (Fondo Nacional de Salud, FONASA), and without health insurance. As for the type of document, Chilean documentation or another type of document, other than the national one, was considered. The vulnerable migratory path was considered when the travel itinerary, from departure to arrival in Chile, was marked by difficult and/or risky conditions for their well-being. Perception of stressful life was defined according to the self-perception of constant stress before being diagnosed with tuberculosis, and was assessed with the following question:
Do you consider that you led a life of constant stress before being diagnosed with tuberculosis?
Statistical analysis
Descriptive statistics for categorical variables were summarized as frequencies and percentages, while continuous variables were summarized as mean, median, standard deviation, and interquartile range. Time-to-diagnosis curves were estimated using the Kaplan-Meier estimator, and comparisons of these estimates were performed using the Log-Rank test. To evaluate the strength of association, a parametric proportional hazards model based on the exponential distribution, expressed as a Hazard Ratio, was performed. Variables that showed a p value < 0.05 in the univariate analysis were entered into the multivariate model. Consequently, a p value < 0.05 was considered a significant statistical association. The analyses were performed with statistical analysis software (STATA v.18).
Ethics
An unnamed coding variable (alphanumeric code) was generated to protect the confidentiality and privacy of the participants. Informed consent was requested from all participants, according to a research protocol approved by the Ethics Committee of the Faculty of Medicine of the University of Chile (File minutes: No. 059) and of the Servicio de Salud Metropolitano Norte (Letter number 075/2021).
Results
Time was studied in 58 cases that agreed to answer the survey. These correspond to 67.4% of the universe of migrant patients with tuberculosis treated in these communes. Of those who consented, 58.6% were treated in the commune of Recoleta. The sample consisted of 56.9% women (n = 33), 75.9% individuals between 18 and 44 years of age (n = 44), and 67.2% (n = 39) who had completed secondary school or less. A total of 84.5% (n = 49) had public health insurance, and 86.2% (n = 50) had Chilean documentation. The countries of origin were Peru, 55.2% (n = 32), followed by Venezuela, 20.7% (n = 12) (Table 1).
In the univariate analysis, the significant variables with p < 0.05 were type of documentation (p = 0.001), type of migration (p = 0.00), HIV diagnosis (p = 0.02), and vulnerable travel route (p = 0.05). In the multivariate analysis, an identity document other than Chile and recent migration were predictors of time to tuberculosis diagnosis (Table 2).
Observing the strong statistical association between the variables' type of document' and 'type of migration' in both univariate and multivariate analyses, the interaction between these two variables was evaluated. The hazard ratio was 3.8 (95% confidence interval: 0.68 to 21.5), with a p value of 0.128, suggesting a significant interaction. Four subgroups were generated from this result:
-
Traditional migration with a Chilean identity document.
-
Traditional migration without a Chilean identity document.
-
Recent migration and Chilean identity documents.
-
Recent migration without a Chilean identity document.
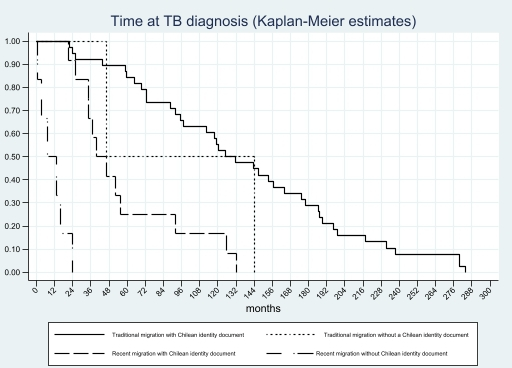
The median time to tuberculosis diagnosis was 93.5 months, with significant variations according to the migration subgroup. The subgroup of persons who considered recent migration without Chilean documentation (subgroup 4) presented the lowest median of 10.1 months. This same subgroup presented a hazard ratio of 13.1, indicating that the diagnosis of tuberculosis was 13.1 times more likely at any time during the observed period, compared to the reference subgroup (traditional migration and Chilean documentation, subgroup 1). This difference was statistically significant (95% confidence interval: 5.5 to 30.9). Next, the recent migration and Chilean documentation subgroup presented a hazard ratio of 2.4 (95% confidence interval: 1.2 to 4.5) (Table 3).
Figure 1 represents Table 3, illustrating the Kaplan-Meier survival curves for the time to tuberculosis diagnosis across subgroups. Subgroup 1, which had Chilean identity documents and came from countries of traditional migration, was considered a reference. The subgroup with recent migration and no documentation was diagnosed with tuberculosis within 24 months after arrival.
Time from arrival of migrants in Chile to tuberculosis diagnosis (Kaplan-Meier estimates).
Discussion
This study estimated the time elapsed from arrival in Chile to diagnosis of tuberculosis in a series of migrants receiving treatment. The results show a wide variability in this interval, from less than one month to 280 months. A greater vulnerability is evident among those who have migrated recently and do not have Chilean documentation. In particular, this subgroup presented a significantly higher hazard ratio of being diagnosed with tuberculosis compared to the reference subgroup.
The wide range of time observed between arrival in Chile and diagnosis of tuberculosis could be linked to the complex migration process, access to healthcare, social integration, and acculturation [6,10]. When comparing our time estimates with previous studies, high heterogeneity is observed. Some report medians of five to nine years [5,13,14], while another found a value similar to that found in our study [15]. These differences are due to several factors: national policies for the detection of tuberculosis in migrants, the existence or lack of follow-up, screening and treatment programs for latent tuberculosis in migrants from countries with a high tuberculosis burden [13,16], the sociodemographic and migratory characteristics of the populations studied (risk profile, country of origin, type of migrant and socioeconomic level), the conditions of the healthcare systems in the countries where the studies were conducted, which differ substantially from the Chilean context, and the healthcare system conditions in the countries where the studies were conducted.
The subgroup of recent migrants without a Chilean identity document had a hazard ratio of 13.1, indicating that at any time after their arrival, these persons have a risk of tuberculosis diagnosis 13 times higher than that observed in the reference subgroup (traditional migration and Chilean identity document). Several studies show a high proportion of tuberculosis cases diagnosed soon after arrival in the destination country. One study reported that 64% of cases were diagnosed in the first two years of residence, mainly in migrants from countries with a high burden of tuberculosis [16]. Another study found that 50% of diagnosed migrants developed the disease within five years in the receiving country, and noted that the risk remained higher compared to the native population [17].
However, the risk of tuberculosis in migrants is not limited to the first years after arrival, but rather is maintained over time, albeit to a lesser extent. This was evident in the “traditional migration” subgroup, which was composed mainly of migrants from Peru (80%) and Bolivia (17.5%), both countries with rates exceeding 100 cases per 100 000 inhabitants [4]. Along these lines, several studies have shown that migrants from high-burden countries maintain an elevated risk of developing tuberculosis, even a decade after entering the country [6,18]. Another study reported that migrants from Latin America and the Caribbean had tuberculosis a median of nine years after arrival [14]. Our findings are consistent with these studies, since 41% of the tuberculosis cases in the sample corresponded to persons who had been residing in Chile for 10 years or more at the time of diagnosis.
In this context, when migrants have tuberculosis, it is usually attributed to reactivation of a previously acquired latent infection [6]. In the case of newly arrived migrants, this reactivation may be triggered by adverse conditions associated with the migration process, such as stress, overcrowding, and limited access to healthcare, among others [5]. In contrast, among those who have resided in the country for several years, reactivation of latent infection may be related to the onset of chronic diseases, such as diabetes, or immunosuppressive treatments that weaken the immune response [6,19,20].
However, Mycobacterium tuberculosis infection may have been acquired at different times: in the country of origin, during the migratory journey, or after arrival, and even as a result of reinfection when returning temporarily to their country for vacation or other reasons [5,21]. Some migrants may arrive with active tuberculosis, while the vast majority arrive with a latent infection that may remain asymptomatic for years.
Unlike other studies that evaluated risk according to country of origin [22], our study used the variable “type of migration,” constructed based on the country of origin of the migrants. In this regard, the category of “recent migration” was mainly composed of people from Venezuela (66.7%) and, to a lesser extent, from Haiti (16.6%). These countries are affected by humanitarian crises, political instability, and deterioration of their health systems, including limitations in tuberculosis control [4,23]. In addition, the tightening of migration policies in Chile in response to the increase in migratory flows in recent years has led thousands of people (mainly Venezuelans) to enter through unauthorized border crossings, especially on the northern border with Bolivia. This has meant that many of them have been in an irregular migratory situation since their arrival [24].
In 2021, Chile implemented a new Migration Law [25]; however, the regularization process for individuals who entered the country irregularly remains limited. Currently, 75% of foreigners in irregular migratory status are of Venezuelan nationality [8]. This situation has been aggravated by the effects of the COVID-19 pandemic, delays, and barriers in regularization procedures, which have further increased the social and health vulnerability of these people [24].
Migrants with Chilean identity documents have access to social, health, educational, and formal employment services, while those without such documentation face multiple forms of exclusion. These people often reside in informal and precarious environments, with exploitative working conditions, no social protection, and difficulties in accessing even decent housing [26]. This precarious situation translates into conditions of poverty, overcrowding, and material deprivation, which are well-documented determinants of the risk of developing tuberculosis [2,10,27].
Chile’s lack of documentation could also be linked to the absence of health insurance and, therefore, to non-enrollment in the health system. In our study, 15.5% of participants had no health insurance, a figure similar to that reported in the National Socioeconomic Characterization Survey (CASEN) [28] and lower than the rate reported in another study [29]. Although this was not an independent risk factor in our study, it may reflect both the lack of information among the migrant population and the persistence of cultural and organizational barriers in healthcare services, which hinder effective access to care [30]. Although the National Tuberculosis Program guarantees free and universal care regardless of health insurance and migratory status, these results suggest that this guarantee has not been sufficient to ensure active strategies for screening, case follow-up, and contact investigation in the migrant population, both inside and outside healthcare facilities.
Among the main limitations of the study were the sample size and the use of convenience sampling. Only 6.9% declined to participate, while 25.6% could not be contacted due to mobility and capacity restrictions at the care centers during the COVID-19 pandemic. Another limitation was the possible recall bias regarding the date of arrival in the country. However, since migration is a significant event in the lives of migrants and their families, it is usually remembered accurately. In addition, the study was conducted only in two communes in the northern sector of the urban radius of Santiago (capital city), excluding other metropolitan areas or regions of the country. This limits the representativeness and generalization of the results to contexts with different characteristics.
Conclusions
This study estimated that the time to diagnosis of tuberculosis in migrants in Chile was highly variable, ranging from one month to 280 months (median 93.5 months or 7.8 years). The recent migration subgroup without a Chilean identity document at any time during the observed period was more likely to be diagnosed with tuberculosis compared to the traditional migration subgroup with a Chilean document (hazard ratio: 13.1; 95% confidence interval: 5.5 to 30.9), followed by the recent migration group with documentation (hazard ratio: 2.4; 95% confidence interval: 1.2 to 4.5). These findings, which had not been previously reported in the country, suggest substantial inequalities in access to timely diagnosis associated with both the type of migration and migratory status.
In this context, it is necessary to strengthen and redesign early detection, follow-up, and treatment programs aimed at migrants. These programs should consider the impact that delayed diagnosis has on the progression of the disease and the transmission chain. It is also essential to ensure the application of the current legal framework, which guarantees access to medical care regardless of migratory status, safeguarding compliance by all healthcare officials. Finally, the results reinforce the importance of establishing clearer, more accessible, and expeditious administrative migration processes that facilitate the regularization of those who arrive in the country, mostly young and healthy people [8]. In line with these needs, implementing policies for timely screening, follow-up, and improved access to care can significantly contribute to controlling tuberculosis in Chile.
Future studies should delve deeper into the characterization and specific barriers faced by migrants in accessing diagnosis and treatment in Chile, as well as make their care trajectories visible through a qualitative approach. Similarly, it is essential to advance in the genomic characterization of the strains present in this population. This is aimed at the early detection of possible non-endemic variants, which could alter the epidemiological profile of tuberculosis in the country.

