Estudios originales
← vista completaPublicado el 1 de octubre de 2025 | http://doi.org/10.5867/medwave.2025.09.3106
Análisis de la lista de espera quirúrgica de patologías no cubiertas por las Garantías Explícitas en Salud en ortopedia y traumatología en Chile
Analysis of the surgical waiting list for conditions not covered by the Explicit Health Guarantees in orthopedics and traumatology in Chile
Abstract
Introduction Surgical waiting lists for conditions not covered by the Explicit Health Guarantees represent unmet needs and structural gaps within the Chilean public health system. The field of orthopedics and traumatology accounts for a high volume of pending procedures, with total knee arthroplasty being the most frequently delayed. The coexistence of deferrable pathologies not formally recorded, combined with the low efficiency in the use of operating rooms, aggravates this problem. This study aims to characterize the surgical waiting list for conditions not covered by the Explicit Health Guarantees in Chile between 2022 and 2024, with a focus on orthopedics and traumatology. Additionally, we identify the most delayed procedures, the most affected health services, and the current capacity for resolution.
Methods A descriptive observational study based on official data requested from the Ministry of Health through transparency and public records, including the Department of Health Statistics and Information and the National Health Fund. Surgical procedures awaiting treatment were analyzed by specialty, region, establishment, sex, and age for the period from 2022 to 2024.
Results Orthopedics and traumatology were the specialties with the highest number of pending procedures (22 to 24% of the total). Knee arthroplasty consistently ranked first, with over 20 000 cases annually. The O'Higgins Health Service had the highest burden. In 2022, the rate of arthroplasties performed on patients covered by the National Health Fund was four times lower than on patients covered by Social Security Health Institutions. No region achieved a surgical volume sufficient to reduce the waiting list significantly.
Conclusions The problem of waiting lists in orthopedics is mainly due to organizational shortcomings. Creating the role of trauma emergency ward, optimizing the use of wards, and creating outpatient surgical units are short- and medium-term measures to reverse this trend.
Main messages
- The surgical waiting list outside the Explicit Health Guarantees in orthopedics and traumatology represents a serious gap in access and efficiency in the Chilean public health system. Highlighting this reality is essential to move toward a more comprehensive and humanized care model that promotes the autonomy and well-being of those affected.
- This study provides an opportunity to gauge the magnitude of the problem, characterize its regional distribution, and indirectly evaluate the public system’s capacity to resolve it.
- One limitation of our study is that it used administrative records, so it does not include clinical variables or individual patient prioritization.
Introduction
The increasing number of patients on surgical waiting lists is a tangible expression of the gap between the population’s health needs and the healthcare system’s capacity to address them. When access to care does not depend exclusively on direct payment (as in publicly or mixed-financed healthcare systems), the emergence of waiting lists is inevitable [1]. However, their magnitude and persistence reflect structural deficiencies, including problems of organization, management, and suboptimal use of resources, affecting even countries with globally recognized healthcare systems such as the United Kingdom [2].
In Chile, as in other countries, surgical waiting lists have been a chronic problem in the healthcare system. One solution implemented at the beginning of the 21st century was the creation of the Explicit Health Guarantees regime. This ensures, by law, timely, quality, and financially protected access to care for specific pathologies within a set time frame [3]. Currently, the Explicit Health Guarantees include 87 pathologies, 11 of which require surgical resolution. While this policy has significantly improved access for the included pathologies, it has also had an unintended effect: pathologies not covered by this system have longer waiting times, deepening inequalities in the system [4].
Despite the multiple strategies implemented in recent decades for pathologies not covered by the Explicit Health Guarantees (such as prioritizing cases based on clinical criteria or purchasing surgical services in the private sector), indicators show slight structural variation in the volume of patients waiting [5]. This situation is particularly acute in specialties such as orthopedics and traumatology, where waiting times are long worldwide and negatively affect patients' quality of life and functionality [6,7]. Highlighting this reality is essential to move toward a more comprehensive and humanized model of care that promotes the autonomy and well-being of those affected [6,8].
A critical dimension of the problem lies in the efficiency of the system, particularly regarding the availability and use of operating rooms [9]. In the Chilean public system, operating rooms are distributed among gynecological-obstetric, emergency, elective, and undifferentiated surgery [10]. Emergency operating rooms treat life-threatening conditions or complications in hospitalized patients, generally excluding orthopedic and traumatic cases, except in severe situations such as open fractures. Elective operating rooms, usually intended for scheduled surgeries, are also used in orthopedics to treat deferred emergencies such as closed fractures and tendon ruptures, generating an "invisible" waiting list [11,12].
One dimension of the science of quality in healthcare is to identify gaps that make it possible to diagnose the current situation and define improvement strategies [13]. Analyzing the magnitude and distribution of the waiting list in orthopedics and traumatology makes it possible to detect bottlenecks, optimize the allocation of human resources, reformulate specialized medical training programs, and even redesign the national surgical network.
The objective of this study is to characterize the evolution of the surgical waiting list for pathologies not included in the Explicit Health Guarantees in Chile between 2022 and 2024, with special emphasis on orthopedics and traumatology. The aim is to identify the procedures with the highest waiting list numbers, the healthcare services with the highest care burden, and the current capacity of the system. The hypothesis is that orthopedics and traumatology account for the highest proportion of cases on the waiting list, with knee arthroplasty being the most delayed procedure nationwide.
Methods
Descriptive observational study. A request was made via the Ministry of Health’s transparency portal for a list of surgical procedures awaiting treatment that were not included in the Explicit Health Guarantees for July 2022, 2023, and 2024. In addition to the surgery code, information was requested on the specialty associated with the service, the healthcare service, and the facility responsible for providing it. Procedures corresponding to surgical waiting lists covered by the Explicit Health Guarantees and those with incomplete data were excluded.
A descriptive analysis of the database was performed, without applying inferential methods, since the universe of available cases was used. Biases are discussed along with limitations. However, the results aim to provide a general characterization of the public health system’s waiting list behavior. In the temporal analysis, the internal trend of each procedure or specialty was identified independently, coding it as “+” if the number of cases increased progressively (2022 < 2023 < 2024), “–” if it showed a sustained decrease (2022 > 2023 > 2024), and “0” if no precise linear sequence was observed. This classification does not reflect the magnitude of the volume or its relative position with respect to other specialties; instead, it is based on the temporal behavior of the specialty or procedure.
For the territorial analysis by health service (total, orthopedics and traumatology, and knee arthroplasty), a ranking of specialties was established according to the volume of procedures awaiting treatment, assigning orthopedics and traumatology a relative position (RANK OT) among all specialties, and also identifying the three with the highest number of procedures per territory (positions 1, 2, and 3). Likewise, a ranking of healthcare services was constructed based on the total volume of procedures awaiting treatment in each year and category analyzed, identifying as “median” the service that occupies the central position within the ranking, thus allowing for a representative comparison of the system.
In addition, the percentage frequency representing the total number of orthopedic and traumatology procedures was estimated in relation to the total number of surgeries not covered by the Explicit Health Guarantees registered in each healthcare service and year.
The number of beneficiaries per health service was obtained from the official website of the National Health Fund [14]. This information was used to calculate the number of procedures awaiting treatment per 100 000 beneficiaries, both for the total and for the categories of orthopedics and traumatology and knee arthroplasty.
To estimate the system’s “response capacity,” the percentage of knee arthroplasties on the waiting list that were actually performed during 2022 was used as an indicator, based on the hospital discharge database of the Department of Health Statistics and Information. Both procedures performed in public and private institutions were considered, also differentiating National Health Fund beneficiaries by provider. This analysis was performed by region and linked to waiting list data for July 2023.
The data were processed and organized using Microsoft Excel, and descriptive analyses were performed using Stata software version 17.
Results
Waiting list not included in Explicit Health Guarantees: 2022 to 2024
During the period from 2022 to 2024, there was an overall increase in the number of surgical procedures on the waiting list not covered by Explicit Health Guarantees, with 332 523 cases registered in 2022, 315,059 in 2023, and 373 907 in 2024. The specialty with the highest waiting volume in the three years was orthopedics and traumatology, representing 23.6% in 2022, 23.9% in 2023, and 22.4% in 2024 (Table 1) (Figure 1). The three specialties with the highest waiting list burden remained constant during the period: orthopedics and traumatology, gastrointestinal surgery, and dermatology.
Total number of procedures on the waiting list by healthcare service and corresponding volume for the specialty of orthopedics and traumatology in 2024.
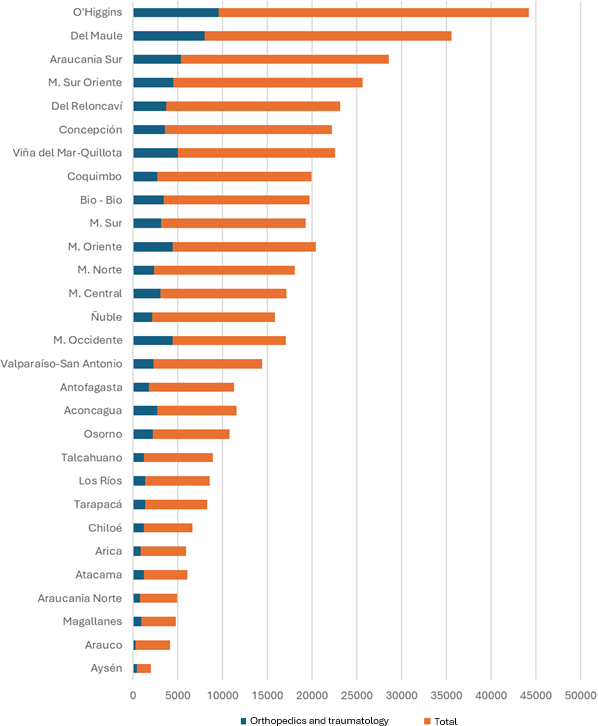
Source: Prepared by the authors based on the study results.
In 2024, three health services exceeded 25 000 procedures on the waiting list: O'Higgins, Maule, and Metropolitano Sur Oriente, with orthopedics and traumatology being the leading specialties on the waiting list in all of them (Table 2). The Metropolitano Occidente healthcare service had the highest proportion of waiting times attributed to this specialty (35%), despite having a hospital that only treats pathologies in this specialty (Instituto Traumatológico Dr. Teodoro Gebauer). In 19 of the country’s 29 (66%) health services, orthopedics and traumatology were the specialties with the highest number of pending procedures.
Concerning individual procedures, knee arthroplasty topped the list for all three years, being the only procedure with more than 20 000 cases per year. In 2024, it was followed by cholecystectomy, third molar extraction, and inguinal hernia repair. Although this order remained unchanged in 2022 and 2024, in 2023, inguinal hernia rose to third place, displacing tooth extraction (Table 3) (Appendix 1).
It is important to note that both cholecystectomy and hip arthroplasty are among the ten most frequent procedures, despite being included in the Explicit Health Guarantees regime with age restrictions. In the case of cholecystectomy, patients under 35 or over 49 are excluded, while in hip arthroplasty, those under 65 are not covered, which explains their accumulation on the non-priority waiting list.
Waiting list for orthopedics and traumatology: 2022 to 2024
Knee arthroplasty accounted for approximately one in four procedures on the waiting list not covered by the Explicit Health Guarantees for surgery during the period, reaching 28.6% in 2024. This was followed by hip arthroplasty in people under 65, hallux valgus correction, rotator cuff repair, and meniscectomy. Together, these procedures accounted for a volume comparable to that of knee arthroplasty (Table 4) (Appendix 2).
In terms of territorial distribution, the Metropolitano Norte healthcare service occupied the central position when ranking services according to the total number of procedures awaiting treatment in 2024, with 2322 cases (2.6%). The O'Higgins (10.7%) and Maule (8.9%) services had the highest waiting volumes. Seven healthcare services exceeded 4000 pending procedures in 2024: O'Higgins, Maule, Araucania Sur, Viña del Mar-Quillota, Metropolitano Sur Oriente, Metropolitano Oriente, and Metropolitano Occidente. In contrast, only five services exceeded that threshold in 2022 and 2023 (Table 5) (Appendix 3).
In proportional terms, orthopedics and traumatology accounted for 22% of all procedures on the waiting list in 2024. The highest percentage was observed in the Metropolitano Occidente health services (35%), Aconcagua (32%), Viña del Mar-Quillota (28%), Metropolitano Oriente (28%), and O'Higgins (28%) (Table 2). This is also reflected in the incidence rates adjusted for beneficiaries of the National Health Fund, where the Aconcagua, O'Higgins, and Osorno health services stand out for their high relative burden of orthopedics and traumatology (Figure 2).
Incidence of procedures on the waiting list for orthopedics and traumatology per 100 000 FONASA beneficiaries, by healthcare service (2024).
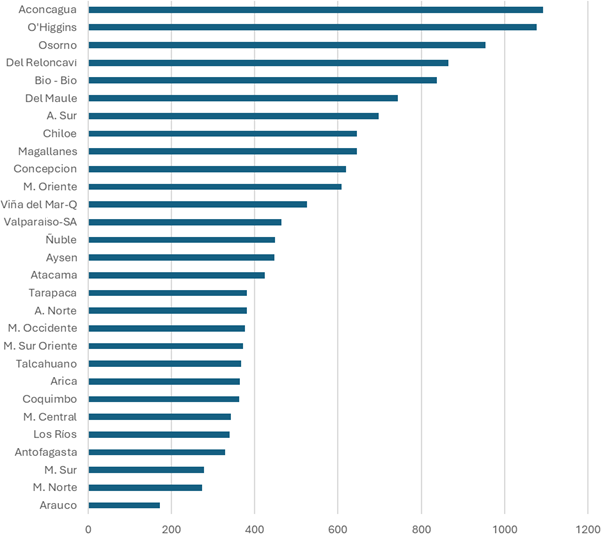
Source: Prepared by the authors based on the study results.
Waiting list for knee arthroplasty: 2022 to 2024
In 2024, the Valparaiso-San Antonio health service had 697 knee arthroplasties on the waiting list (2.9%), placing it in the middle of the distribution when ranking health services from highest to lowest by total number of knee arthroplasties on the waiting list. That year, three health services exceeded 2000 cases: O'Higgins (n = 2626), Maule (n = 2326), and Viña del Mar-Quillota (n = 2202). In previous years, only the O'Higgins service exceeded this threshold, showing an accumulation of cases in more health services (Table 6) (Appendix 4).
In terms of incidence adjusted for the beneficiary population of the National Health Fund aged over 50 and 60, Aconcagua and O'Higgins had the highest rates, exceeding 1000 cases per 100 000 beneficiaries, indicating high pressure on healthcare services. The healthcare services of Osorno, Tarapaca, and Chiloe also exhibited high rates, although to a lesser extent (Figure 3).
Incidence of patients on the waiting list for knee arthroplasty in 2024, by age group and health service (≥ 50 and ≥ 60 years per 100 000 FONASA beneficiaries).
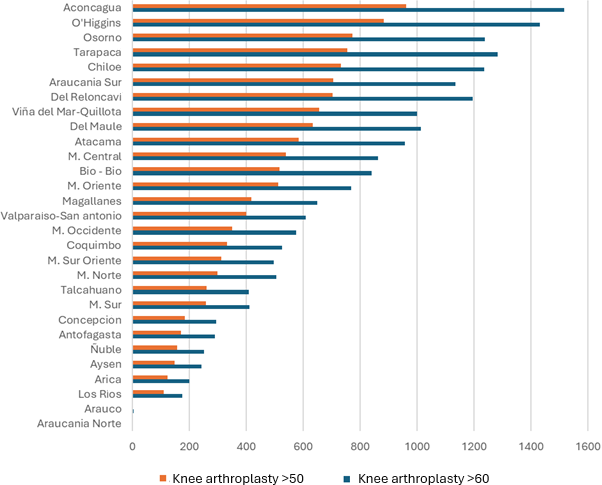
Source: Prepared by the authors based on the study results.
Capacity for knee arthroplasty based on surgical volume in 2022
During 2022, 1690 knee arthroplasties were performed in the population over 60 years of age affiliated with Health Insurance Institutions (ISAPRE, private insurance) (n = 312 468), equivalent to an incidence of 540 per 100 000 beneficiaries. In the National Health Fund, 3967 procedures were performed in a population of 3 363 353 people, with an incidence of 117 per 100 000. These figures reveal a marked inequality between the two subsystems.
No region managed to completely resolve its waiting list, even considering procedures performed in the public and private systems. The Los Rios Region had the highest proportion of public resolution (40%) and total resolution (42.1%). It was followed by Magallanes, with 30% coverage in the public system and 46.8% in total. The Valparaiso Region, despite having one of the longest waiting lists (n = 2,637), resolved only 1.7% through the public system. Adding the interventions performed in private institutions by beneficiaries of the National Health Fund, coverage increased to 14%. Antofagasta was the region with the highest total resolution capacity (76.6%), although only 15.2% of its cases were resolved in the public system, reflecting a strong dependence on the private sector (Table 7).
Discussion
Main findings
This study confirms that orthopedics and traumatology is the specialty with the highest number of surgical procedures not covered by the Explicit Health Guarantees awaiting treatment in the Chilean public system. This trend has remained constant over the three years studied. Within this specialty, knee arthroplasty stands out as the procedure with the highest number of pending cases, being the only one to exceed 20 000 cases.
Additionally, it is worth noting that among the ten most common surgical conditions not included in the Explicit Health Guarantees, two of them are included in this coverage, but with age restrictions. These are hip arthroplasty in people over 65 and cholecystectomy in adults between 35 and 49 years of age. This situation highlights the need to review and update the clinical guidelines of the Explicit Health Guarantees regime, which have remained unchanged for over 15 years [15,16]. For example, hospital discharge data show that more than 40% of hip replacements are performed on patients under 65 years of age [17]. In this economically active group, functional disability has a significant economic impact, both in terms of sick leave and loss of productivity [18]. In line with this problem, a Swedish study estimated that patients waiting for arthroplasty accumulated average costs of USD 860 during the 5.5 months before surgery, of which 60% corresponded to loss of productivity and 30% to home care [19].
Economic burden and territorial variability
The study conducted by Cartes et al. [20] estimated that in 2023, the cost associated with the surgical waiting list would reach US$800 million. The analysis identified that the relative weight assigned to each Diagnosis-Related Group, the poverty index, age, specialty, and type of facility accounted for nearly 50% of these costs. Regarding geographical distribution, it was observed that the O'Higgins and Maule healthcare services accounted for the highest amounts. In addition, it was observed that the five services with the highest number of orthopedic and traumatology procedures awaiting treatment per 100 000 beneficiaries are concentrated in the Valparaíso and Los Lagos regions. This situation contrasts with the logic of greater backwardness in the extreme regions, where historically there are fewer specialists available. This suggests that territorial distribution does not always follow usual patterns, requiring a focused review.
The efficiency of elective surgery wards as a cause of waiting lists not covered by explicit health guarantees
Identifying bottlenecks in the healthcare system is key to improving the resolution of surgical waiting lists. As previously documented, these lists are largely a consequence of the inefficient use of operating rooms for elective surgeries. For this reason, operating room management must play a central role in the design of public policies [12]. In Chile, considering only the number of patients waiting, the magnitude of the problem may seem insurmountable. In 2024, there were 332 523 people on the waiting list, a figure comparable to the total number of surgeries performed in 2018 (n = 297 692) and 2019 (n = 416 339). However, when the analysis focuses on the efficiency of elective operating rooms, the picture changes. In those years, this volume of interventions was achieved by performing only two surgeries per day per elective operating room. A simple projection indicates that if the frequency increases to three procedures per day, it would be possible to clear the waiting list in two years, without the need to build new hospitals. This estimate had already been proposed in previous studies [12], including the 2020 report by the National Productivity Commission. That document proposed specific recommendations for optimizing the use of operating rooms [21]. However, its implementation has been limited, contributing to the gaps highlighted in our study.
Consequently, the efficient use of operating rooms represents one of the main challenges in reducing the waiting list of surgeries not included in the Explicit Health Guarantees. Although this problem affects all specialties, it cannot be addressed uniformly. Increasing the frequency of short procedures, such as arthroscopies, is not the same as increasing the frequency of complex surgeries such as arthroplasties, neurosurgeries, or cardiovascular interventions, which require more surgical time and greater resources [22]. Therefore, the debate must move from a focus on the number of patients to one that prioritizes operational optimization, addressing factors such as low daily productivity, delays in the start of the surgical day, and turnaround times between procedures. All of these are elements that directly restrict the public system’s capacity to deliver results [9].
Another factor that limits surgical efficiency in the public system is the high frequency of operating room cancellations. A cancellation rate of less than 5% is considered efficient [9]. However, figures above this threshold have been reported in Chile between 2019 and 2022 [11]. The most common causes are related to the patient, including failure to fast, incomplete tests, or difficulties in establishing contact with them [11,12,23]. Other frequent causes of suspension include union-related issues and failures in the support unit, with the latter highlighting the management of the sterilization unit within each institution [11]. The high frequency of surgical suspensions increases system costs, undermines patient confidence, and leads to additional health expenses for both users and institutions [24,25].
The particular case of orthopedics and traumatology: the “hidden” surgical waiting list
In the specific case of orthopedics and traumatology, the volume of surgical waiting lists not covered by Explicit Health Guarantees is aggravated by the existence of a “hidden surgical waiting list.” This list is made up of patients hospitalized for fractures or other acute traumatic injuries who, due to their “deferrable urgent” condition, are not treated in the emergency room and require procedures that occupy operating rooms intended for elective surgeries. Unlike specialties such as gastrointestinal surgery, which have exclusive operating rooms for emergencies, these orthopedic pathologies must compete for space in the operating room with scheduled surgeries, directly affecting the availability to resolve pathologies on the surgical waiting list that are not included in the Explicit Health Guarantees. An immediate and cost-effective strategy to mitigate this burden would be to set up trauma emergency operating rooms, operating at least 12 hours a day, seven days a week, which would relieve congestion in elective operating rooms and allow them to be used exclusively for resolving the Explicit Health Guarantees lists and those not covered by them.
Proposals to reduce surgical waiting lists outside the explicit health guarantees
One of the main strategies adopted by the public system to reduce surgical waiting lists is to establish surgical resolution agreements with the private sector [26]. This public-private relationship has partially alleviated the accumulated demand. However, it also highlights the marked differences in operating room management between the two sectors [27]. While in the private system, surgical procedures are remunerated according to performance and productivity, in the public system, rigid structures predominate, with limited operating hours (generally between 8:00 a.m. and 5:00 p.m.) and low operational efficiency, reflected in an average of only two surgeries per day during working hours [11].
Another critical factor restricting surgical access in the public system is the limited availability of hospital beds, which has been the most sensitive issue during the COVID-19 pandemic [28,29]. Some institutions have responded to this challenge with outpatient or short-stay surgery programs, using anesthesia recovery units as a temporary alternative to hospitalization [29,30,31,32]. In orthopedics and traumatology, this problem is particularly acute in the case of fractures, especially hip fractures, whose delayed surgical resolution is associated with prolonged hospital stays and intensive use of beds [33]. This limits the availability of beds to resolve surgical waiting list pathologies. Therefore, the implementation of trauma emergency wards would relieve congestion in elective wards, reduce hospitalization times, and improve bed utilization, optimizing overall surgical flow.
In the medium term, a key structural strategy involves creating public centers dedicated exclusively to outpatient surgery or short-stay hospitalization, allowing for more efficient handling of the growing demand in different specialties [34]. International experience, particularly in the United States, has shown that ambulatory surgical centers are a cost-effective alternative to traditional hospitals [35]. Since the 1990s, these centers have grown steadily, driven by the need to improve efficiency [36,37]. They are now a key pillar of the US healthcare system, enabling shorter surgeries, lower costs, and shorter recovery times [38,39], covering trauma procedures, including hip and knee arthroplasty [35,40]. In Chile, this model already exists in the private sector, especially in plastic surgery, where the absence of National Health Fund codes has promoted the bundling of procedures in outpatient centers with more competitive costs [41]. In the public sector, attempts to replicate this strategy have been sporadic and have generally been implemented within the hospitals themselves, without creating independent structures [42]. Just as primary emergency services have succeeded in relieving pressure on hospital emergency rooms, outpatient surgery centers could play a similar role concerning operating rooms, reducing pressure on traditional infrastructure and improving the overall efficiency of the system [43].
The study by Lenz et al. [44] revealed that between 2010 and 2019, public spending on health increased considerably, but without a proportional increase in healthcare provision. In fact, spending efficiency fell by up to 47% and labor productivity declined by more than 30%. This stagnation can be explained, in part, by the fact that the growth strategy has focused on increasing the number of workers, without achieving substantive improvements in the system’s capacity to deliver results [44]. Given this scenario, a comprehensive and phased strategy is required. In the short term, public-private collaboration must be maintained, and after-hours surgical programs must be strengthened, in combination with improvements in the efficient use of hospital operating rooms. In the medium term, it is essential to implement operating rooms exclusively for non-urgent trauma cases. Finally, in the long term, progress must be made in creating public outpatient surgery centers, inspired by successful international experiences. These centers, with a focus on efficiency, time culture, and safety, could transform the current surgical model, improve productivity, and ensure more equitable and timely access to surgeries with greater functional and social impact, such as arthroplasty.
The specific case of knee arthroplasty
Access to knee arthroplasty is a critical equity issue in the Chilean healthcare system. According to the classification of the Organization for Economic Cooperation and Development (OECD), this procedure is a relevant indicator of surgical access and impact on quality of life [45]. In 2019, the ratio between the number of arthroplasties performed on beneficiaries of the Social Security Health Institutions system and the National Health Fund was 2.8:1 [17]. However, our study reveals that this ratio has increased to 4.6:1. This difference reflects a deepening inequality that cannot be explained by epidemiological differences, but rather by structural and management barriers. Furthermore, the current rate of arthroplasty procedures is insufficient to meet the accumulated demand in all regions of the country. Access to these procedures could be radically improved if deferrable emergencies did not occupy elective operating rooms and if there were centers for major outpatient surgery [46]. Ensuring timely access to this procedure meets clinical criteria rather than principles of equity, productivity, and sustainability of the system.
Limitations and strengths
Our study is based on administrative records from the Ministry of Health, which precludes the incorporation of individual clinical variables, such as comorbidities or prioritization criteria, that are essential for assessing the healthcare burden. In addition, the data correspond to annual snapshots (July 2022, 2023, and 2024), which limits the possibility of analyzing intra-annual fluctuations.
It was also not possible to directly link hospital discharges with waiting list data, as they come from different sources rather than having standard identifiers. Finally, although the rate of procedures per beneficiary of the National Health Fund was calculated, structural variables such as the availability of operating rooms, surgical equipment, or the budget per service were not considered, which could significantly influence the observed resolution capacity.
Despite these limitations, this study enables us to gauge the magnitude of the problem, characterize its regional distribution, and indirectly assess the public system’s capacity to address it. In this context, there is a need for future research and public policies to focus on reforming the surgical model, promoting the more efficient use of operating rooms, establishing units exclusively for non-urgent trauma cases, and creating public outpatient surgery centers. Only through a phased approach, with a structural and long-term vision, will it be possible to guarantee more equitable, timely, and sustainable access to surgery, especially for procedures with high functional and social impact, such as knee arthroplasty.
Conclusions
This research allowed us to characterize the evolution of the surgical waiting list not covered by the Explicit Health Guarantees regime in Chile between 2022 and 2024, with a special emphasis on the specialty of orthopedics and traumatology. It was confirmed that this area accounts for the highest number of procedures on the waiting list within the public system, consistently representing more than 30% of the total during the three-year period analyzed. In particular, knee arthroplasty stood out as the procedure with the highest cumulative volume, exceeding 20 000 cases in 2024.
At the territorial level, the O'Higgins and Maule healthcare services had the highest volumes of pending trauma surgeries, both in absolute terms and adjusted by beneficiaries. Likewise, the ranking of specialties on hold showed significant differences between territories, although orthopedics and traumatology remained among the top positions in most of them.

